Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(1):19-24
DOI 10.1590/S0100-72032008000100004
PURPOSE: The aim of this article is to evaluate the use of nevirapine HIV-infected pregnant women in our service. METHODS: a retrospective study was performed between January 2003 and December 2006 analysing all women prescribed nevirapine in pregnancy. Exclusion criteria included: (1) women who started nevirapine before pregnancy, (2) patients with abnormal baseline liver enzymes, and (3) women with incomplete liver biochemistry data. Evaluated parameters included age, weeks of exposure to nevirapine, gestational age in the begginning of medication, weeks of follow-up, viral load, CD4 cells count and serum aminotransferase levels. The incidence of adverse hepatic and/or cutaneous effects was determined and correlated to the CD4 cells count. Statistical analysis were performed using Fisher’s exact test and t-Student test when appropriate, with a statistical significance level of p<0,05. RESULTS: one hundred fifty-seven women met the inclusion criteria. Thirty-one (19.7%) presented cutaneous and/or hepatic toxicity. Skin rash accounted for 77.4% of toxicities and liver function abnormalities were noted in 22.6% of women exhibiting toxicities. Grade 1, 2 and 3 hepatotoxicities were observed in 0.6, 2.5 and 1.3%, respectively. Baseline CD4 counts, viral loads and transaminases were similar in pregnant women with nevirapine adverse effects and those without reaction. Median absolute CD4 cell counts were 465.4 and 416.6 cells/µL in women with and without side effects, respectively (p=0.3). All patients who experienced hepatotoxicity had pretreatment CD4 counts superior to 250 cells/µL. CONCLUSIONS: The incidence of adverse events with nevirapine in our study was high, but most of them were cutaneous. There was no correlation between high CD4 counts and adverse events when analysing both cutaneous and hepatic reactions; nevertheless, hepatotoxicity occurred only in pregnant women with CD4 counts >250 cells/µL.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):614-618
DOI 10.1590/S0100-72032007001200003
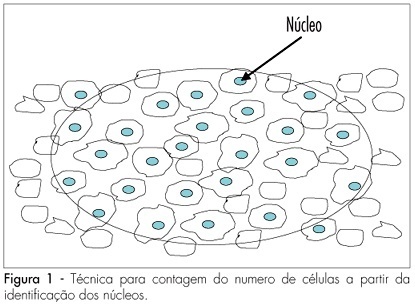
PURPOSE: to determine the variation of the number of ovarian follicles during fetal life. METHODS: twelve ovaries donated for research were included in our study, nine from fetuses and three from newborn babies who died in the first hour after being delivered with 39 weeks of pregnancy. Fetal age was confirmed both by the last menstrual period of the woman and by ultrasonography. Ovaries were fixed in formaldehyde, included in paraffin and serially sliced at 7 mm. At every 50 cuts, the obtained material was haematoxilin-eosin stained and evaluated with an optical microscope (400 X). The follicles were counted in ten different regions of the ovarian cortex, each region with an area of 625 mm². The presence of a nucleus was considered the parameter for counting. Follicular density, per 1 mm³ was calculated using the formula Nt=(No x St x t)/do, where Nt is the number of follicles; No is the mean number of follicles in 1 mm²; St is the total number of slices in 1 mm³; t is the slice thickness and do is the nuclei mean diameter. RESULTS: the gestational age of fetuses ranged from 24 to 39 weeks. The number of follicles per 0.25 mm² ranged from 10.9 ± 4.8 in a newborn to 34.7 ± 10.6 in another newborn. Among the fetuses, the least value was obtained in a 36 week-old fetus (11.1 ± 6.2) and the highest in a 28 week-old fetus (25.3 ± 9.6). The total number of slices per ovary ranged from six to 13, corresponding to follicles counted in areas from 15 to 32.5 mm². The total number of follicles ranged from 500,000 at the age of 22 weeks to > 1,000,000 at the age of 39 weeks. CONCLUSIONS: our results demonstrate different (increasing) densities of ovarian follicles along the gestational period, providing more knowledge about this still not well-known subject.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):608-613
DOI 10.1590/S0100-72032007001200002
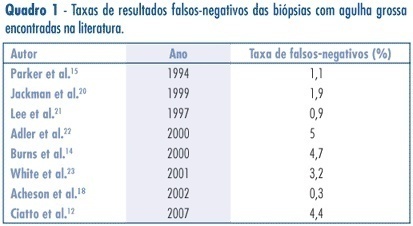
PURPOSE: to assess the accuracy (rate of correct predictions) of stereotactic core needle biopsy (CNB) of risk category BI-RADS® 4 breast lesions. METHODS: a retrospective analysis of category BI-RADS® 4 breast lesions that had been submitted to a stereotactic core-needle biopsy from June 1998 to June 2003. Patients with histological benign results consistent with the radiographic image were referred to mammographic follow-up. Patients with malign diagnosis and papillary lesions were submitted to standard specific treatment. Excisional biopsies were performed when results were benign, but in disagreement with the mammographic image. It was considered as a gold-standard attendance: (1) the mammographic follow-up of low suspicion lesions with benign results at CNB, which stayed unchanged for, at least, three years, and (2) surgical resection when specimen results were malign or benign, but with a high suspicion on mammography. Sensitivity (S) specificity (E) and overall accuracy of stereotactic CNB were statistically analyzed. RESULTS: among the 118 non-palpable lesions of category BI-RADS® 4 submitted to CNB, the results obtained were: 27 malign cases, 81 benign, and ten lesions with atypical or papillary lesions. The statistical analysis comprised 108 patients (atypical and papillary lesions were excluded). CNB sensitivity was 87.1% and specificity 100%. The positive predictive value was 100% and the negative, 95.1%. False negatives occurred in 3.7% (4/108) of cases. The prevalence of malign diagnostics in the BI-RADS® 4 lesions of this sample was 29.7 (31/118).The accuracy of this method in this casuistic was 96.3%. CONCLUSIONS: these results support stereotactic CNB as an extremely reliable alternative to open biopsy, in the diagnosis and definition of breast lesions. In positive results, it is possible to indicate the appropriate therapy, and, in negative (when mammography shows low suspicion), it allows a follow up.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):639-646
DOI 10.1590/S0100-72032007001200007
PURPOSE: to compare the effectiveness of low doses of vaginal misoprostol (12.5 versus 25 µg) for induction of labor. METHODS: a double-blind, randomized, controlled clinical trial was performed in Santa Casa de Misericórdia de Sobral, from May 2005 to April 2006. Sixty-two term pregnant women, with intact membranes and with indication for labor induction, were included. They randomly received 25 µg (32) or 12.5 µg (30) of vaginal misoprostol each four hours, until the maximum of eight doses. Mode of delivery, time between induction and delivery, perinatal complications, and maternal side effects were studied. The control variables were maternal and gestational ages, parity and Bishop score. The statistical tests used were average calculations, shunting line-standards and Student t-test (numerical continuous variables), chi2 (categorical variables) and Mann-Whitney test (discrete variables). RESULTS: the two groups, 12.5 and 25 µg, did not differ in relation to the interval of time between the induction onset and delivery (1524 versus 1212 min, p=0.333), in the frequency of vaginal delivery (70 versus 71.8%, p=0.720), Apgar scores below seven at the fifth minute (3,3 versus 6,25%, p=0.533) and tachysystole frequency (3.3 versus 9.3%, p=0.533). The average of total dose administered was significantly higher in the 25 µg group (40 versus 61.2 µg, p=0.03). CONCLUSIONS: vaginal misoprostol in the dose of 12.5 µg was efficient, with collateral effects similar, to the 25 µg of vaginal misoprostol, for induction of labor at term.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):633-638
DOI 10.1590/S0100-72032007001200006
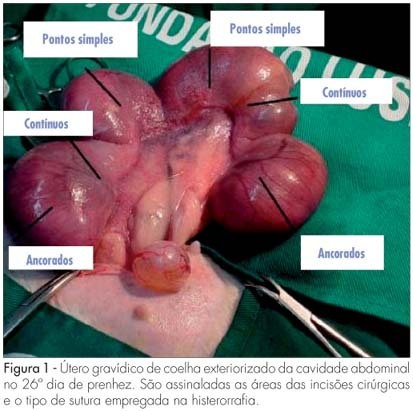
PURPOSE: to compare macro and microscopically, surgical uterine sutures in female rabbits, after caesarean section utilizing separate, continuous and continuous anchored suture stitches. METHODS: three New Zealand female rabbits in their first pregnancy were used. The caesarean section was carried out at the 26th day of gestation and three incisions were performed in each uterus. The hysterorrhaphy was performed with a 00 Vicryl® thread, and a different suture technique was employed for each incision. Total hysterectomy and adnexectomy were done at the 60th day post-delivery with the preservation of eventual adhesions for the evaluation of the surgical scars. The extent of scar retraction, amount of fibrin deposit and the suture integrity were evaluated through macroscopy. For the evaluation through microscopy, hematoxylin eosin technique was used for cellular colorimetry, and Masson's trichrom to evidence collagen. The statistical non-parametric Friedman's test was employed for the matching hypothesis, and Fisher's exact test to verify the homogeneity of the techniques (level of significance: 5%). RESULTS: a total of 18 scars were obtained (six scars per suture). The following mean values were obtained for the longitudinal (0.5/0.4/0.5, p=0.069) and transversal retraction degrees (0.3/0.4/0.3, p=0.143) respectively for separate, continuous and continuous anchored suture techniques. All sutures presented regular fibrin deposit, no adhesions and integral absorption of the stitches. The mean value of the blood vessels (158.5/139.3/172.1; p=0.293), fibroblasts (351.6/345.8/354.3; p=0.311) and of collagen percentage (44.0/45.5/48.5; p=0.422) were calculated through microscopy, respectively for separate, continuous and continuous anchored suture techniques. CONCLUSIONS: the type of hysterorrhaphy technique of caesarean section in female rabbits did not generate any significant statistical difference in the macroscopic and microscopic parameters evaluated.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):625-632
DOI 10.1590/S0100-72032007001200005
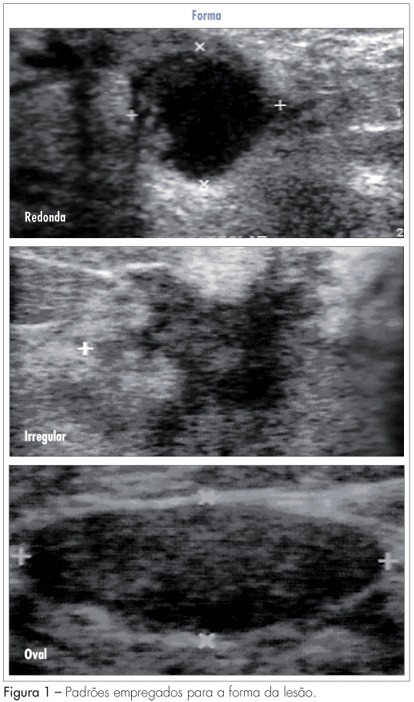
PURPOSE: to analyze which characteristics proposed by the BIRADS lexicon for ultrasound have the greatest impact on distinguishing between benign and malignant lesions. METHODS: ultrasonography features from the third edition of the BIRADS were studied in 384 nodes submitted to percutaneous biopsy from February 2003 to December 2006, at the Medical School of Botucatu. For the ultrasonography, the equipment Logic 5 with a 7.5-12 MHz multifrequential linear transducer was used. The ultrasonography analysis of the node considered the features proposed by the BIRADS lexicon for ultrasound. The data were submitted to statistical analysis by the logistic regression model. RESULTS: the benign lesions represented 42.4% and the malignant, 57.6%. The logistic regression analysis found an odds ratio (OR) for cancer of 7.69 times when the surrounding tissue was altered, of 6.25 times when there were microcalcifications in the lesions interior, of 1.95 when the acoustic effect is shadowing, of 25.0 times when there was the echogenic halo, and of 7.14 times when the orientation was non-parallel. CONCLUSIONS: among the features studied, the lesion limit, represented by the presence or not of the halogenic halo, is the most important differentiator of the benign from the malignant masses.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):619-624
DOI 10.1590/S0100-72032007001200004
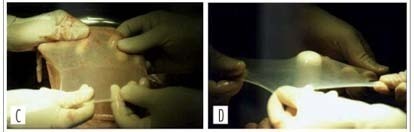
PURPOSE: to evaluate the results of neovaginoplasty with the use of a human amniotic graft in patients with the Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. METHODS: the study was a retrospective analysis of a series of 28 patients with the MRKH syndrome conducted from 1990 to 2003. The patients were attended and treated at the Ambulatório de Ginecologia Infanto-Puberal (AGIP) of the Hospital Universitário of the Faculdade de Medicina de Ribeirão Preto of the Universidade de São Paulo (FMRP-USP), being submitted to neovaginoplasty by the technique of McIndoe and Bannister, modified by the use of a human amniotic membrane graft. Epithelization, amplitude and depth of the neovaginas were evaluated 7 and 40 days after the procedure. Patient satisfaction was determined during the late postoperative period in terms of the presence of discomfort and dyspareunia during sexual relations. RESULTS: postoperatively, seven patients (25%) presented vaginal stenosis and six of them were submitted to a new surgical intervention, one had shortening of the neovagina, corrected with the use of exercises with a vaginal mold, three (10.7%) developed a rectovaginal fistula, one (3.6%) a uterovesical fistula, and one (3.6%) excess skin in the vaginal introitus - all successfully corrected with surgery. Four patients (14.3%) presented urinary tract infection. Two months after surgery, 11/19 patients (57.8%) presented satisfactory sexual activity and 42% dyspareunia, and within a maximum period of four years, 20/21 patients (95.2%) had satisfactory sexual activity and 4.8% dyspareunia. CONCLUSIONS: an amniotic membrane graft is a good option for the treatment of vaginal agenesis. Perioperative follow-up involves educational guidance regarding the use of the mold and regarding patient sexuality in order to reduce the complaints of dysfunctional coitus in the presence of a favorable surgical evolution and a neovagina of adequate aspect.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(3):121-126
DOI 10.1590/S0100-72032008005000002
PURPOSE: to compare the frequency of vulvovaginitis in women infected with human imunnodeficiency virus (HIV) with the frequency in non-infected women. METHODS: a transversal study including 64 HIV infected women and 76 non-infected ones. The frequencies of bacterial vaginosis, candidiasis and trichomoniasis, diagnosed by Amsel's criteria, culture and fresh exam, respectively, were calculated. Chi-square test, Fisher's exact test and multiple regressions to verify the independence of associations were used to analyze the data. RESULTS: the vaginal infection was more prevalent in HIV infected patients, as compared to the control group (59.4 versus 28.9%, p<0,001; Odds Ratio=2.7, IC95%=1.33-5.83, p=0.007). Bacterial vaginosis occurred in 26.6% of the positive-HIV women; vaginal candidiasis, in 29.7% and trichomoniasis, in 12.5% of them. All the infections were significantly more frequent in the group of HIV infected women (p=0.04, 0.02 e 0.04, respectively). CONCLUSIONS: vulvovaginitis is more frequent in HIV infected women.