Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):494-496
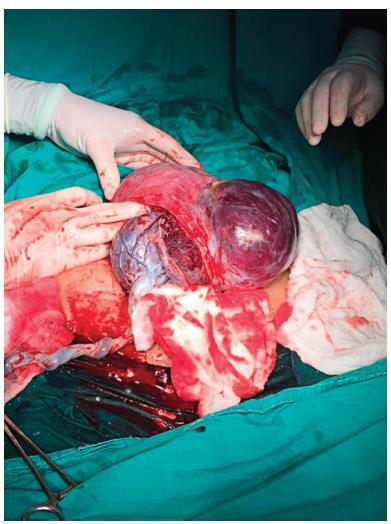
Placenta accreta syndromes are associated with increased maternal mortality and morbidity. Cesarean hysterectomy is usually performed in cases of placenta accreta syndrome. Fertility sparing methods can be applied. In the present study, we report a successful segmental uterine resection method for placenta accreta in the anterior uterine wall in a cesarean section case. A 39-year-old woman underwent an elective cesarean section at 38 + 2 weeks. A placental tissue with an area of 10 cm was observed extending fromthe anterior uterine wall to the serosa, 2 cm above the uterine incision line. The placental tissue was removed with the help of monopolar electrocautery. The uterine incision was continuously sutured. The patient was discharged on the second postoperative day. The placental pathology was reported as placenta accreta. The American College of Obstetricians and Gynecologists (ACOG) generally recommends cesarean section hysterectomy in cases of placenta accreta because removal of placenta associated with significant hemorrhage. Conservative and fertility sparing methods include placenta left in situ, cervical inversion technique and triple-P procedure. There are several studies reporting that segmental uterine resection is performed with and without balloon placement or artery ligation. Segmental uterine resection may be an alternative to cesarean hysterectomy to preserve fertility or to protect the uterus in cases of placenta accreta when there is no placenta previa. received
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):491-493
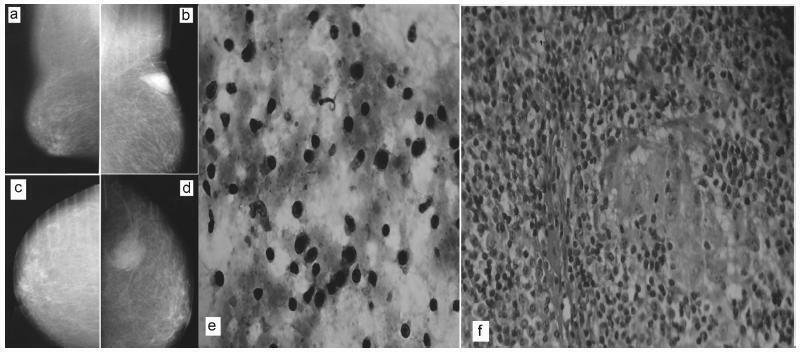
There are rare benign diseases that can mimic malignant breast neoplasms in the clinical exam and in mammography. We evaluated the contribution of an accessible procedure to most clinicians, the fine-needle aspiration cytology, to identify a rare mimicker of malignant breast neoplasms. A type 2 diabetic 85-year-old female presented with a 6-month history of a left breast lump. The physical exam and mammography were compatible with breast cancer. Nevertheless, after fine-needle aspiration cytology, the diagnosis was plasma cellmastitis. Once this rare diagnosis was established, the tumor was extirpated, and the final histologic diagnosis corroborated chronic plasma cellmastitis. The patient’s postoperative evolution was uneventful, and no other treatment was needed. Fine-needle aspiration cytology could be a valuable tool to identify rare mimickers of malignant breast neoplasms.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):430-432
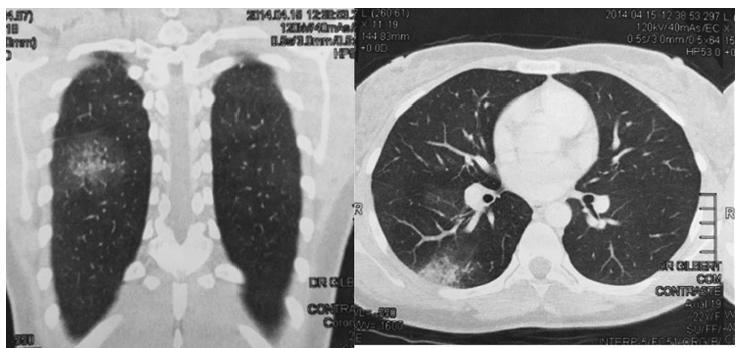
Mirror syndrome is an unusual pathological condition in which maternal edema in pregnancy is seen in association with severe fetal and/or placental hydrops. The disease can be life-threatening for both the mother and the fetus. The pathogenesis is poorly understood, and may be confused with preeclampsia, even though distinguishing features can be identified. We report a rare case of mirror syndrome with maternal pulmonary edema associated with fetal hydrops due to Patau syndrome.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):425-429
Polyglandular autoimmune syndrome type II (PGA-II) is a rare immunoendocrinopathy syndrome characterized by the occurrence of autoimmune Addison disease along with diabetes mellitus type 1 and/or autoimmune thyroid disease. Here, we report the case of a 23-year-old female with PGA-II who was followed up at the dermatology and endocrinology clinics of the Universidade Federal do Triângulo Mineiro, located in the state of Minas Gerais, Brazil. First, the patient presented diffuse skin hyperpigmentation, vitiligo; and in sequence, due to vomiting, appetite and weight loss, hypoglycemia, amenorrhea, and galactorrhea, the patient was then diagnosed with PGA-II. The patient also presented intense hyperprolactinemia due to primary hypothyroidism. The late diagnosis of PGA-II is frequent because the disorder is uncommon and has non-specific clinical manifestations. This report emphasizes the significance of a timely diagnosis and appropriate treatment to reduce morbidity and mortality associated with these diseases, especially Addison disease. The present study reports a rare case of a patient with PGA-II with primary amenorrhea associated with hyperprolactinemia.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):372-376
Parvovirus B19 has tropism for red line blood cells, causing immune hydrops during pregnancy. A positive anti-Kell Coombs reaction usually happens during pregnancy when there is production of antibodies that target Kell antigens, but cross reactions to other antigens may occur. A 24-year-old Gypsy primigravida, 0 Rhesus positive, presented with persistent isolated hyperthermia for 2 weeks and a positive indirect Coombs test result with anti-Kell antibodies at routine tests. She had a 19-week live fetus. The blood tests revealed bicytopenia with iron deficiency anemia, leucopoenia with neutropenia, and elevated C-reactive protein. She was medicated with imipenem, and had a slow clinical recovery. Blood, urine and sputum samples were taken to perform cultures and to exclude other systemic infections. Escherichia coli was isolated in the urine, which most probably caused a transient cross anti-Kell reaction. Haemophilus influenza in the sputum and seroconversion to parvovirus B19 was confirmed, causing unusual deficits in the white cells, culminating in febrile neutropenia. Despite the patient’s lack of compliance to the medical care, both maternal and fetal/neonatal outcomes were good. This a rare case report of 2 rare phenomena, a cross anti-Kell reaction to E. coli and parvovirus B19 infection with tropism for white cells causing febrile neutropenia, both events occurring simultaneously during pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):369-371
Hemangioma is a benign neoplasm that may affect the vulva, and it can cause functional or emotional disability. This article reports the case of a 52-year-old female patient with a history of a genital ulcer for the past 3 years and who had undergone various treatments with creams and ointments. The patient was biopsied and diagnosed with vulvar hemangioma and was subsequently submitted to surgical excision of the lesion. We emphasize the importance of following the steps of the differential diagnosis and proceeding with a surgical approach only if necessary.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):300-303
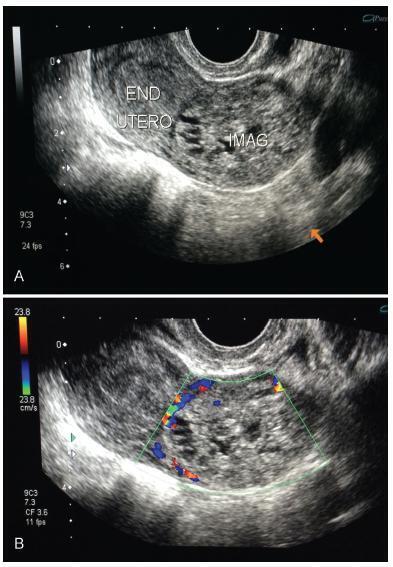
Thoracic endometriosis syndrome is a rare condition that includes four entities: catamenial pneumothorax, catamenial hemothorax, catamenial hemoptysis and lung nodules. We describe the case of a 23-year-old woman with complaints of hemoptysis during menstrual period in the two years prior to the appointment. Initially, a treatment for tuberculosis was established with no success. Further investigation showed a 4 mmnodule in the right lung, and the transvaginal ultrasonography indicated the presence of deep endometriosis. Considering the occurrence of symptoms only during menses, an empirical therapy was instituted with remission of the complaints.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):294-299
This report presents the case of a patient with gestational trophoblastic neoplasia after a partial hydatidiform mole formed in the Fallopian tube. Ectopic molar pregnancy is a rare condition, with an estimated incidence of 1 in every 20,000 to 100,000 pregnancies; less than 300 cases of it have been reported in the Western literature. The present report is important because it presents current diagnostic criteria for this rare condition, which has been incorrectly diagnosed in the past, not only morphologically but also immunohistochemically. It also draws the attention of obstetricians to the occurrence of ectopic molar pregnancy, which tends to progress to Fallopian tube rupture more often than in cases of ectopic non-molar pregnancy. Progression to gestational trophoblastic neoplasia ensures that patients with ectopic molar pregnancy must undergo postmolar monitoring, which must be just as thorough as that of patients with intrauterine hydatidiform moles, even if chemotherapy results in high cure rates.