Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):175-183
DOI 10.1590/S0100-72032012000400007
PURPOSE: To associate the quality of life with the nutritional status of climacteric women. METHODS: This was a cross-sectional study on a sample of 200 climacteric women aged 40 to 65 years who responded to a 24-hour food recall and to questions about socioeconomic factors and current, previous and family medical history. Body mass index (BMI), waist circumference (WC) and waist-hip ratio were used for anthropometric evaluation. To assess the quality of life, we applied the MRS-menopause rating scale. RESULTS: The average BMI and waist circumference were 30.1 kg/m² (obesity grade 1) and 99 cm (very increased risk for cardiovascular disease), respectively. Increased protein consumption and decreased fiber, calcium and vitamin D intake were detected. The most prevalent disease was hypertension, 48.5% of the women studied were taking medication for cardiovascular disease and 23% were taking antidepressant medications. Regarding quality of life, significant results related to BMI as well as blood pressure were found. CONCLUSIONS: A nutritional intervention aiming to correct or improve food consumption and anthropometric profile may result in health benefits for climacteric women. The prevalence of obesity, associated with a poorer quality of life, morbidity and mortality underscores the need for a feeding re-education program during the climacteric.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):170-174
DOI 10.1590/S0100-72032012000400006
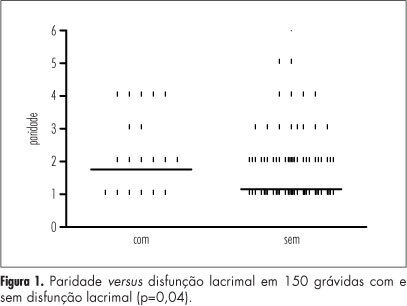
PURPOSE: To assess the prevalence of lacrimal dysfunction during pregnancy comparing it to non-pregnant women and to correlate these findings with obstetric history. METHODS: We interviewed 150 pregnant and 150 non-pregnant women for symptoms of dry eyes and obstetric history. Both groups underwent Schirmer I testing and responded to a questionnaire on dry eye symptoms. Patients with collagen diseases, medications associated with dryness of mucous membranes, hepatitis C infection and AIDS, previous intraocular inflammation and eye surgery were excluded. Data were analyzed by the Χ2 and Fisher tests when the data were nominal and by the Student´s t-test and Mann-Whitney test when numerical. The level of significance was set at 5%. RESULTS: The two groups did not differ in symptoms of lacrimal dysfunction. The results of Schirmer's test were equal in both groups for the right eye (p=0.3) and left eye (p=0.3). However, pregnant women had a higher prevalence of at least one dry eye (p=0.004). The occurrence of dry eye in both groups (patients and controls) was associated with a greater number of full-term pregnancies/patient (p=0.04) but not with pregnancy time (p=0.5) or number of abortions (p=0.9). CONCLUSIONS: Pregnant women suffer more from lacrimal dysfunction than non pregnant women; in both groups the prevalence of tear dysfunction is more elevated in women with higher parity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):164-169
DOI 10.1590/S0100-72032012000400005
PURPOSE: To describe the maternal and perinatal outcomes after the use of 12.5 µg of sublingual misoprostol for labor induction in women with term pregnancy and a live fetus. METHODS: We conducted a multicenter, open and non-randomized clinical trial during the period from July to December 2009. We included 30 pregnant women with an indication for labor induction at term, carrying a live fetus, with a Bishop score of six or less, cephalic presentation, estimated fetal weight of less than 4,000 g and an amniotic fluid index greater than five. We excluded women with a previous uterine scar, non-reassuring fetal status, congenital anomalies, multiple pregnancy, intrauterine growth restriction, genital bleeding, and contraindications of vaginal delivery. A tablet of 12.5 µg sublingual misoprostol was administered every six hours, until the beginning of labor, with the maximum of eight doses. RESULTS: Labor was successfully induced in 90% of pregnant women. The mean interval between the first dose and the onset of uterine contractions and delivery was 14.3±11.7 hours and 25.4±13 hours, respectively. The frequency of vaginal delivery was 60%. Uterine tachysystole occurred in two pregnant women, being reversed in both cases without the need for cesarean section. Meconium-stained amniotic fluid was observed in four patients, and an Apgar score of less than 7 at five minutes in only one newborn. CONCLUSION: Maternal and perinatal outcomes were favorable after induction of labor with sublingual misoprostol at a dose of 12.5 µg every six hours. However, controlled trials are needed to compare this regimen with other doses and routes of administration.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):128-132
DOI 10.1590/S0100-72032012000300007
PURPOSE: To evaluate the importance of the oral glucose tolerance test for the diagnosis of glucose intolerance (GI) and type 2 diabetes mellitus (DM-2) in women with PCOS. METHODS: A retrospective study was conducted on 247 patients with PCOS selected at random. The diagnosis of GI was obtained from the two-hour oral glucose tolerance test with 75 g of glucose according to the criteria of the World Health Organization (WHO) (GI: 120 minutes for plasma glucose >140 mg/dL and <200 mg/dL), and the diagnosis of DM-2 was obtained by both the oral glucose tolerance test (DM: 120 minutes for plasma glucose >200 mg/dL) and fasting glucose using the criteria of the American Diabetes Association (impaired fasting glucose: fasting plasma glucose >100 and <126 mg/dL; DM: fasting glucose >126 mg/dL). A logistic regression model for repeated measures was applied to compare the oral glucose tolerance test with fasting plasma glucose. ANOVA followed by the Tukey test was used for the analysis of the clinical and biochemical characteristics of patients with and without GI and/or DM-2. A p<0.05 was considered statistically significant. RESULTS: PCOS patients had a mean age of 24.8±6.3, and body mass index (BMI) of 18.3 to 54.9 kg/m² (32.5±7.6). The percentage of obese patients was 64%, the percentage of overweight patients was 18.6% and 17.4% had healthy weight. The oral glucose tolerance test identified 14 cases of DM-2 (5.7%), while fasting glucose detected only three cases (1.2%), and the frequency of these disorders was higher with increasing age and BMI. CONCLUSIONS: The results of this study demonstrate the superiority of the oral glucose tolerance test in relation to fasting glucose in diagnosing DM-2 in young women with PCOS and should be performed in these patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):122-127
DOI 10.1590/S0100-72032012000300006
PURPOSE: To compare the diagnostic accuracy of sonohysterography (HSN) and conventional transvaginal ultrasound (USG) in assessing the uterine cavity of infertile women candidate to assisted reproduction techniques (ART). METHODS: Comparative cross-sectional study with 120 infertile women candidate to ART, assisted at Centro de Reprodução Assistida (CRA) of Hospital Regional da Asa Sul (HRAS), Brasília - DF, from August 2009 to November 2010. Sonohysterography was performed with saline solution infusion in a close system. The sonohysterography finding was compared to previous USG results. The uterine cavity was considered abnormal when the endometrium was found to be thicker than expected during the menstrual cycle and when an endometrial polyp, a submucous myoma and an abnormal shape of the uterine cavity were observed. The statistical analysis was done using absolute frequencies, percentage values and the χ², with the level of significance set at 5%. RESULTS: HSN revealed that 92 (76.7%) infertile women candidate to ART had a normal uterine cavity, while 28 (23.3%) had the following abnormalities: 15 polyps (12.5%), 9 cases of abnormal shape of the uterine cavity (7.5%), 6 submucous myomas (5%), 4 cases of inadequate endometrial thickness for the menstrual cycle phase (3.3%), and 2 cases of uterine septum (1.7%); 5 women presented more than one abnormality (4.2%). While USG showed alteration in the cavity only in 5 (4.2%) women, the sonohysterography confirmed 4 out of the 5 abnormalities shown by USG and detected an abnormal uterine cavity in 24 other women, who had not been detected by USG. This means that sonohysterography was able to detect more abnormalities in the uterine cavity than USG, with a statistically significant difference (p=0.002). CONCLUSION: The sonohysterography was more accurate than USG in the assessment of the uterine cavity of this cohort of infertile women candidate to ART. The sonohysterography can be easily incorporated into the investigation of these women and contribute to reducing embryo implantation failures.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):118-121
DOI 10.1590/S0100-72032012000300005
PURPOSE: To report the use of colpotomy for the treatment of ectopic pregnancies. METHODS: This was a retrospective cross-sectional study conducted on all women hospitalized with a clinical-laboratory suspicion of ectopic pregnancy who did not fulfill the criteria for drug treatment with methothrexate, during the period from February 2007 to August 2008. Demographic variables, gynecologic history and characteristics associated with treatment were obtained by reviewing the medical records. RESULTS: Eighteen women were included in the study. Mean age was 27±5.2 years. All patients presented ruptured ectopic pregnancy and all were submitted to partial salpingectomy. Surgical time ranged from 30 to 120 minutes (mean: 64.5 minutes) calculated from the moment when the patient entered the operating room to the moment when she left it. No patient presented postoperative infection. Mean time of hospitalization was 40±14.3 hours. The medications used during the postoperative period were similar in all cases, being based on nonsteroid anti-inflammatory drugs, dipyrone, paracetamol and meperidine, as needed. The diet was reintroduced 8 hours after the end of surgery. CONCLUSIONS: The use of colpotomy in the treatment of ectopic pregnancy showed good results, with the absence of important complications and a short hospitalization time. The basic surgical instruments needed for this procedure are relatively common to all hospitals, and the surgical technique is reproducible.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):113-117
DOI 10.1590/S0100-72032012000300004
PURPOSE: To determine the association between maternal complications and type of delivery in women with heart disease and to identify the possible clinical and obstetrical factors implicated in the determination of the route of delivery. METHODS: This was a retrospective and descriptive study of the medical records of pregnant women with heart disease admitted to a tertiary reference hospital in the municipality of Fortaleza, Ceará, from 2006 to 2007. The study population included all pregnant women with an antepartum diagnosis of heart disease admitted for delivery, while women who received a diagnosis of heart disease after delivery were excluded, regardless of age and gestational week. A semi-structured questionnaire regarding sociodemographic, clinical and obstetrical variables was used. A descriptive analysis was first performed based on simple frequencies and proportions of the sociodemographic variables. Next, possible associations between clinical and obstetrical aspects and type of delivery were analyzed, with the verification of association between maternal complications and type of delivery. The Fisher exact test was applied for this analysis, with the level of significance set at p<0.05. The collected data were processed and analyzed using the Epi-InfoTM software version 6.04 (Atlanta, USA). RESULTS: Seventy-three pregnant women with heart disease were included in the study. Interatrial communication was the condition most frequently observed among congenital diseases (11.0%) and mitral calcification among the acquired ones (24.6%). The proportion of cesarean deliveries was higher than the proportion of vaginal deliveries, except for women with acquired heart disease. An association was detected between type of heart disease and type of delivery (p=0.01). There were 13 cases of maternal complications (17.8%). Among them, ten (76.9%) occurred during cesarean section and three during vaginal delivery. No association mas detected between maternal complications and type of delivery in pregnant women with heart disease (p=0.74). CONCLUSIONS: There was no association between the occurrence of maternal complications and route of delivery among pregnant women with heart disease.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):107-112
DOI 10.1590/S0100-72032012000300003
PURPOSE: To analyze the influence of maternal nutritional status, weight gain and energy consumption on fetal growth in high-risk pregnancies. METHODS: A prospective study from August 2009 to August 2010 with the following inclusion criteria: puerperae up to the 5th postpartum day; high-risk singleton pregnancies (characterized by medical or obstetrical complications during pregnancy); live fetus at labor onset; delivery at the institution; maternal weight measured on the day of delivery, and presence of medical and/or obstetrical complications characterizing pregnancy as high-risk. Nutritional status was assessed by pregestational body mass index and body mass index in late pregnancy, and the patients were classified as: underweight, adequate, overweight and obese. A food frequency questionnaire was applied to evaluate energy consumption. We investigated maternal weight gain, delivery data and perinatal outcomes, as well as fetal growth based on the occurrence of small for gestational age and large for gestational age neonates. RESULTS: We included 374 women who were divided into three study groups according to newborn birth weight: adequate for gestational age (270 cases, 72.2%), small for gestational age (91 cases, 24.3%), and large for gestational age (13 cases, 3.5%). Univaried analysis showed that women with small for gestational age neonates had a significantly lower mean pregestational body mass index (23.5 kg/m², p<0.001), mean index during late pregnancy (27.7 kg/m², p<0.001), and a higher proportion of maternal underweight at the end of pregnancy (25.3%, p<0.001). Women with large for gestational age neonates had a significantly higher mean pregestational body mass index (29.1 kg/m², p<0.001), mean index during late pregnancy (34.3 kg/m², p<0.001), and a higher proportion of overweight (30.8%, p=0.02) and obesity (38.5%, p=0.02) according to pregestational body mass index, and obesity at the end of pregnancy (53.8%, p<0.001). Multivariate analysis revealed the index value during late pregnancy (OR=0.9; CI95% 0.8-0.9, p<0.001) and the presence of hypertension (OR=2.6; 95%CI 1.5-4.5, p<0.001) as independent factors for small for gestational age. Independent predictors of large for gestational age infant were the presence of diabetes mellitus (OR=20.2; 95%CI 5.3-76.8, p<0.001) and obesity according to body mass index during late pregnancy (OR=3.6; 95%CI 1.1-11.7, p=0.04). CONCLUSION: The maternal nutritional status at the end of pregnancy in high-risk pregnancies is independently associated with fetal growth, the body mass index during late pregnancy is a protective factor against small for gestational age neonates, and maternal obesity is a risk factor for large for gestational age neonates.