-
Original Article04-14-2023
Nonpharmacological Methods to Reduce Pain During Active Labor in A Real-life Setting
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):03-10
Abstract
Original ArticleNonpharmacological Methods to Reduce Pain During Active Labor in A Real-life Setting
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):03-10
Views255See moreAbstract
Objective
To evaluate the association between pain intensity in the active phase of the first stage of labor with the use or not of nonpharmacological methods for pain relief in a real-life scenario.
Methods
This was an observational cross-sectional study. The variables analyzed were obtained by a questionnaire with the mothers (up to 48 hours postpartum) to investigate the intensity of pain during labor using the visual analog scale (VAS). The nonpharmacological pain relief methods routinely used in obstetric practice were evaluated by consulting medical records. The patients were separated into two groups: Group I – patients who did not use nonpharmacological methods for pain relief and Group II –patients who used these methods.
Results
A total of 439 women who underwent vaginal delivery were included; 386 (87.9%) used at least 1 nonpharmacological method and 53 (12.1%) did not. The women who did not use nonpharmacological methods had significantly lower gestational age (37.2 versus 39.6 weeks, p < 0.001) and shorter duration of labor (24 versus 114 min, p < 0.001) than those who used the methods. There was no statistically significant difference in the pain scale score using the VAS between the group that used nonpharmacological methods and the group that did not (median 10 [minimum 2– maximum 10] versus 10 [minimum 6–maximum 10] p = 0.334).
Conclusion
In a real-life setting, there was no difference in labor pain intensity between the patients who used nonpharmacological methods and those who did not use them during the active phase of labor.
-
Original Article04-14-2023
Cervical Cancer Screening with DNA-HPV Testing and Precancerous Lesions Detection: A Brazilian Population-based Demonstration Study
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):21-30
Abstract
Original ArticleCervical Cancer Screening with DNA-HPV Testing and Precancerous Lesions Detection: A Brazilian Population-based Demonstration Study
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):21-30
Views272See moreAbstract
Objective
To evaluate the rates of precancerous lesions, colposcopy referral, and positive predictive value (PPV) by age groups of a population-based screening with DNA-HPV testing.
Methods
The present demonstration study compared 16,384 HPV tests performed in the first 30 months of the program with 19,992 women tested in the cytology screening. The colposcopy referral rate and PPV for CIN2+ and CIN3+ by age group and screening program were compared. The statistical analysis used the chi-squared test and odds ratio (OR) with 95% confidence interval (95%CI).
Results
The HPV tests were 3.26% positive for HPV16-HPV18 and 9.92% positive for 12 other HPVs with a 3.7 times higher colposcopy referral rate than the cytology program, which had 1.68% abnormalities. Human Papillomavirus testing detected 103 CIN2, 89 CIN3, and one AIS, compared with 24 CIN2 and 54 CIN3 detected by cytology (p < 0.0001). The age group between 25 and 29 years old screened by HPV testing had 2.4 to 3.0 times more positivity, 13.0% colposcopy referral, twice more than women aged 30 to 39 years old (7.7%; p < 0.0001), and detected 20 CIN3 and 3 early-stage cancer versus 9 CIN3 and no cancer by cytology screening (CIN3 OR= 2.10; 95%CI: 0.91 -5.25; p = 0.043). The PPV of colposcopy for CIN2+ ranged from 29.5 to 41.0% in the HPV testing program.
Conclusion
There was a significant increase in detections of cervix precancerous lesions in a short period of screening with HPV testing. In women < 30 years old, the HPV testing exhibited more positivity, high colposcopy referral rate, similar colposcopy PPV to older women, and more detection of HSIL and early-stage cervical cancer.
-
Original Article04-14-2023
Immediate Postpartum Insertion of Copper Intrauterine Device in a Brazilian University Hospital: Expulsion and Continuation Rates
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):31-37
Abstract
Original ArticleImmediate Postpartum Insertion of Copper Intrauterine Device in a Brazilian University Hospital: Expulsion and Continuation Rates
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):31-37
Views224Abstract
Objective
To evaluate the expulsion and continuation rates of the copper intrauterine device (IUD) inserted in the immediate postpartum period in a Brazilian public university hospital.
Materials and Methods
In the present cohort study, we included women who received immediate postpartum IUD at vaginal delivery or cesarean s March 2018 to December 2019. Clinical data and the findings of transvaginal ultrasound (US) scans performed 6-weeks postpartum were collected. The expulsion and continuation rates were assessed 6-months postpartum using data from the electronic medical records or by telephone contact. The primary outcome was the proportion of IUDs expelled at 6 months. For the statistical analysis, we used the Student t-test, the Poisson distribution, and the Chi-squared test.
Results
There were 3,728 births in the period, and 352 IUD insertions were performed, totaling a rate of 9.4%. At 6 weeks postpartum, the IUD was properly positioned in 65.1% of the cases, in 10.8% there was partial expulsion, and in 8.5% it had been completely expelled. At 6 months postpartum, information was obtained from 234 women, 74.4% of whom used IUD, with an overall expulsion rate of 25.6%. The expulsion rate was higher after vaginal delivery when compared with cesarean section (68.4% versus 31.6% respectively; p = 0.031). There were no differences in terms of age, parity, gestational age, final body mass index, and newborn weight.
Conclusion
Despite the low insertion rate of copper IUDs in the postpartum period and a higher expulsion rate, the rate of long-term continuation of intrauterine contraception was high, indicating that it is a useful intervention to prevent unwanted pregnancies and to reduce short-interval birth.
Key-words continuation ratecooper intrauterine deviceexpulsion rateimmediate postpartum insertionpostpartum contraceptionSee more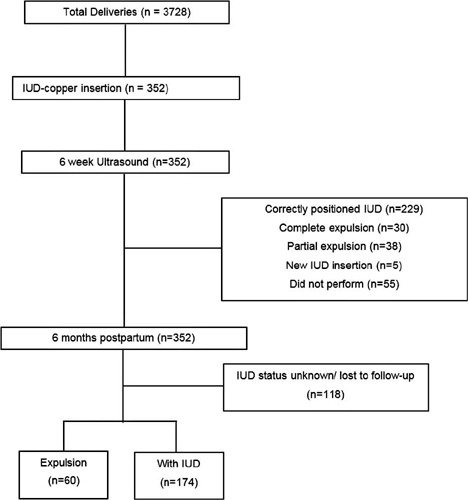
-
Original Article04-14-2023
Predictive Factors of Tolerance in Office Hysteroscopy – a 3-Year Analysis from a Tertiary Center
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):38-42
Abstract
Original ArticlePredictive Factors of Tolerance in Office Hysteroscopy – a 3-Year Analysis from a Tertiary Center
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):38-42
Views156See moreAbstract
Objective
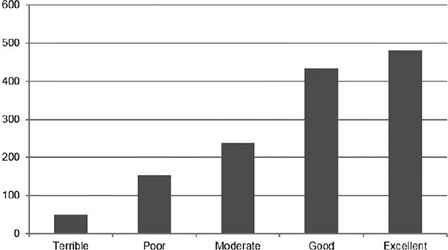
Pain is the primary limitation to performing hysteroscopy. We aimed to evaluate the predictive factors of low tolerance to office hysteroscopic procedures. Methods Retrospective cohort study of the patients who underwent office hysteroscopy from January 2018 to December 2020 at a tertiary care center. Pain tolerance to office-based hysteroscopy was subjectively assessed by the operator as terrible, poor, moderate, good, or excellent. Categorical variables were compared with the use of the Chi-squared test; an independent-samples t-test was conducted to compare continuous variables. Logistic regression was performed to determine the main factors associated with low procedure tolerance.
Results
A total of 1,418 office hysteroscopies were performed. The mean age of the patients was 53 ± 13.8 years; 50.8% of women were menopausal, 17.8% were nulliparous, and 68.7% had a previous vaginal delivery. A total of 42.6% of women were submitted to an operative hysteroscopy. Tolerance was categorized as terrible or poor in 14.9% of hysteroscopies and moderate, good, or excellent in 85.1%. A terrible or poor tolerance was more frequently reported in menopausal women (18.1% vs. 11.7% in premenopausal women, p = 0.001) and women with no previous vaginal delivery (18.8% vs. 12.9% in women with at least one vaginal birth, p = 0.007). Low tolerance led more often to scheduling a second hysteroscopic procedure under anesthesia (56.4% vs. 17.5% in reasonable-to-excellent tolerance, p < 0.0005).
Conclusion
Office hysteroscopy was a well-tolerated procedure in our experience, but menopause and lack of previous vaginal delivery were associated with low tolerance. These patients are more likely to benefit from pain relief measures during office hysteroscopy.
-
Original Article03-24-2022
Randomized Clinical Trial Comparing Quadratus Lumborum Block and Intrathecal Morphine for Postcesarean Analgesia
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1083-1089
Abstract
Original ArticleRandomized Clinical Trial Comparing Quadratus Lumborum Block and Intrathecal Morphine for Postcesarean Analgesia
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1083-1089
Views153See moreAbstract
Objective
To compare the efficacy of quadratus lumborum (QL) block and intrathecal morphine (M) for postcesarean delivery analgesia.
Methods
Thirty-one pregnant women with ≥ 37 weeks of gestation submitted to elective cesarean section were included in the study. They were randomly allocated to either the QL group (12.5 mg 0.5% bupivacaine for spinal anesthesia and 0.3 ml/kg 0.2% bupivacaine for QL block) or the M group (12.5 mg bupivacaine 0.5% and 100 mcg of morphine in spinal anesthesia). The visual analog scale of pain, consumption of morphine and tramadol for pain relief in 48 hours, and side effects were recorded.
Results
Median pain score and/or pain variation were higher in the morphine group than in the QL group (p = 0.02). There was no significant difference in the consumption of morphine or tramadol between groups over time. Side effects such as pruritus, nausea, and vomiting were observed only in the morphine group.
Conclusion
Quadratus lumborum block and intrathecal morphine are effective for analgesia after cesarean section. Patients undergoing QL block had lower postoperative pain scores without the undesirable side effects of opioids such as nausea, vomiting, and pruritus.
-
Original Article03-24-2022
Relationship between the Prenatal Diagnosis of Placenta Acreta Spectrum and Lower Use of Blood Components
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1090-1093
Abstract
Original ArticleRelationship between the Prenatal Diagnosis of Placenta Acreta Spectrum and Lower Use of Blood Components
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1090-1093
Views138See moreAbstract
Objective
To describe the clinical results of patients admitted and managed as cases of placenta accreta spectrum (PAS) at a Central American public hospital and the influence of the prenatal diagnosis on the condition.
Materials and Methods
A retrospective analysis of PAS patients treated at Hospital Bertha Calderón Roque, in Managua, Nicaragua, between June 2017 and September 2021. The diagnostic criteria used were those of the International Federation of Gynecology and Obstetrics (Fédération Internationale de Gynécologie et d'Obstétrique, FIGO, in French). The population was divided into patients with a prenatal ultrasonographic diagnosis of PAS (group 1) and those whose the diagnosis of PAS was established at the time of the caesarean section (group 2).
Results
During the search, we found 103 cases with a histological and/or clinical diagnosis of PAS; groups 1 and 2 were composed of 51 and 52 patients respectively. Regarding the clinical results of both groups, the patients in group 1 presented a lower frequency of transfusions (56.9% versus 96.1% in group 2), use of a lower number of red blood cell units (RBCUs) among those undergoing transfusions (median: 1; interquartile range: [IQR]: 0–4 versus median: 3; [IQR]: 2–4] in group 2), and lower frequency of 4 or more RBCU transfusions (29.4% versus 46.1% in group 2). Group 1 also exhibited a non-significant trend toward a lower volume of blood loss (1,000 mL [IQR]: 750–2,000 mL versus 1,500 mL [IQR]: 1,200–1,800 mL in group 2), and lower requirement of pelvic packing (1.9% versus 7.7% in group 2).
Conclusion
Establishing a prenatal diagnosis of PAS is related to a lower frequency of transfusions. We observed a high frequency of prenatal diagnostic failures of PAS. It is a priority to improve prenatal detection of this disease.
-
Original Article03-24-2022
Perinatal Outcomes in Women with Chronic Kidney Diseases
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1094-1101
Abstract
Original ArticlePerinatal Outcomes in Women with Chronic Kidney Diseases
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1094-1101
Views193See moreAbstract
Objective
To assess maternal and neonatal outcomes in women with chronic kidney disease (CKD) at a referral center for high-risk pregnancy.
Methods
A retrospective cohort of pregnant women with CKD was followed at the Women's Hospital of Universidade Estadual de Campinas, Brazil, between 2012 and 2020. Variables related to disease etiology, treatment duration, sociodemographic variables, lifestyle, other associated diseases, obstetric history, and perinatal outcomes were assessed. The causes of CKD were grouped into 10 subgroups. Subsequently, we divided the sample according to gestational age at childbirth, as preterm and term births, comparing maternal and neonatal outcomes, and baseline characteristics as well as outcomes among such groups.
Results
A total of 84 pregnancies were included, in 67 women with CKD. Among them, six pregnancies evolved to fetal death, five to miscarriage, and one was a twin pregnancy. We further analyzed 72 single pregnancies with live births; the mean gestational age at birth was 35 weeks and 3 days, with a mean birth weight of 2,444 g. Around half of the sample (51.39%) presented previous hypertension, and 27.7% developed preeclampsia. Among the preterm births, we observed a higher frequency of hypertensive syndromes, longer maternal intensive care unit (ICU) stay in the postpartum period, higher incidence of admission to the neonatal ICU, higher neonatal death, lower 5-minute Apgar score, and lower birth weight.
Conclusion
This study demonstrates increased adverse outcomes among pregnancies complicated by CKD and expands the knowledge on obstetric care among such women in an attempt to reduce maternal risks and identify factors related to prematurity in this population.
-
Original Article03-24-2022
Misoprostol Administration Before Hysteroscopy Procedures – A Retrospective Analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1102-1109
Abstract
Original ArticleMisoprostol Administration Before Hysteroscopy Procedures – A Retrospective Analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1102-1109
Views238See moreAbstract
Objective
To evaluate the use of misoprostol prior to hysteroscopy procedures regarding technical ease, the presence of side effects, and the occurrence of complications.
Methods
This is a retrospective, observational, analytical, case-control study, with the review of medical records of 266 patients followed-up at the Gynecological Videoendoscopy Sector of the Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto of the Universidade de São Paulo (HCFMRP – USP, in the Portuguese acronym) from 2014 to 2019, comparing 133 patients who used the drug before the procedure with 133 patients who did not.
Results
The occurrence of postmenopausal uterine bleeding was the main indication for hysteroscopy and revealed a statistical difference between groups (p < 0.001), being present in 93.23% of the patients in the study group and in 69.7% of the patients in the control group. Only 2 patients (1.5%) in the study group reported adverse effects. Although no statistical differences were observed regarding the occurrence of complications during the procedure (p = 0.0662), a higher total number of complications was noted in the group that used misoprostol (n = 7; 5.26%) compared with the group that did not use the drug (n = 1; 0.75%), a fact that is clinically relevant. When evaluating the ease of the technique (measured by the complete performance of all steps of the hysteroscopy procedure), it was verified that although there was no difference between groups (p = 0.0586), the control group had more than twice as many incompletely performed procedures (n = 17) when compared with the group that used misoprostol previously (n = 8), which is also clinically relevant.
Conclusion
The use of misoprostol prior to hysteroscopy in our service indicated that the drug can facilitate the performance of the procedure, but not without side effects and presenting higher complication rates.


