Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):444-449
To identify maternal factors associated with the presence of low birth weight in term neonates.
Matched hospital-based case-controlled study performed in a high complexity institution located in the city of Neiva, Colombia. The study included women with term gestation and singleton live fetuses. Patients with prior diseases, coming from other regions, with pregnancy resulting from assisted reproduction, or with a diagnosis of fetal abnormality or aneuploidy were excluded. Low birth weight was the dependent variable, and the independent variables that were analyzed were maternal sociodemographic and clinical characteristics. Adjusted and non-adjusted odds ratios (aOR and OR) together with the 95% confidence intervals (95% CI) were reported.
The study included 270 participants (90 cases and 180 controls). Controlling for maternal age, educational level, socioeconomic and civil status, social security and the presence of maternal disease during gestation, it was found that weight gain (aOR 0.77, 95% CI 0.70-0.85) and the absence of prenatal care (aOR 8.20, 95% CI 3.22-20.87) were among the factors associated with low birth weight.
The absence of weight gain and of prenatal care are factors associated with the presence of low birth weight in term neonates and should be considered in clinical practice.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):450-457
The present study aims to investigate the association between caspase-8 (CASP8) (rs13416436 and rs2037815) and Fas cell surface death receptor (FAS) (rs3740286 and rs4064) polymorphisms with endometriosis in Brazilian women.
In the present case-control study, 45 women with a diagnosis of endometriosis and 78 normal healthy women as a control group were included. The genotyping was determined by real-time polymerase chain reaction (PCR) with Taqman hydrolysis probes (Thermo Fisher Scientific, Darmstadt, Germany). Genotypic and allelic frequencies were analyzed using Chi-squared (χ2) test. In order to determine the inheritance models and haplotypes ,SNPStats (Institut Català d’Oncologia, Barcelona, Spain) was used. Levels of 5% (p = 0.05) were considered statistically significant.
No significant difference was observed in genotypic or allelic frequencies between control and endometriosis groups for rs13416436 and rs2037815 (CASP8 gene). On the other hand, a significant difference between rs3740286 and rs4064 (FAS gene) was found. Regarding polymorphisms in the FAS gene, a statistically significant differencewas found in co-dominant and dominantmodels. Only the haplotype containing the rs3740286A and rs4064G alleles in the FAS gene were statistically significant.
The polymorphisms in the CASP8 gene were not associated with endometriosis. The results indicate an association between FAS gene polymorphisms and the risk of developing endometriosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):458-464
Intraoperative frozen section (IFS) is a valuable resource, and its use in gynecological pathology has not been sufficiently emphasized. The main goal of the present study is to evaluate the reliability and agreement rates between IFS and the final paraffin section (PS) and determine how reliable IFS is.
A retrospective study of all IFSs performed on uterine tumors and suspicious adnexal masses between January 2012 and December 2016 (excluding metastases) at the department of obstetrics and gynecology of the Centro Hospitalar Tondela Viseu. Frozen versus permanent section diagnosis were compared regarding the histologic type of the tumor, and the depth of myometrial invasion.
A total of 286 cases were eligible for the present study, including 102 (35.7%) IFSs of uterine tumors, and 184 (64.3%) IFSs of ovarian tumors. The overall rate of deferred cases was 5.2% (15/286). The accuracy of the diagnosis in cases of endometrial carcinoma was 96.25% (77/80). Among the ovarian tumors, misdiagnoses occurred in 2 cases (1.1%), corresponding to a borderline tumor (serous type) and a clear cell intracystic adenocarcinoma.
The IFS analysis plays an important role in selected situations and is associated to a high sensitivity and specificity in cases of ovarian and endometrial tumors. Its high accuracy is almost universally associated with the possibility of obtaining an optimal surgical treatment at the time of the first surgical approach.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):465-470
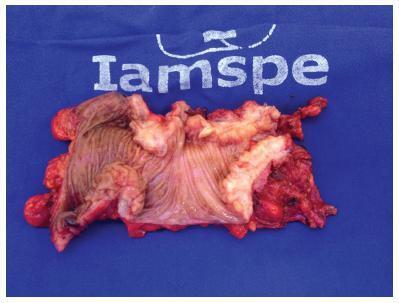
To describe and evaluate the use of a simple, low-cost, and reproducible simulator for teaching the repair of obstetric anal sphincter injuries (OASIS).
Twenty resident doctors in obstetrics and gynecology and four obstetricians participated in the simulation. A fourth-degree tear model was created using lowcost materials (condom simulating the rectal mucosa, cotton tissue simulating the internal anal sphincter, and bovine meat simulating the external anal sphincter). The simulator was initially assembled with the aid of anatomical photos to study the anatomy and meaning of each component of the model. The laceration was created and repaired, using end-to-end or overlapping application techniques.
The model cost less than R$ 10.00 and was assembled without difficulty, which improved the knowledge of the participants of anatomy and physiology. The sutures of the layers (rectal mucosa, internal sphincter, and external sphincter) were performed in keeping with the surgical technique. All participants were satisfied with the simulation and felt it improved their knowledge and skills. Between 3 and 6 months after the training, 7 participants witnessed severe lacerations in their practice and reported that the simulation was useful for surgical correction.
The use of a simulator for repair training in OASIS is affordable (low-cost and easy to perform). The simulation seems to improve the knowledge and surgical skills necessary to repair severe lacerations. Further systematized studies should be performed for evaluation.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):379-383
Perineal trauma is a negative outcome during labor, and until now it is unclear if the maternal position during the second stage of labormay influence the risk of acquiring severe perineal trauma. We have aimed to determine the prevalence of perineal trauma and its risk factors in a low-risk maternity with a high incidence of upright position during the second stage of labor.
A retrospective cohort study of 264 singleton pregnancies during labor was performed at a low-risk pregnancymaternity during a 6-month period. Perineal trauma was classified according to the Royal College of Obstetricians and Gynecologists (RCOG), and perineal integrity was divided into three categories: no tears; first/ second-degree tears + episiotomy; and third and fourth-degree tears. A multinomial analysis was performed to search for associated factors of perineal trauma.
From a total of 264 women, there were 2 cases (0.75%) of severe perineal trauma, which occurred in nulliparous women younger than 25 years old. Approximately 46% (121) of the women had no tears, and 7.95% (21) performed mediolateral episiotomies. Perineal trauma was not associated with maternal position (p = 0.285), health professional (obstetricians or midwives; p = 0.231), newborns with 4 kilos or more (p = 0.672), and labor analgesia (p = 0.319). The multinomial analysis showed that white and nulliparous presented, respectively, 3.90 and 2.90 times more risk of presenting perineal tears.
The incidence of severe perineal trauma was low. The prevalence of upright position during the second stage of labor was 42%. White and nulliparous women were more prone to develop perineal tears.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):384-389
The main objective of this study was to examine the diagnostic performance of the first-trimester combined test for aneuploidies in unselected pregnancies from Rio de Janeiro and compare it with the examples available in the literature.
We investigated 3,639 patients submitted to aneuploidy screening from February 2009 to September 2015. The examination is composed of the Fetal Medicine Foundation risk evaluation based on nuchal translucency evaluation, mother’s age, presence of risk factors, presence of the nasal bone and Doppler of the ductus venous in addition to biochemical analysis of pregnancy-associated plasma protein A (PAPP-A) and beta-human chorionic gonadotropin (β-hCG) markers. The cut-off point for high risk for aneuploidies was defined as greater than 1:100, with intermediate risk defined between 1:100 and 1:1,000, and low risk defined as less than 1:1,000. The variable aneuploidy was considered as a result not only of trisomy of chromosome 21 but also trisomy of chromosomes 13 and 18.
Excluding the losses, the results of 2,748 patients were analyzed. The firsttrimester combined test achieved 71.4% sensitivity with a 7.4% false-positive (FP) rate, specificity of 92.6%, positive predictive value (PPV) of 6.91% and negative predictive value (NPV) of 99.76%, when the cut-off point considered was greater than 1:1,000. Through a receiving operating characteristics (ROC) curve, the cut-off point that maximized the sensitivity and specificity for the diagnosis of aneuploidies was defined as 1:1,860. When we adjusted the false-positive (FP) rate to 5%, the detection rate for this analysis is 72.7%, with a cut-off point of 1:610.
The combined test of aneuploidy screening showed a detection rate inferior to those described in the literature for a higher FP rate.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):390-396
To outline the demographic and clinical characteristics of patients with deep intestinal endometriosis submitted to surgical treatment at a tertiary referral center with a multidisciplinary team, and correlate those characteristics with the surgical procedures performed and operative complications.
A prospective cohort from February 2012 to November 2016 of 32 women with deep intestinal endometriosis operations. The variables analyzed were: age; obesity; preoperative symptoms (dysmenorrhea, dyspareunia, acyclic pain, dyschezia, infertility, urinary symptoms, constipation and intestinal bleeding); previous surgery for endometriosis; Enzian classification; size of the intestinal lesion; and surgical complications.
Themean age was 37.75 (±5.72) years. A total of 7 patients (22%) had a prior history of endometriosis. The mean of the largest diameter of the intestinal lesions identified intraoperatively was of 28.12 mm (±14.29 mm). In the Enzian classification, there was a predominance of lesions of the rectum and sigmoid, comprising 30 cases (94%). There were no statistically significant associations between the predictor variables and the outcome complications, even after the multiple logistic regression analysis. Regarding the size of the lesion, there was also no significant correlation with the outcome complications (p = 0.18; 95% confidence interval [95%CI]:0.94-1.44); however, there was a positive association between grade 3 of the Enzia classification and the more extensive surgical techniques: segmental intestinal resection and rectosigmoidectomy, with a prevalence risk of 4.4 (p < 0.001; 95%CI:1.60-12.09).
The studied sample consisted of highly symptomatic women. A high prevalence of deep infiltrative endometriosis lesions was found located in the rectum and sigmoid region, and their size correlated directly with the extent of the surgical resection performed.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):397-402
To analyze the perioperative results and safety of performing gynecological surgeries using robot-assisted laparoscopy during implementation of the technique in a community hospital over a 6-year period.
This was a retrospective observational study in which the medical records of 274 patients who underwent robotic surgery from September 2008 to December 2014 were analyzed. We evaluated age, body mass index (BMI), diagnosis, procedures performed, American Society of Anesthesiologists (ASA) classification, the presence of a proctor (experienced surgeon with at least 20 robotic cases), operative time, transfusion rate, perioperative complications, conversion rate, length of stay, referral to the intensive care unit (ICU), and mortality. We compared transfusion rate, perioperative complications and conversion rate between procedures performed by experienced and beginner robotic surgeons assisted by an experienced proctor.
During the observed period, 3 experienced robotic surgeons performed 187 surgeries,while 87 surgeries were performedby 20 less experienced teams, always with the assistance of a proctor. The median patient age was 38 years, and the median BMI was 23.3 kg/m2. The most frequent diagnosis was endometriosis (57%) and the great majority of the patients were classified as ASA I or ASA II (99.6%). The median operative time was 225 minutes, and the median length of stay was 2 days. We observed a 5.8% transfusion rate, 0.8% rate of perioperative complications, 1.1% conversion rate to laparoscopy or laparotomy, no patients referred to ICU, and no deaths. There were no differences in transfusion, complications and conversion rates between experienced robotic surgeons and beginner robotic surgeons assisted by an experienced proctor.
In our casuistic, robot-assisted laparoscopy demonstrated to be a safe technique for gynecological surgeries, and the presence of an experienced proctor was considered a highlight in the safety model adopted for the introduction of the robotic gynecological surgery in a high-volume hospital and, mainly, for its extension among several surgical teams, assuring patient safety.