-
Original Article01-28-2021
Risk Factors for Postpartum Hemorrhage and its Severe Forms with Blood Loss Evaluated Objectively – A Prospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):113-118
Abstract
Original ArticleRisk Factors for Postpartum Hemorrhage and its Severe Forms with Blood Loss Evaluated Objectively – A Prospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):113-118
Views293See moreAbstract
Objective
To identify risk factors related to postpartum hemorrhage (PPH) and severe PPH with blood loss quantified objectively.
Methods
This is a complementary analysis of a prospective cohort study that included pregnant women delivering vaginally. The total blood loss was obtained through the sum of the volume collected from the drape with the weight of gauzes, compresses and pads used by women within 2 hours. Exploratory data analysis was performed to assess mean, standard deviation (SD), frequency, percentage and percentiles. The risk factors for postpartum bleeding were evaluated using linear and logistic regression.
Results
We included 270 women. Themean blood loss at 120 minutes was 427.49 mL (±335.57 mL). Thirty-one percent (84 women) bled > 500mL and 8.2% (22 women) bled > 1,000 mL within 2 hours. Episiotomy, longer second stage of labor and forceps delivery were related to blood loss > 500mL within 2 hours, in the univariate analysis. In the multivariate analysis, only forceps remained associated with bleeding > 500 mL within 2 hours (odds ratio [OR] = 9.5 [2.85-31.53]). Previous anemia and episiotomy were also related to blood loss > 1,000mL.
Conclusion
Prolonged second stage of labor, forceps and episiotomy are related to increased incidence of PPH, and should be used as an alert for the delivery assistants for early recognition and prompt treatment for PPH.
-
Original Article01-28-2021
Follicular Fluid from Infertile Women with Mild Endometriosis Impairs In Vitro Bovine Embryo Development: Potential Role of Oxidative Stress
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):119-125
Abstract
Original ArticleFollicular Fluid from Infertile Women with Mild Endometriosis Impairs In Vitro Bovine Embryo Development: Potential Role of Oxidative Stress
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):119-125
Views172See moreAbstract
Objective
To investigate whether follicular fluid (FF) from infertile women with mild endometriosis (ME) alters in vitro bovine embryo development, and whether the antioxidants N-acetyl-cysteine (NAC) and/or L-carnitine (LC) could prevent such damages.
Methods
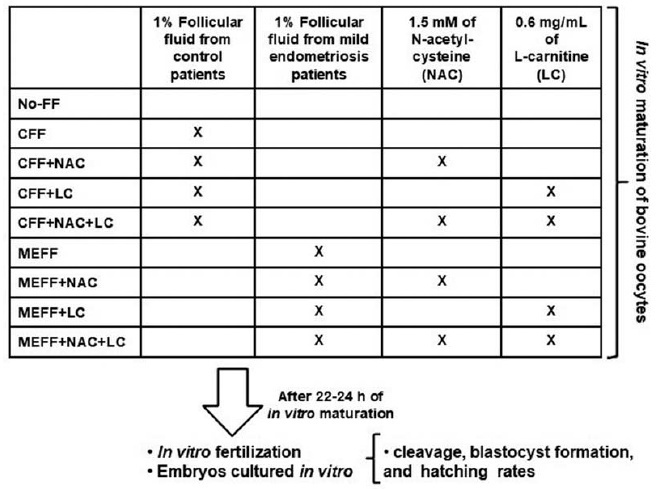
Follicular fluid was obtained from infertile women (11 with ME and 11 control). Bovine oocytes were matured in vitro divided in: No-FF, with 1% of FF from control women (CFF) or ME women (MEFF); with 1.5mM NAC (CFF + NAC, MEFF + NAC), with 0.6mg/mL LC (CFF + LC, MEFF + LC), or both antioxidants (CFF + NAC + LC, MEFF + NAC + LC). After in vitro fertilization, in vitro embryo culture was performed for 9 days.
Results
A total of 883 presumptive zygotes were cultured in vitro. No differences were observed in cleavage rate (p = 0.5376) and blastocyst formation rate (p = 0.4249). However, the MEFF group (12.5%) had lower hatching rate than the No-FF (42.1%, p = 0.029) and CFF (42.9%, p = 0.036) groups. Addition of antioxidants in the group with CFF did not alter hatching rate (p ≥ 0.56), and in groups with MEFF, just NAC increased the hatching rate [(MEFF: 12.5% versus MEFF + NAC: 44.4% (p = 0.02); vs MEFF + LC: 18.8% (p = 0.79); versus MEFF + NAC + LC: 30.8% (p = 0.22)].
Conclusion
Therefore, FF from infertile women with ME added to medium of in vitro maturation of bovine oocytes impairs hatching rate, and NAC prevented these damages, suggesting involvement of oxidative stress in worst of oocyte and embryo quality of women with ME.
-
Original Article01-19-2021
Gestational Risk as a Determining Factor for Cesarean Section according to the Robson Classification Groups
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):84-90
Abstract
Original ArticleGestational Risk as a Determining Factor for Cesarean Section according to the Robson Classification Groups
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):84-90
Views247See moreAbstract
Objective
To analyze and compare the frequency of cesarean sections and vaginal deliveries through the Robson Classification in pregnant women attended at a tertiary hospital in two different periods.
Methods
Cross-sectional, retrospective study of birth records, comprising 4,010 women, conducted from January 2014 to December 2015 in the only public regional referral hospital for the care of high- risk pregnancies, located in Southern Brazil.
Results
The overall cesarean section rate reached 57.5% and the main indication was the existence of a previous uterine cesarean scar. Based on the Robson Classification, groups 5 (26.3%) and 10 (17.4%) were the most frequent ones. In 2015, there was a significant increase in the frequency of groups 1 and 3 (p < 0.001), when compared with the previous year, resulting in an increase in the number of vaginal deliveries (p < 0.0001) and a reduction in cesarean section rates.
Conclusion
The Robson Classification proved to be a useful tool to identify the profile of parturients and the groups with the highest risk of cesarean sections in different periods in the same service. Thus, it allowsmonitoring in a dynamic way the indications and delivery routes and developing actions to reduce cesarean rates according to the characteristics of the pregnant women attended.
-
Original Article01-19-2021
Factors Associated with Exclusive Breastfeeding in a Maternity Hospital Reference in Humanized Birth
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):91-96
Abstract
Original ArticleFactors Associated with Exclusive Breastfeeding in a Maternity Hospital Reference in Humanized Birth
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):91-96
Views181See moreAbstract
Objective
To analyze the factors associated with the prevalence of exclusive breastfeeding (EBF) for up to six months in mother/infant binomials cared for at a usual-risk maternity hospital.
Methods
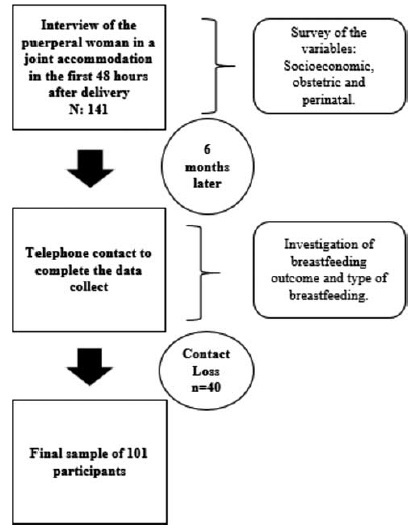
The present is a descriptive, longitudinal, prospective, quantitative study. Socioeconomic, obstetric and perinatal variables from 101 mother/infant binomials in a Public Maternity Hospital in the city of Curitiba, state of Paraná, Brazil, were investigated during hospitalization after delivery and 6 months after birth. For the statistical analysis, the Chi-squared test was used. The variables that showed values of p < 0.25 for the Chi-squared test were also submitted to an odds ratio (OR) analysis.
Results
The prevalence (42.6%) of EBF was observed. Most women (93.1%) had had more than 6 prenatal consultations, and the variables maternity leave and support to breastfeeding were associated with EBF. Support to breastfeeding by professionals and family members increased 4-fold the chance of maintenance of EBF (OR = 0.232; 95% confidence intercal [95%CI]: 0.079 to 0.679; p = 0.008). Cracked nipples were the biggest obstacle to breastfeeding, and low milk production was the main responsible factor for weaning.
Conclusion
The encouragement of breastfeeding and the mother’s stay for a longer period with the child contributed to the maintenance of EBF until the sixth month of life of the infant.
-
Original Article01-19-2021
Temporal Trend of Near Miss and its Regional Variations in Brazil from 2010 to 2018
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):97-106
Abstract
Original ArticleTemporal Trend of Near Miss and its Regional Variations in Brazil from 2010 to 2018
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):97-106
Views229See moreAbstract
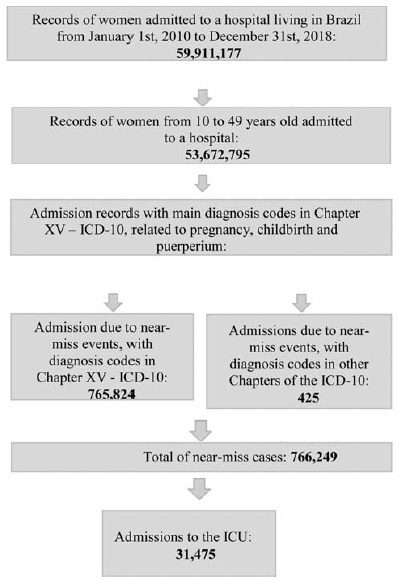
Cases of maternal near miss are those in which women survive severe maternal complications during pregnancy or the puerperium. This ecological study aimed to identify the temporal trend of near-miss cases in different regions of Brazil between 2010 and 2018, using data fromtheHospital Information System(HIS) of theUnified BrazilianHealth System (SUS, in the Portuguese acronym). Hospital admission records of women between 10 and 49 years old with diagnosis included in the 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) and codes indicating nearmiss events were selected. From 20,891,040 admissions due to obstetric causes, 766,249 (3.66%) near-miss cases were identified, and 31,475 women needed admission to the intensive care unit (ICU). The cases were found to be more predominant in black women over 35 years old from the North and Northeast regions. There was a trend of increase in near-miss rates of ~ 13.5% a year during the period of the study. The trend presented a different behavior depending on the level of development of the region studied. The main causes of near miss were preeclampsia (47%), hemorrhage (24%), and sepsis (18%).
-
Original Article01-19-2021
Gestational Diabetes Mellitus and Obesity are Related to Persistent Hyperglycemia in the Postpartum Period
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):107-112
Abstract
Original ArticleGestational Diabetes Mellitus and Obesity are Related to Persistent Hyperglycemia in the Postpartum Period
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):107-112
Views250See moreAbstract
Objective
To evaluate the obstetric and sociodemographic characteristics of gestational diabetic women who maintained hyperglycemia in the postpartum period (6-12 weeks postpartum).
Methods
This is a longitudinal cohort study with women who have had gestational diabetes and/or macrosomic children between March 1st, 2016 and March 1st, 2017. Between 6 and 12 weeks after birth, women who had gestational diabetes collected fasting glycemia, glucose tolerance test, and glycated hemoglobin results. The data were collected from medical records and during an interview in the first postpartum consultation. A statistical analysis was performed using frequency, percentage, Chi- Squared test, Fisher exact test, Mann-Whitney test, and multivariate Poisson regression. The significance level adopted for the statistical tests was 5%.
Results
One hundred and twenty-two women were included. Most of the women were younger than 35 years old (70.5%), white, multiparous, and with no history of gestational diabetes. Thirteen percent of the participants developed persistent hyperglycemia. A univariate analysis showed that maternal age above 35 years, being overweight, having grade 1 obesity and weight gain under 5 kg was related to the persistence of hyperglycemia in the postpartum period.
Conclusion
Maternal age above 35 years, obesity and overweight, and the diagnosis of gestational diabetes in the first trimester of pregnancy are associated with hyperglycemia during the postpartum period.
-
Original Article01-19-2021
Switching of Hormone Therapies in Breast Cancer Women
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):185-189
Abstract
Original ArticleSwitching of Hormone Therapies in Breast Cancer Women
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):185-189
Views100See moreAbstract
Objective
The objective of the present study was to analyze the reasons that led to hormone therapies (HTs) regimen changes in women with breast cancer.
Methods
This was a retrospective cross-sectional study from a single-institution Brazilian cancer center with patient records diagnosed with breast cancer between January 2012 and January 2017.
Results
From 1,555 women who were in treatment with HT, 213 (13.7%) women had HT switched, either tamoxifen to anastrozole or vice-versa. Most women included in the present study who switched HT were > 50 years old, postmenopausal, Caucasian, and had at least one comorbidity. From the group with therapy change, ‘disease progression’ was reason of change in 124 (58.2%) cases, and in 65 (30.5%) patients, ‘presence of side effects’ was the reason. From those women who suffered with side effects, 24 (36.9%) had comorbidities.
Conclusion
The present study demonstrated a low rate of HT switch of tamoxifen to anastrozole. Among the reasons for changing therapy, the most common was disease progression, which includes cancer recurrence, metastasis or increased tumor. Side effects were second; furthermore, age and comorbidities are risk factors for side effects.
-
Original Article01-19-2021
The Effectiveness of Melissa Officinalis L. versus Citalopram on Quality of Life of Menopausal Women with Sleep Disorder: A Randomized Double-Blind Clinical Trial
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):126-130
Abstract
Original ArticleThe Effectiveness of Melissa Officinalis L. versus Citalopram on Quality of Life of Menopausal Women with Sleep Disorder: A Randomized Double-Blind Clinical Trial
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):126-130
Views297See moreAbstract
Objective
The present study aimed to assess the effect of Melissa Officinalis L. (a combination of lemon balm with fennel fruit extract) compared with citalopram and placebo on the quality of life of postmenopausal women with sleep disturbance.
Methods
The present study is a randomized, double-blind, placebo clinical trial among 60 postmenopausal women with sleep disturbance who were referred to a university hospital from 2017 to 2019. The participants were randomized to receive M. Officinalis L. (500 mg daily), citalopram (30 mg) or placebo once daily for 8 weeks. The Menopause-Specific Quality of Life (MENQOL) questionnaire was self-completed by each participant at baseline and after 8 weeks of the intervention and was compared between groups.
Results
The mean for all MENQOL domain scores were significantly improved in the M. Officinalis L. group compared with citalopram and placebo (p < 0.001). The mean ± standard deviation (SD) after 8 weeks in the M. Officinalis L., citalopram and placebo groups was 2.2 ± 0.84 versus 0.56 ± 0.58 versus 0.36 ± 0.55 in the vasomotor (p < 0.001), 1.02 ± 0.6 versus 0.28 ± 0.2 versus 0.17 ± 0.1 in the psychomotor-social (p < 0.001), 0.76 ± 0.4 versus 0.25 ± 0.1 versus 0.11 ± 0.1 in the physical and 2.3 ± 1.0 versus 0.35 ± 0.5 versus 0.41 ± 0.5 in the sexual domain, respectively.
Conclusions
The results revealed that M. Officinalis L. may be recommended for improving the quality of life of menopausal women with sleep disturbance. Trial registration The present study was registered by the name “Comparison of the efficacy of citalopram and compound of Asperugo procumbens and foeniculum vulgare in treatment of menopausal disorders” with the code in the Iranian Registry of Clinical Trials (IRCT).


