Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):278-284
DOI 10.1590/S0100-72032012000600007
PURPOSE: To evaluate the anatomical distribution of deep infiltrating endometriosis (DIE) lesions in a sample of women from the South of Brazil. METHODS: A prospective study was conducted on women undergoing surgical treatment for DIE from January 2010 to January 2012. The lesions were classified according to eight main locations, from least serious to worst: round ligament, anterior uterine serosa/vesicouterine peitoneal reflection, utero-sacral ligament, retrocervical area, vagina, bladder, intestine, ureter. The number and location of the DIE lesions were studied for each patient according to the above-mentioned criteria and also according to uni- or multifocality. The statistical analysis was performed using Statistica version 8.0. The values p<0.05 were considered statistically significant. RESULTS: During the study period, a total of 143 women presented 577 DIE lesions: uterosacral ligament (n=239; 41.4%), retrocervical (n=91; 15.7%), vagina (n=50; 8.7%), round ligament (n=50; 8,7%), vesico-uterine septum (n=41; 7.1%), bladder (n=12; 2.1%), and intestine (n=83; 14.4%), ureter (n=11; 1.9%). Multifocal disease was observed in the majority of patients (p<0.0001), and the mean number of DIE lesions per patient was 4. Ovarian endometrioma was present in 57 women (39.9%). Sixty-five patients (45.4%) presented intestinal infiltration on histological examination. A total of 83 DIE intestinal lesions were distributed as follows: appendix (n=7), cecum (n=1) and rectosigmoid (n=75). The mean number of intestinal lesions per patient was 1.3. CONCLUSIONS: DIE has a multifocal pattern of distribution, a fact of fundamental importance for the definition of the complete surgical treatment of the disease.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):274-277
DOI 10.1590/S0100-72032012000600006
PURPOSE: This study aimed to evaluate the results of neovaginoplasty by a modified McIndoe-Bannister technique and by the non-surgical Frank technique. METHODS: This retrospective study was conducted on a convenience sample of 25 women with vaginal agenesis undergoing surgical or conservative treatment at an Infant-Pubertal Gynecology Outpatient Clinic. Data were obtained from the medical records. Fifteen women underwent the surgical McIndoe-Bannister modified technique Surgical Group, and 10 women underwent the non-surgical Frank technique Frank Group. The following parameters were considered for comparative analysis between the two samples: vaginometry, surgical and non-surgical complications, and sexual satisfaction after treatment. Sexual satisfaction was assessed by a simple question: How is your sex life? RESULTS: There were differences related to vaginal length before and after performing exercises in both Frank Group (initial vaginal length 2.4±2.0 cm versus 6.9±1.1 cm after treatment, p<0.0001) and Surgical Group (initial vaginal length 0.9±1.4 cm versus 8.0±0.8 cm after treatment, p<0.0001). Increased vaginal length was observed in Surgical Group compared to Frank Group (Frank Group=7.0±0.9 cm versus Surgical Group=8.0±0.8 cm, p=0.0005). Forty percent of Surgical Group women had surgical complications versus no complications with the Frank technique. All women reported to be satisfied with their sexual life. CONCLUSION: The present data indicate that both the surgical and Frank techniques are effective for the treatment of vaginal agenesis, resulting in the construction of a vagina that pewrmits sexual intercourse and sexual satisfaction. The favorable aspects of the Frank technique are related to its low cost and to the low rates of major complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):268-273
DOI 10.1590/S0100-72032012000600005
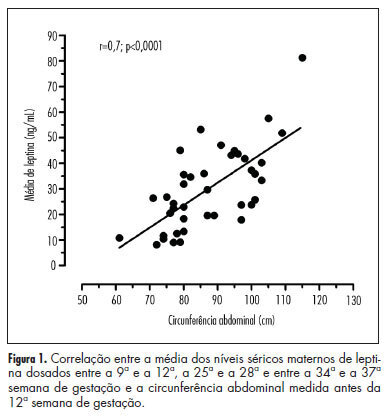
PURPOSE: To evaluate the correlation between maternal waist circumference measured before the 12th week of gestation and serum leptin levels during pregnancy, as well as to compare the leptin levels of women with and without abdominal obesity diagnosed in early pregnancy. METHODS: Prospective study including 40 pregnant women receiving low-risk prenatal care, older than 20 years, nonsmokers, with singleton pregnancies and without chronic disease. Waist circumference was measured before the 12th week and serum leptin levels were measured between the 9th and 12th, 25th and 28th and 34th and 37th weeks of gestation. According to waist circumference measurement, the cohort was divided into two groups: with and without abdominal obesity. The Mann-Whitney and χ² tests were used to assess the differences between groups. The Pearson correlation coeffient was used to assess the association between waist circumference and serum leptin levels during pregnancy. The level of significance was set at p<0.05. RESULTS: The mean weight and body mass index of patients with abdominal obesity (74.4±11.0 kg/28.9±4.1) was higher than that of patients without abdominal obesity (55.6±5.9 kg/21.1±2.4) (p=0.001). The mean leptin levels in pregnant patients with abdominal obesity (41.9±3.5 ng/mL) was higher than in patients without abdominal obesity (23.6±2.7 ng/mL) (p<0.0002). A positive correlation was obtained between the waist circumference measured during the same period and the mean serum leptin levels (r=0.7; p<0.0001). CONCLUSIONS: Waist circumference measured before the 12th week of pregnancy is a valid and simple method to predict the serum leptin levels throughout pregnancy. Pregnant women with abdominal obesity diagnosed before 12th week have higher mean serum leptin levels during pregnancy than those without abdominal obesity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):259-267
DOI 10.1590/S0100-72032012000600004
PURPOSE: To compare the filling out of the prenatal care card of pregnant women at a school-service and other services, as well as to verify the concordance between these records and verbal information provided by the puerperae. METHODS: A two-stage epidemiological, cross-sectional study was performed with stratified sampling, proportional to number of births. In the first stage, the information recorded on the prenatal care card in the school-service was compared to that recorded in units not linked to higher health education in Recife (PE). In the second stage, the information about prenatal care was collected with a semi-structured questionnaire applied to women during the puerperal period. A total of 262 puerperae older than 19 years, who had a prenatal care card at the time of delivery were included in the study from May to July 2008. Data were analyzed statistically by the χ² test, Student´s t-test or Mann-Whitney test, all one-sided to the right, with the level of significance set at 5%. RESULTS: The information more often recorded on the prenatal care card in the school-service was: schooling (86.5 versus 70.3%; p=0.002), marital status, (83.7 versus 70.9%; p=0.01), weight prior to pregnancy (72.1 versus 46.8%; p<0.001), height (62.5 versus 45.6%; p=0.007), and educational practices (76.9 versus 11.4%; p<0.001) and, at other services, only birth weight <2,500 g (15.4 versus 27.2% at the school-service; p=0.02). There were significant discrepancies between data obtained by verbal information and the prenatal care records of the pregnant women. At the school-service, 40.3% of pregnant women received adequate prenatal care versus 20.3% at other units. CONCLUSIONS: In all services, there was a predominance of recorded information directly related to delivery, while information about actions with preventive characteristics during prenatal care was neglected.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):254-258
DOI 10.1590/S0100-72032012000600003
PURPOSE: To determine the frequency of hydatiform mole in tissues obtained by curettage. METHODS: A cross-sectional, prospective and descriptive conducted on patients who underwent curretage due to a diagnosis of abortion or hydatiform mole whose material was sent for pathological examination. We excluded women who did not accept to participate and refused to sign the free informed consent form. We studied the following variables: pathological findings, age, race, number of pregnancies and previous abortions, gestational age at diagnosis, quantitative serum beta fraction of human chorionic gonadotropin and ultrasound findings. The data were compared to the to histological diagnosis, considered to be the gold standard. Data were stored and analyzed in Microsoft Excel® software and the Epi-Info program, version 6.0 (STATCALC) and the results are presented as frequency (percentage) or mean±standard deviation. The χ2 test was used to determine the association between qualitative variables and the level of significance was set at p<0.005. RESULTS: A total of 515 curettage procedures were performed, 446 of which comprised the sample. The frequency of hydatiform mole was 2.2% (ten cases). The mean age of the patients with a mole was 31±10 years, most patients were white and multiparous and had no history of previous abortions, but there was no significant association between these variables. The pregnancy loss occurred early in patients with and without a mole and the most common complaints in both groups were vaginal bleeding and cramps in the lower abdomen. Quantitative determination of human chorionic gonadotropin was performed in 422 cases (413 with and 9 without a hydatiform mole). The levels of the hormone were higher than 100,000 mIU/mL in 1.9% of the patients without a hydatiform mole and in 44.45% of the patients with the disease (p=0.00004). All patients with this hormonal level had an ultrasound suspicion of hydatiform mole and one of them also had a clinical suspicion. A total of 333 patients underwent ultrasound examination. Of the patients with sonographic findings suggestive of molar pregnancy, there was confirmation in five (41.7%) cases. The other seven (58.3%) were false positives. A significant association was found between ultrasound suspected molar pregnancy and disease confirmation by histopathological analysis (p=0.0001). In 50% of cases of hydatiform mole there was no suspicion of the disease according to clinical signs and symptoms, levels of beta fraction of human chorionic gonadotropin or sonographic findings. CONCLUSIONS: The frequency of hydatidiform mole is low and the disease may not be suspected by clinical examination, ultrasonography or the serum level of the beta fraction of human chorionic gonadotropin, requiring pathological examination of tissue obtained by uterine evacuation for diagnosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):248-253
DOI 10.1590/S0100-72032012000600002
PURPOSE: To verify whether women with atypias of undetermined significance and precursor lesions or invasive cervical outcomes were referred to Medium Complexity Units (MCU) following the guidelines recommended by the Brazilian Ministry of Health. METHODS: Retrospective study based on the cytopathological outcomes of users of the Unified Health System, seen at Basic Health Assistance Units (BHAU) and referred to MCUs in the municipality of Goiânia, state of Goiás, from 2005 to 2006. We assessed 832 records according to the recommendations of the Brazilian Ministry of Health, as established by the Brazilian Nomenclature for Cervical Cytopathologic Outcomes and Recommended Clinical Practice. To check the distribution of variables such as reasons for referral, results of colposcopy and histopathology and clinical procedures we calculated absolute and relative frequencies, mean, minimum and maximum values. RESULTS: We understood 72.7% of the referrals were not in accordance with the recommendations of the Ministry of Health. There were 605 women with test results classified as atypical squamous cells of undetermined significance, possibly non-neoplasms, and squamous intraepithelial lesion of low level which were sent to MCU, and of these 71.8% were submitted to colposcopy, and 64.7% had histopathological examination which results were classified as 31.0% with non-neoplasms and 44.6% as NIC I. Out of 211 women with results classified as more severe squamous lesions, 86.3% were submitted to colposcopy and 68.7% of these had histopathological examinations. CONCLUSIONS: The results of this study revealed high rates of inappropriate referrals to MCU, which required a high percentage of unnecessary procedures. The recommendations of the Ministry of Health were followed by BHAU and the majority of women received counseling/treatment as recommended.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):158-163
DOI 10.1590/S0100-72032012000400004
PURPOSE: To verify cervical length using transvaginal ultrasonography in pregnant women between 28 and 34 weeks of gestation, correlating it with the latent period and the risk of maternal and neonatal infections. METHODS: 39 pregnant women were evaluated and divided into groups based on their cervical length, using 15, 20 and 25 mm as cut-off points. The latency periods evaluated were three and seven days. Included were pregnant women with live fetuses and gestational age between 28 and 34 weeks, with a confirmed diagnosis on admission of premature rupture of membranes. Patients with chorioamnionitis, multiple gestation, fetal abnormalities, uterine malformations (bicornus septate and didelphic uterus), history of previous surgery on the cervix (conization and cerclage) and cervical dilation greater than 2 cm in nulliparous women and 3 cm in multiparae were excluded from the study. RESULTS: A <15 mm cervical length was found to be highly related to a latency period of up to 72 hours (p=0.008). A <20 mm cervical length was also associated with a less than 72 hour latency period (p=0.04). A <25 mm cervical length was not found to be statistically associated with a 72 hour latency period (p=0,12). There was also no significant correlation between cervical length and latency period and maternal and neonatal infection. CONCLUSION: The presence of a short cervix (<15 mm) was found to be related to a latency period of less than 72 hours, but not to maternal or neonatal infections.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):153-157
DOI 10.1590/S0100-72032012000400003
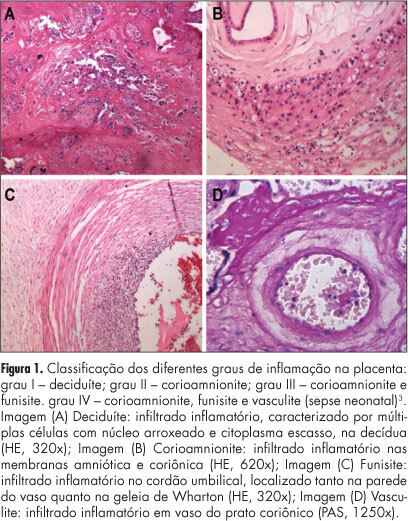
PURPOSE: To evaluate the influence of maternal complications, prematurity, fetal anthropometric parameters and conditions of the newborn on different degrees of chorioamnionitis. METHODS: We analyzed 90 placentas from deliveries performed at the General Hospital of Triângulo Mineiro Federal University with a diagnosis of inflammation in the anatomopathological exams. We reviewed the medical records to obtain relevant maternal and fetal information. The infections were classified as grade I - deciduitis; grade II - chorioamnionitis; grade III - chorioamnionitis and vasculitis; grade IV - neonatal sepsis and grade V - fetal death and pneumonitis. RESULTS: Among the pregnant women analyzed, 50.0% had no complications, 15.0% had ruptured membranes, 15.0% urinary tract infection, 7.5% hypertensive disorders, 7.5% transvaginal infection, 5.0% hematogenous infection, and 11.1% other complications. More than a half the neonates were males and 72.2% were born at term. Analysis of the degree of chorioamnionitis showed that 56.7% had grade I, 22.2% grade II, 4.4% grade III, 10.0% grade IV, and 6.7% grade V. Data were analyzed statistically by the Χ2 test for qualitative variables and by the Spearman test for correlation analysis. The higher grades of chorioamnionitis were observed in cases of maternal complications. We observed negative correlations between all parameters and the degree of fetal chorioamnionitis, which were significant regarding weight, length, thoracic circumference and Apgar score in the first and fifth minutes. CONCLUSIONS: The different patterns of chorioamnionitis were related to different maternal and fetal clinical features, affecting the life conditions of the newborn and the severity of morphological lesions found in stillbirths.