Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(8):386-393
DOI 10.1590/S0100-72032012000800008
PURPOSE: To evaluate sociodemographic, behavioral and reproductive factors and morbidities associated with inadequate weight gain during pregnancy. METHODS: Cohort study conducted from December 2007 to August 2008 with women in the first trimester of pregnancy looking for prenatal care in the Public Health System who lived in the cities of Petrópolis or Queimados, Rio de Janeiro state (Brazil). Women with multiple pregnancy, who had a miscarriage in the index pregnancy or who lacked information for the assessment of pregravid nutritional status or weight gain were excluded. Pregravid nutritional status and weight gain during pregnancy were determined according to the criterion established by the Institute of Medicine (IOM). Statistical analysis was performed using a multinomial logistic regression model. RESULTS: A total of 1,287 women were included in the study; 26.6% of them were overweight or obese while 11% were underweight. Inadequate weight gain during pregnancy was observed in 71.4% of pregnant women; 35.6% of them did not gain enough weight while 35.8% gained more weight than recommended by the IOM. In the multivariate analysis, women with hypertension (OR=2.1; 95%CI 1.4-3.1), pregravid overweight (OR=2.5; 95%CI 1.4-4.5) or obesity (OR=2.7; 95%CI 1.8-3.9) and who had a higher educational level were more likely to gain more weight than recommended, while pregravid underweight (OR=0.6; 95%CI 0.4-0.9) represented a protection against excessive gain. CONCLUSION: Pregravid nutritional diagnosis and weight gain monitoring should be actions effectively instituted in the routine of health professionals.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):296-303
DOI 10.1590/S0100-72032012000700002
PURPOSE: To determine the pattern of alcohol use before and during pregnancy and associated risk factors in puerperal women hospitalized in a public university hospital in Southeastern Brazil. METHODS: Between June and September 2009, 493 puerperae were consecutively evaluated. Those with cognitive impairment were excluded from the study. The AUDIT and CAGE questionnaires were used to diagnose alcohol use/abuse before pregnancy, in addition to the T-ACE during pregnancy. Another questionnaire was applied to collect sociodemographic data, such as age, educational level, marital status, and household income. The χ² test was used in the statistical analysis and the Odds Ratio (OR) and 95% confidence interval (95%CI) were calculated. A p-value <0.05 was considered to be significant. RESULTS: Before pregnancy, the CAGE was positive in 50/405 (12.3%) women and the AUDIT identified alcohol use in 331 (67.1%), which was of low risk in 233 (47.3%), risky in 73 (14.8%), and harmful or indicating possible alcohol dependence in 25 (5%). During pregnancy, the CAGE was positive in 53/405 (13.1%) women and the T-ACE in 84 (17%); the AUDIT identified alcohol use in 114 women, which was of low risk in 73 (14.8%), risky in 27 (5.5%), and harmful or indicating possible alcohol dependence in 14 (2.8%). During pregnancy, alcohol use was more frequent (OR=2.8; 95%CI 1.2 - 6.2) among women with a lower educational level (8.8 versus 3.3%) and more frequent (OR=3.8; 95%CI 1.3 - 11.1) among those who did not cohabit with a partner (6 versus 1.7%). Among pregnant women who drank alcohol, 49/114 (43%) were advised to stop drinking. CONCLUSIONS: Alarming alcohol use was observed during pregnancy, especially among pregnant women with a lower educational level and those who did not cohabit with a partner. There was a low frequency of counseling aimed at abstinence and the AUDIT was the instrument that most frequently diagnosed alcohol consumption.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):304-309
DOI 10.1590/S0100-72032012000700003
PURPOSE: To evaluate the impact of body mass index (BMI) at the beginning of pregnancy and weight gain on pregnancy outcome so that this measure can be implemented and valued by prenatal care health services. METHOD: Cross-sectional population-based study of all births in the only two hospitals in Rio Grande city (Brazil), in 2007. Among the 2,557 mothers interviewed, it was possible to calculate BMI in only 1,117. The Stata 11 software was used for data analysis. Logist regression was applied to the outomes involving diabetes mellitus, premature labor and cesarean section. Regarding birth weight, data were adjusted by multinomial logistic regression using as base category the group of 2,500 to 4,000 g. The level of significance was set at p-value <0.05 in a two-tailed test. RESULTS: There was no increased risk of hypertension or diabetes in patients in the different groups of BMI and weight gain. The risk of preterm delivery was evident in the group with a weight gain ≤8 kg (p<0.05). Regarding the route of delivery, it was observed that the higher the BMI in early pregnancy (p=0.001) and the greater the weight gain during pregnancy (p=0.004), the greater the risk of surgical delivery, which reached 11% in the group of obese mothers (p=0.004) and 12% in the group with a weight gain ≥17 kg (p=0.001). The weight of the newborns was influenced by BMI and weight gain, and the higher the BMI in early pregnancy and the gestational weight gain, the greater the risk of macrosomia. CONCLUSION: The monitoring of BMI and weight gain during pregnancy is a low cost and useful procedure for the establishment of nutritional interventions aimed at reducing maternal and fetal risks.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):310-315
DOI 10.1590/S0100-72032012000700004
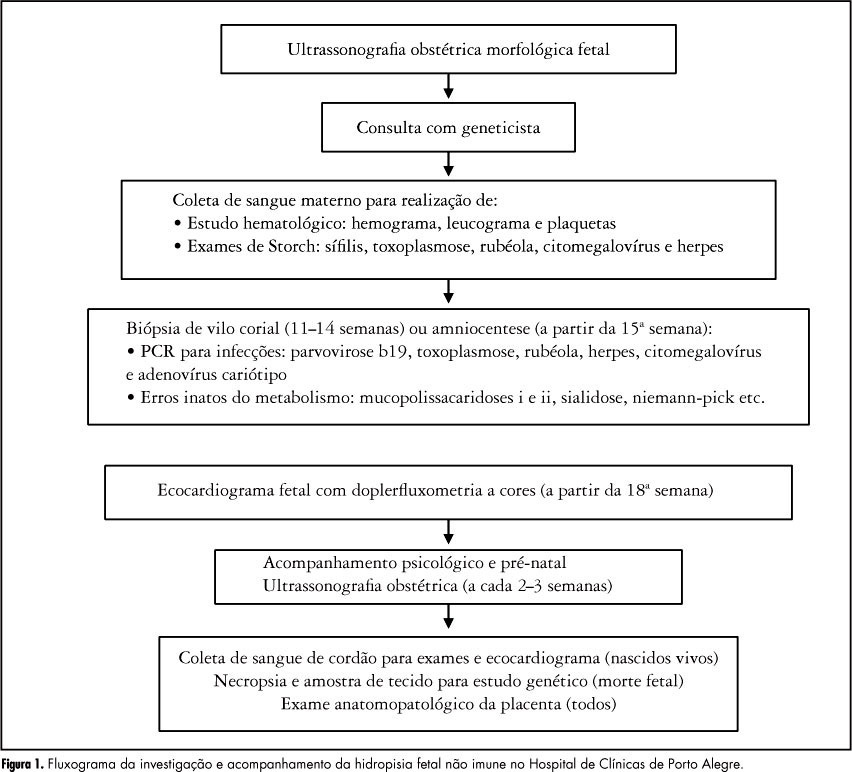
PURPOSE: To identify the etiology of nonimmune hydrops fetalis cases in pregnant women diagnosed and referred for prenatal care. METHODS: Retrospective analysis of cases with nonimmune hydrops fetalis that were monitored between March 1992 and December 2011. Diagnosis was confirmed by the presence of fetal subcutaneous edema (≥5 mm) with effusion in at least one serous cavity using obstetric ultrasound, and etiological investigation was conducted with cytogenetic (karyotype), infectious (syphilis, parvovirus B19, toxoplasmosis, rubella, cytomegalovirus, adenovirus and herpes simplex), hematologic and metabolic (inborn errors) analysis and fetal echocardiography. Twin pregnancies were excluded. Statistical analysis was performed using the χ² test for adhesion (software R 2.11.1). RESULTS: We included 116 patients with nonimmune hydrops fetalis; the etiology was elucidated in 91 cases (78.5%), while 25 cases (21.5%) were classified as idiopathic. Most cases had a chromosomal etiology, for a total of 26 cases (22.4%), followed by lymphatic etiology with 15 cases (12.9% with 11 cases of cystic hygroma), and cardiovascular and infectious etiology with 14 cases each (12.1%). In the remaining cases, the etiology was thoracic in 6.9% (eight cases), malformation syndromes in 4.3% (five cases), extrathoracic tumors in 3.4% (four cases), metabolic in 1.7% (two cases), and hematologic, gastrointestinal and genitourinary in 0.9% (one case each). During the postnatal period, 104 cases were followed up until the 40th day of life, and 12 cases had intrauterine fetal death. The survival rate of these 104 newborns was 23.1% (24 survived). CONCLUSION: An attempt should be made to clarify the etiology of hydrops diagnosed during pregnancy since the condition is associated with a wide spectrum of diseases. It is especially important to determine whether a potentially treatable condition is present and to identify disease at risk for recurrence in future pregnancies for adequate pre-conception counseling.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):316-322
DOI 10.1590/S0100-72032012000700005
PURPOSE: To compare the metabolic parameters, body composition and muscle strength of women with Polycystic Ovary Syndrome (PCOS) to those of women with ovulatory menstrual cycles. METHODS: A case-control study was conducted on 27 women with PCOS and 28 control women with ovulatory cycles, aged 18 to 27 years with a body mass index of 18 to 39.9 kg/m², who did not practice regular physical activity. Serum testosterone, androstenedione, prolactin, sex hormone-binding globulin (SHBG), insulin and glycemia levels were determined. Free androgen index (FAI) and resistance to insulin (by HOMA) were calculated. The volunteers were submitted to evaluation of body composition based on skin folds and DEXA and to 1-RM maximum muscle strength tests in three exercises after familiarization procedures and handgrip isometric force was determined. RESULTS: Testosterone levels were higher in the PCOS group than in the Control Group (68.07±20.18 versus 58.20±12.82 ng/dL; p=0.02), as also were the FAI (282.51±223.86 versus 127.08±77.19; p=0.01), insulin (8.41±7.06 versus 4.05±2.73 µIU/mL; p=0.01), and HOMA (2.3±2.32 versus 1.06±0.79; p=0.01), and SBHG levels were lower (52.51±43.27 versus 65.45±27.43 nmol/L; p=0.04). No significant differences in body composition were observed between groups using the proposed methods. The PCOS group showed greater muscle strength in the 1-RM test in the bench press (31.2±4.75 versus 27.79±3.63 kg; p=0.02), and leg extension exercises (27.9±6.23 versus 23.47±4.21 kg; p=0.02) as well as handgrip isometric force (5079.61±1035.77 versus 4477.38±69.66 kgf/m², p=0.04). PCOS was an independent predictor of increase muscle strength in bench press exercises (estimate (E)=2.7) (p=0.04) and leg extension (E=3.5) (p=0.04), and BMI in the exercise of isometric handgrip (E=72.2) (p<0.01), bench press (E=0.2) (p=0.02) and arm curl (E=0.3) (p<0.01). No association was found between HOMA-IR and muscle strength. CONCLUSIONS: Women with POS showed greater muscle strength, with no difference in body composition, and IR was not associated with muscle strength performance. Muscle strength may be possibly related to high levels of androgens in these women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):323-328
DOI 10.1590/S0100-72032012000700006
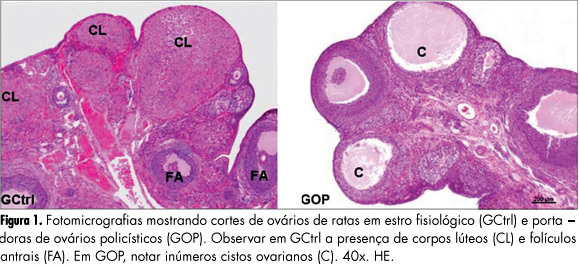
PURPOSES: To evaluate the histomorphometry of ovarian interstitial cells, as well as the blood sex steroid concentrations of female rats with polycystic ovaries induced by continuous light. METHODS: Twenty female rats were divided into two groups: Control Group - in the estrous phase (CtrlG), and a group of rats with polycystic ovaries induced by continuous illumination (POG). CtrlG animals were maintained on a light period from 07:00 a.m. to 07:00 p.m., and POG animals with continuous illumination (400 Lux) for 60 days. After this period all animals were anesthetized and blood was collected for the determination of serum estradiol (E2), progesterone (P4), and testosterone (T), followed by removal of the ovaries that were fixed in 10% formalin and processed for paraffin embedding. Five-µm histological sections were stained with hematoxylin and eosin and used for histomorphometric analysis. Morphological analyses, cyst count, determination of concentration and of the nuclear volume of interstitial cells were performed with the aid of a light microscope adapted to a high resolution camera (AxioCam), whose images were transmitted to and analyzed by the computer using AxioVision Rel 4.8 software (Carl Zeiss). Data were analyzed statistically by the Student's t-test (p<0.05). RESULTS: Morphological analysis showed the presence of ovarian cysts in POG animals and corpora lutea in CtrlG animals, as well as evidence of the origin of interstitial cells from the internal theca of these cysts. POG animals presented increased serum estradiol levels (pg/mL) compared to CtrlG animals (POG=124.9±4.2>CtrlG=73.2±6.5, p<0.05), the same occurring with testosterone levels (pg/mL) (POG=116.9±4.6>CtrlG=80.6±3.9, p<0.05). However, progesterone levels (ng/mL) were higher in CtrlG than in POG animals (CtrlG=16.3±2.0>POG=4.2±1.5, p<0.05). Morphometry showed a significant increase in nuclear volume in POG animals (POG=102.1±5.2>CtrlG=63.6±16.5, p<0.05), as well as in the area occupied (%) by interstitial cells (POG=24.4±6.9>CtrlG=6.9±3.2, p<0.05) compared to CtrlG animals. CONCLUSION: The interstitial cells of the rat polycystic ovary probably originate from ovarian cysts due to the degeneration of granulosa cells and differentiation of the internal theca cells. The elevations of serum testosterone and estradiol were probably due to the significant increase in cell activity and in the area occupied by interstitial cells.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):329-334
DOI 10.1590/S0100-72032012000700007
PURPOSE: To evaluate the influence of climacteric symptoms on the sexual function in middle-aged women. METHODS: A cross-sectional population study was conducted on a sample of 370 middle-aged women, aged 40 to 65 years-old, cared for at the Basic Health Units in Natal, in the state of Rio Grande do Norte, Brazil. We used a questionnaire containing questions on sociodemographic, clinical, and behavioral characteristics. Sexual function was evaluated by the Female Sexual Function Index (FSFI), while the menopause symptoms by the Menopause Rating Scale (MRS). RESULTS: In the studied group, 67% of the women reported risk for sexual dysfunction (FSFI≤26.5). All FSFI domains (desire, arousal, lubrication, orgasm, satisfaction, and pain) were lower in women with risk for sexual dysfunction (p<0.001). The arousal, orgasm, and pain domains were most likely to contribute to lower FSFI scores. All somatovegetative, urogenital, and psychological MRS symptoms were more elevated in women with risk for sexual dysfunction, being significant for all comparisons (p<0.001). Logistic regression analysis revealed that the likelihood of women with risks of sexual dysfunction to present hot flushes, depression, sexual problems, and vaginal dryness was, respectively, 2.1 (95%CI 1.2 - 3.5); 2.4 (95%CI 1.5 - 4.1); 2.3 (95%CI 1.4 - 3.8), and 2.2 (95%CI 1.3 - 3.6) times higher, respectively, compared to those without any risk. CONCLUSION: Climacteric symptoms seem to influence the sexual function in middle-aged women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):248-253
DOI 10.1590/S0100-72032012000600002
PURPOSE: To verify whether women with atypias of undetermined significance and precursor lesions or invasive cervical outcomes were referred to Medium Complexity Units (MCU) following the guidelines recommended by the Brazilian Ministry of Health. METHODS: Retrospective study based on the cytopathological outcomes of users of the Unified Health System, seen at Basic Health Assistance Units (BHAU) and referred to MCUs in the municipality of Goiânia, state of Goiás, from 2005 to 2006. We assessed 832 records according to the recommendations of the Brazilian Ministry of Health, as established by the Brazilian Nomenclature for Cervical Cytopathologic Outcomes and Recommended Clinical Practice. To check the distribution of variables such as reasons for referral, results of colposcopy and histopathology and clinical procedures we calculated absolute and relative frequencies, mean, minimum and maximum values. RESULTS: We understood 72.7% of the referrals were not in accordance with the recommendations of the Ministry of Health. There were 605 women with test results classified as atypical squamous cells of undetermined significance, possibly non-neoplasms, and squamous intraepithelial lesion of low level which were sent to MCU, and of these 71.8% were submitted to colposcopy, and 64.7% had histopathological examination which results were classified as 31.0% with non-neoplasms and 44.6% as NIC I. Out of 211 women with results classified as more severe squamous lesions, 86.3% were submitted to colposcopy and 68.7% of these had histopathological examinations. CONCLUSIONS: The results of this study revealed high rates of inappropriate referrals to MCU, which required a high percentage of unnecessary procedures. The recommendations of the Ministry of Health were followed by BHAU and the majority of women received counseling/treatment as recommended.