Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):102-106
DOI 10.1590/S0100-72032012000300002
PURPOSE: To assess the prevalence of obstetric risk factors and their association with unfavorable outcomes for the mother and fetus. METHODS: A longitudinal, descriptive and analytical study was conducted on 204 pregnant women between May 2007 and December 2008. Clinical and laboratory assessments followed routine protocols. Risk factors included socio-demographic aspects; family, personal and obstetric history; high pre-gestational body mass index (BMI); excessive gestational weight gain and anemia. Adverse outcomes included pre-eclampsia (4.5%), gestational diabetes mellitus (3.4%), premature birth (4.4%), caesarian birth (40.1%), high birth weight (9.8%) and low birth weight (13.8%). RESULTS: The average age was 26±6.4 years; the mothers were predominantly non-white (84.8%), 51.8% had incomplete or complete secondary level schooling, 67.2% were in a stable marital relationship and 51.0% had a regular paid job; 63.7% were admitted to the prenatal clinic during the second trimester and 16.7% during the first, with 42.6% being primiparous. A past history of chronic hypertension was reported by 2.9%, pre-eclampsia by 9.8%, excessive gestational weight gain by 15.2% and former gestational diabetes mellitus by 1.0%. In the current pregnancy, elevated pre-gestational BMI was found in 34.6%; 45.5% presented with excessive gestational weight gain, 25.3% with anemia and 47.3% with dyslipidemia. Of the 17.5% of cases with altered blood glucose, gestational diabetes mellitus was confirmed in 3.4% and proteinuria occurred in 16.4% of all cases. Adverse maternal fetal outcomes included pre-eclampsia (4.5%), gestational diabetes mellitus (3.4%), premature birth (4.4%), caesarean birth (40.1%) and high and low birth weight (9.8% and 13.8%, respectively). Independent predictors of adverse maternal fetal outcomes were identified by Poisson multivariate regression analysis: pre-gestational BMI>25 kg/m² was a predictor for pre-eclampsia (RR=17.17; 95%CI 2.14-137.46) and caesarian operation (RR=1.79; 95%CI 1.13-2.85), previous caesarean was a predictor for present caesarean operation (RR=2.28; 95%CI 1.32-3.92) and anemia and high gestational weight gain were predictors for high birth weight (RR=3.38; 95%CI 1.41-8.14 and RR=4.68; 95%CI 1.56-14.01, respectively). CONCLUSION: Pre-gestational overweight/obesity, previous caesarean, excessive weight gain and anemia were major risk factors for pre-eclampsia, caesarean operations and high birth weight.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):92-96
DOI 10.1590/S0100-72032012000200009
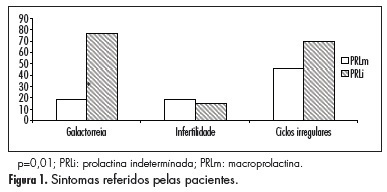
PURPOSE: To characterize patients with indeterminate values of hyperprolactinemia (PEG test for the identification of macroprolactinemias with recovery between 30 and 65%) (PRLi) or macroprolactinemia (PRLm), in relation to clinical characteristics, such as the presence or absence of symptoms, as well as their intensity and variation, and the presence or absence of central nervous system tumors. METHODS: This is a cross-sectional retrospective survey of records of 24 patients with hyperprolactinemia, in reproductive ages, with prolactin >25 ng/dL. Eleven women with PRLm and 13 with PRLi were included. Records from the two groups were extracted for analysis: age, parity, body mass index, presence of galactorrhea, infertility, and central nervous system tumor. Anthropometrics data were expressed as mean and standard deviation. To compare groups regarding the presence of central nervous system tumor, galactorrhea, as well as infertility we used the Student's t-test. RESULTS: Galactorrhea was more prevalent in patients with PRLi (p=0.01). Seventy percent of women with PRLi presented pituitary tumor (microprolactinoma), whereas this finding was evident in 17% of the PRLm Group (p=0.04). Among the patients with and PRLm PRLi, nine were not investigated with the image of the central nervous system because they have low levels of prolactin (five carriers and four PRLm PRLi). There were no significant differences regarding the occurrence of infertility or irregular menstrual cycles between groups. DISCUSSION: Women with intermediate hyperprolactinemia present more galactorrhea symptoms as well as central nervous system tumors than women with macroprolactinemia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):86-91
DOI 10.1590/S0100-72032012000200008
PURPOSE: To evaluate the actions of the "Um Beijo Pela Vida" Program developed in a Brazilian Northeast city to increase adherence to breast cancer screening by women registered by the Brazilian Family Health Strategy for breast cancer screening. METHODS: A quantitative approach was used to evaluate the coverage of screening actions for aged 40 years-old or more. Community workers from the nine Family Health Teams of the town carried out an active search. The percentage of eligible women who were screened for breast cancer by clinical breast examination or mammography, mammogram classification according to BI-RADS®, women screened who were referred for further testing and treatment, and the number of breast cancers detected were collected by means of a structured questionnaire, analyzed with the EPI-INFO TM software and compared to previously defined patterns. RESULTS: 3,608 women were included, corresponding to 68.4% of the target population registered in the Brazilian Family Health Strategy. Coverage rates of clinical breast examination for women aged 40 to 49 years-old and of mammograms for women aged 50 to 69 years-old were 58.9 and 56.7%, respectively. All women with highly suspicious mammographic lesions were submitted to fine needle aspiration or core biopsy (100%). Six new cases of cancer were detected and 80% of the standards established for this evaluation were carried out. CONCLUSIONS: The evaluation of the actions of the Program suggests its adequacy considering the degree of fulfillment of the previously defined requirements.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):80-85
DOI 10.1590/S0100-72032012000200007
PURPOSE: To evaluate the clinical outcomes after a minimum period of 5 years of follow-up of patients with abnormal uterine bleeding of benign etiology who underwent endometrial ablation, analyzing the success rate of treatment defined as patient satisfaction and improvement in uterine abnormal bleeding, as well as late complications and factors associated with recurrence of symptoms. METHODS: A cross-sectional survey was conducted after a minimum period of 5 years after surgery in patients who underwent the procedure between 1999 and 2004. We analyzed the following data: age at the time of surgery, immediate and late complications and associated factors. Logistic regression with Odds Ratio (OR) calculation was performed to evaluate possible associations between the success rate of surgery and the analyzed variables. RESULTS: A total of 114 patients underwent endometrial ablation between March 1999 and April 2004. The median follow-up was 82 months. The logistic regression model allowed the correct prediction of the success of endometrial ablation in 80.6% of cases. Age was directly related to the success of the procedure (OR=1.2; p=0.003) and previous tubal ligation showed a negative association with the success of endometrial ablation (OR=0.3; p=0.049). Among the patients with treatment failure, 21 (72.4%) underwent hysterectomy. In one of the hysterectomy cases, hydro/hematosalpinx was confirmed by the anatomopathological exam, characterizing the postablation-tubal sterilization syndrome. CONCLUSION: Endometrial ablation has proven to be a worthwhile treatment option, maintaining high rates of patient satisfaction, even over long-term follow-up. The age at endometrial ablation influenced the therapeutic success. Further studies are needed to evaluate the factors that may influence the future indication for the procedure in selected cases.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):74-79
DOI 10.1590/S0100-72032012000200006
PURPOSE: To analyze the prevalence of insulin resistance, according to different biochemical and anthropometric measurements in women with polycystic ovary syndrome. METHODS: A total of 189 patients with polycystic ovary syndrome were retrospectively analyzed. Insulin resistance diagnosis was performed using fasting insulin, HOMA-IR, QUICKI, insulin sensibility index and glucose/fasting insulin ratio. Body mass index and lipid accumulation product were used. Data were analyzed statistically by descriptive statistics, ANOVA, Tukey post-test, and Pearson's correlation. RESULTS: The polycystic ovary syndrome patients had a mean age of 24.9±5.2 and a mean body mass index of 31.8±7.6. The percentage of obese patients was 57.14%. Among the methods of insulin resistance investigation, the insulin sensibility index was the technique that most detected (56.4%) the presence of insulin resistance in women with polycystic ovary syndrome. The insulin resistance was detected in 87% of obese patients. The fasting glucose/fasting insulin ratio and insulin sensibility index were strongly correlated with lipid accumulation product. CONCLUSION: The prevalence of insulin resistance varied according to the method used, and it was greater the higher the body mass index. Lipid accumulation product was also related to insulin resistance.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):69-73
DOI 10.1590/S0100-72032012000200005
PURPOSE: To identify the knowledge and awareness of health professionals regarding the Brazilian legislation on induced abortion. METHODS: Unidentified sealed envelopes containing the questionnaires were sent to all professionals (n=149) working in the Obstetrics Department of a university hospital and public hospital at the periphery of São Paulo (SP), Brazil. A total of 119 professionals responded to the questionnaire. The 0.05 confidence interval and the Fisher exact test and χ² test were used for data analysis. RESULTS: Of the respondents, 48.7% were physicians, 33.6% were nursing professionals and 17.6% were professionals from other fields (psychologists, nutritionists, physiotherapists, laboratory technicians and administrators). There was a significant difference (p=0.01) in the proportion of professionals who believe that abortion for non-lethal fetal malformation and due to unplanned pregnancies should be included in the Brazilian legislation. It was observed that the knowledge about the law and the description of the circumstances allowed by law on abortion was significantly different when comparing health professionals (p=0.01). When asked about the situations in which Brazilian law allows abortion, 32.7% of physicians, 97.5% of nursing professionals and 90.5% of other professionals were unaware of the law. CONCLUSION: This study demonstrated the lack of of knowledge of Brazilian law among health professionals, to a lesser extent among obstetricians and a to a greater extent among nursing professionals. Attitudes of discrimination and prejudice were observed regarding the care provided to women who induce an abortion.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):63-68
DOI 10.1590/S0100-72032012000200004
PURPOSE: To evaluate the susceptibility to toxoplasmosis in pregnant women in the public health service from two cities in the western region of Paraná, Brazil. METHODS: Four thousand twenty-two pregnant women were evaluated for anti-Toxoplasma gondii IgG and IgM by ELISA and MEIA. Seronegative pregnant women repeated the serology in the second and third trimester of pregnancy. Neonatal screening of 27 newborns was also performed in one of the cities to detect IgM anti- Toxoplasma gondii by fluorometry. All pregnant women answered an epidemiological questionnaire to analyze the factors associated with the risk of infection by Toxoplasma gondii. For statistical analysis, the presence of IgG anti-Toxoplasma gondii was considered as the dependent variable and the variables contained in the epidemiological questionnaire as the independent ones. RESULTS: The prevalence of anti-Toxoplasma gondii IgG in pregnant women was 59.8 and 60.6%. In one of the cities, the variables associated with the presence of IgG antibodies were low educational level and more than one pregnancy. There was no association with other factors studied such as consumption of raw or undercooked meat, consumption of raw vegetables, consumption of colonial salami, handling soil or sand, the presence of a home vegetable garden and cats in the household. In the other city there was no statistical association with the variables studied. No case of acute infection and no seroconversion were confirmed in either city. None of the infants evaluated were positive for toxoplasmosis. CONCLUSION: Toxoplasmosis is common in pregnant women attended by the public health service in the region studied and 40% of them are susceptible to the infection. These data reinforce the need to keep the screening program in these cities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):56-62
DOI 10.1590/S0100-72032012000200003
PURPOSE: To describe the characteristics of pregnancies complicated by maternal syphilis and fetal death. METHODS: Retrospective descriptive study performed by reviewing the medical records of 48 pregnant women with maternal syphilis and fetal death outcome admitted to Hospital Geral de Nova Iguaçu, Baixada Fluminense, State of Rio de Janeiro, during the period from 2005 to 2008. Birth weight >500 g and fetal death documented by Death Certificate were the inclusion criteria. The following aspects were analyzed: sociodemographic factors, reproductive history, aspects of the current pregnancy, prenatal care, Venereal Disease Research Laboratory (VDRL) testing, and other gestational conditions, in addition to syphilis. The fetal deaths were classified as maternal, placental or fetal. Percentage, mean, standard deviation (SD), maximum and minimum values were reported. RESULTS: The mean maternal age was 22.7 years (SD=0.9 years), and at least 50% of the patients had low educational level. At hospital admission, 68.8% of the subjects were in the third trimester, with a mean gestational age of 29.2 weeks (SD=0.5), and more than 50% were in labor. The vast majority of fetal deaths (93%) occurred before maternal hospitalization. Among the patients who received prenatal care (54.2%), 30.8% had no VDRL test, 30.8 and 15.4% had a reactive and non-reactive result, respectively, and none had more than one prenatal VDRL test. At the time of childbirth, most of the mothers (95.8%) carried out VDRL testing. Overall, the VDRL titers varied from 1:1 to 1:512, with predominant values >1:4 (91.7%). In 23% of cases other clinical conditions related to fetal death, in addition to syphilis, were found. CONCLUSIONS: The infection was the main clinically identified cause of fetal death in this patient series. Fetal death occurred during the preterm period and in the presence of high titers of maternal infection, suggesting recent syphilis infection.