Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(5):235-242
DOI 10.1590/S0100-72032012000500008
PURPOSE: To evaluate the survival and complications associated with prematurity of infants with less than 32 weeks of gestation. METHODS: It was done a prospective cohort study. All preterm infants with a gestational age between 25 and 31 weeks and 6 days, born alive without congenital anomalies and admitted to the NICU between August 1st, 2009 and October 31st, 2010 were included. Newborns were stratified into three groups: G25, 25 to 27 weeks and 6 days; G28, 28 to 29 weeks and 6 days; G30, 30 to 31 weeks and 6 days, and they were followed up to 28 days. Survival at 28 days and complications associated with prematurity were evaluated. Data were analyzed statistically by c² test, analysis of variance, Kruskal-Wallis test, odds ratio with confidence interval (CI) and multiple logistic regression, with significance set at 5%. RESULTS: The cohort comprised 198 preterm infants (G25=59, G28=43 and G30=96). The risk of death was significantly higher in G25 and G28 compared to G30 (RR=4.14, 95%CI 2.23-7.68 and RR=2.84, 95%CI: 1.41-5.74). Survival was 52.5%, 67.4% and 88.5%, respectively. Survival was greater than 50% in preterm >26 weeks and birth weight >700 g. Neonatal morbidity was inversely proportional to gestational age, except for necrotizing enterocolitis and leukomalacia, which did not differ among groups. Logistic regression showed that pulmonary hemorrhage (OR=3.3, 95%CI 1.4-7.9) and respiratory distress syndrome (OR=2.5, 95%CI 1.1-6.1) were independent risk factors for death. There was a predominance of severe hemorrhagic brain lesions in G25. CONCLUSION: Survival above 50% occurred in infants with a gestational age of more than 26 weeks and >700 g birth weight. Pulmonary hemorrhage and respiratory distress syndrome were independent predictors of neonatal death. It is necessary to identify the best practices to improve the survival of extreme preterm infants.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):147-152
DOI 10.1590/S0100-72032012000400002
PURPOSE: To assess medication adherence therapeutic during pregnancy in a sample of Brazilian women during the post-partum period. METHODS: We conducted a cross-sectional study in the obstetric unit of a university hospital, Brazil, between August and November 2010. We recruited patients aged 18 years or more, with a gestational age of more than 22 weeks whose newborns weighed more than 500 g. Patients were excluded if they used sedatives or other mind-altering drugs. Data were collected after labor using a structured questionnaire containing questions about sociodemographic characteristics, medication use, number of previous pregnancies, contraceptive methods, prenatal care, and medication adherence. Medication adherence was assessed using the four-item Morisky medication adherence scale - MMAS-4, groups were compared by the Fisher exact Test and Kruskal-Wallis Test and Χ2 de Pearson Test. RESULTS: Mean age was 22.5 years (SD=6.5), and 53.8% of the pregnant women had initiated prenatal care during the first trimester of pregnancy. Of the 130 patients interviewed, 96.9% had used at least one prescribed drug during pregnancy, with an average of 2.8 drugs per patient. The major classes prescribed were antianemics (55.1%), analgesics, anti-inflammatories, and antipyretics (19.0%) and anti-infectives (7.2%). 71.6% took two to four drugs. Only 19.2% of patients were considered adherent. The variables that showed a negative influence on adherence were: higher level of education, having one's own income, earlier prenatal care and previous abortion. CONCLUSION: Our findings indicate that, although most of the patients used prescribed drugs during pregnancy, the rate of medication adherence was low, which indicates the need for further investigation about the impact of non-adherence during pregnancy and its causes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(5):221-227
DOI 10.1590/S0100-72032012000500006
PURPOSE: To evaluate the thickness of the lower uterine segment by transvaginal ultrasound in a group of non-pregnant women and to describe the morphologic findings in the scar of those submitted to cesarean section. METHODS: A retrospective study of 155 transvaginal ultrasound images obtained from premenopausal and non-pregnant women, conducted between January 2008 and November 2011. the subjects were divided into three groups: women who were never pregnant (Control Group I), women with previous vaginal deliveries (Control Group II) and women with previous cesarean section (Observation Group). We excluded women with a retroverted uterus, intrauterine device users, pregnant women and those with less than one year of tsince the last obstetrical event. The data were analyzed statistically with Statistica®, version 8.0 software. ANOVA and LSD were used to compare the groups regarding quantitative variables and the Student's t-test was used to compare the thickness of the anterior and posterior isthmus. The Spearman correlation coefficient was calculated to estimate the association between quantitative variables. P values <0.05 were considered statistically significant. RESULTS: There was significant difference between the thickness of the anterior and posterior isthmus only in the group of women with previous cesarean section. Comparing the groups two by two, no significant differences between the thickness of the anterior and posterior isthmus were observed in the Control Groups, but this difference was significant when we compared the Observation Group with each Control Group. In the Observation Group, no correlation was found between the thickness of the isthmus and the number of previous cesarean deliveries or the time elapsed since the last birth. A niche was found in the cesarean scar in 30.6% of the women in the Observation Group, 93% of whom complained of post-menstrual bleeding. CONCLUSION: The relationship between the thickness of the anterior and posterior wall of the lower uterine segment by transvaginal ultrasound is a suitable method for the evaluation of the uterine lower segment in women with previous cesarean sections.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(5):228-234
DOI 10.1590/S0100-72032012000500007
PURPOSE: To evaluate habits of sun exposure and sun protection of pregnant women in a public hospital, to assess orientation about photo protection during the prenatal care, and to detect the presence of melasma and its impact on their quality of life. METHODS: A descriptive cross sectional study conducted among women of 18 years old and older, after delivery, who participated in a program of prenatal care in the South Region of Brazil. The sample was non-probabilistic by convenience. Data collection occurred from July to August 2011 through direct interview using a structured questionnaire to obtain personal information and photo protection habits during pregnancy, skin assessment and photographic record of lesions through informed consent. The skin was classified per Fitzpatrick's phototypes and the melasma was diagnosed clinically. In the patients with melasma, the MELASQoL-PB version was applied. The analysis was performed using Statistica®, version 8.0, and the significance level of p<0.05. RESULTS: In the sample (109 mothers) predominated white women (60.6% phototype III), young (average age 24.4 years SD=6.1) and housewives (59.6%). The majority (80%) stayed exposed to sunlight for 1-2 hours per day between 10 am and 3 pm, and from those (72%) did not apply any photoprotection due to lack of sunscreen habit. Other physical means of sun protection were used by 15% of these patients. Information during prenatal care about the risks of sun exposure was reported by 34% of the mothers interviewed. There was a trend toward a significant association between prenatal guidance and daily use of sunscreen (p=0.088). About 20% of mothers had melasma. The average score MELASQol-PB (25) showed a negative impact on quality of life of these patients. CONCLUSION: In these women, sun exposure occurred at inappropriate times, without proper guidance and without the use of an effective sunscreen. The mothers with melasma complained about the appearance of their skin, frustration and embarrassment.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(5):215-220
DOI 10.1590/S0100-72032012000500005
PURPOSE: To evaluate factors associated with morbidities among Brazilian women aged 40-65 years and with 11 or more years of schooling. METHODS: A secondary analysis of a cross-sectional population-based study was conducted, using an anonymous self-report questionnaire completed by 377 women. Were evaluated, with this instrument, some morbidities (hypertension, diabetes, insomnia and depression) and sociodemographic, behavioral, clinical and reproductive factors. The association between morbidities and independent variables was evaluated by the Χ2 test. Multiple logistic regression analysis with stepwise selection criteria was used to select the major factors associated with morbid conditions. RESULTS: In the multiple regression analysis, insomnia was associated with bad/fair self-perception of health (OR=2.3) and nervousness (OR=5.1). Depression was associated with bad/fair self-perception of health (OR=3.7) and bad/poor leisure (OR=2.8). Hypertension was associated with obesity (OR=3.1) and being in postmenopausal (OR=2.6). Diabetes was associated with age above 50 years (OR=3.9) and obesity (OR=12.5). CONCLUSIONS: The prevalence of morbidities was high and a worse self-perception of health and obesity were the main factors associated with morbidity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(5):209-214
DOI 10.1590/S0100-72032012000500004
PURPOSE: To assess the prevalence of bacterial vaginosis and to compare the accuracy of testing pH and KOH with the Nugent gradient, the gold standard for the diagnosis of bacterial vaginosis (BV) in asymptomatic and symptomatic pregnant women at low risk. METHODS: We conducted a cross-sectional study on 321 pregnant women with gestational age between 14 and 26 weeks, 218 of them asymptomatic and 103 with vaginal complaints suggestive of bacterial vaginosis. All women were assessed by the criteria of Nugent and subjected to the measurement of vaginal pH and to the 10% KOH test. The Kappa coefficient was used to evaluate the methods in terms of diagnostic agreement. RESULTS: Most patients were adolescents (mean age 21.0±5.6 years), nulliparous and mulattos. The prevalence of bacterial vaginosis was 33.3% as estimated by the pH and KOH method and 35.5% by the Nugent method. Excellent agreement of the methods was found among asymptomatic pregnant women, with 72.5% of them showing negative results to both tests, which resulted in a high Kappa coefficient (k=0.82). The group of symptomatic women showed 49.5% positivity to both diagnostic methods, with excellent agreement (k=0.74). CONCLUSION: The prevalence of bacterial vaginosis determined by both the pH and KOH method and the Nugent score was high. The pH and KOH method can diagnose bacterial vaginosis as accurately as the Nugent criterion.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):184-188
DOI 10.1590/S0100-72032012000400008
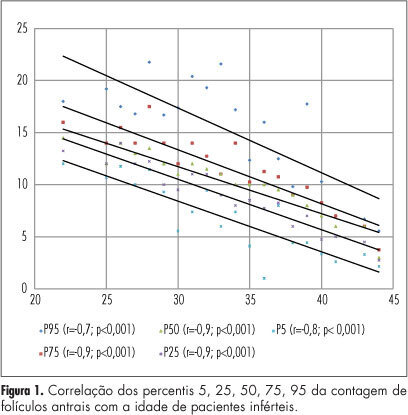
PURPOSE: To produce age-related nomograms for ovarian antral follicle count (AFC) in infertile women. METHODS: It was done a cross-sectional study of patients attended in the center of assisted reproduction Fêmina, from March 2010 to October 2011. The patients were submitted to transvaginal ultrasonography from day 2 to day 4 of their menstrual period. Patients included were between 21 to 45 years old, with regular menses, two healthy ovaries, without any evidence of endocrinopathies and who gave written informed consent. Patients excluded were smokers, with galactosemia or ovarian cysts, with antecedents of liver disease, ovarian surgeries or who were treated with chemotherapy or radiotherapy. In order to check the evolution of the AFC in relation to patient age, we used the 5th, 25th, 50th, 75th and 95th percentiles. Linear regression was carried out using these percentiles, permitting us to determine the effect of age on the CFA. RESULTS: A total of 172 patients with a mean age of 32.7 years were included in the trial. The male and tubal factors were the main causes of infertility, accounting for 65% of cases. The age-related nomogram for the 5th, 25th, 50th, 75th and 95th percentiles of AFC revealed that changes were best fitted by a linear function. The percentiles that showed the highest correlations were 25 (r=-0.9; p<0.001), 50 (r=-0.9; p<0.001) and 75 (r=-0.9; p<0.001). CONCLUSION: A nomogram was constructed correlating age with the different AFC percentiles in infertile women without endocrinopathies. This showed a linear pattern of decline in AFC with age in all percentiles. These nomograms could provide a reference guide for the clinician. However, future validation, with longitudinal data, still is needed.