Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(12):631-638
DOI 10.1590/S0100-72032008001200008
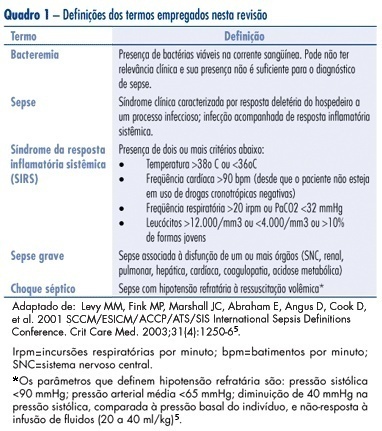
Sepsis is one of the main causes of maternal death, being related to infections from obstetric origin (infected abortion, chorioamnionitis, puerperal infection) or non-obstetric (resulting from infections which occur in other areas). This review aims at describing the mechanisms involved in the physiopathology of this entity and at updating the clinical approach to sepsis, recommended in international guidelines (early goal-directed therapy - precocious resuscitation, or precocious treatment guided by goals), as well as at calling attention to the influence of pregnancy both in the clinical manifestation and in the therapeutic management of septic conditions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(11):573-582
DOI 10.1590/S0100-72032008001100008
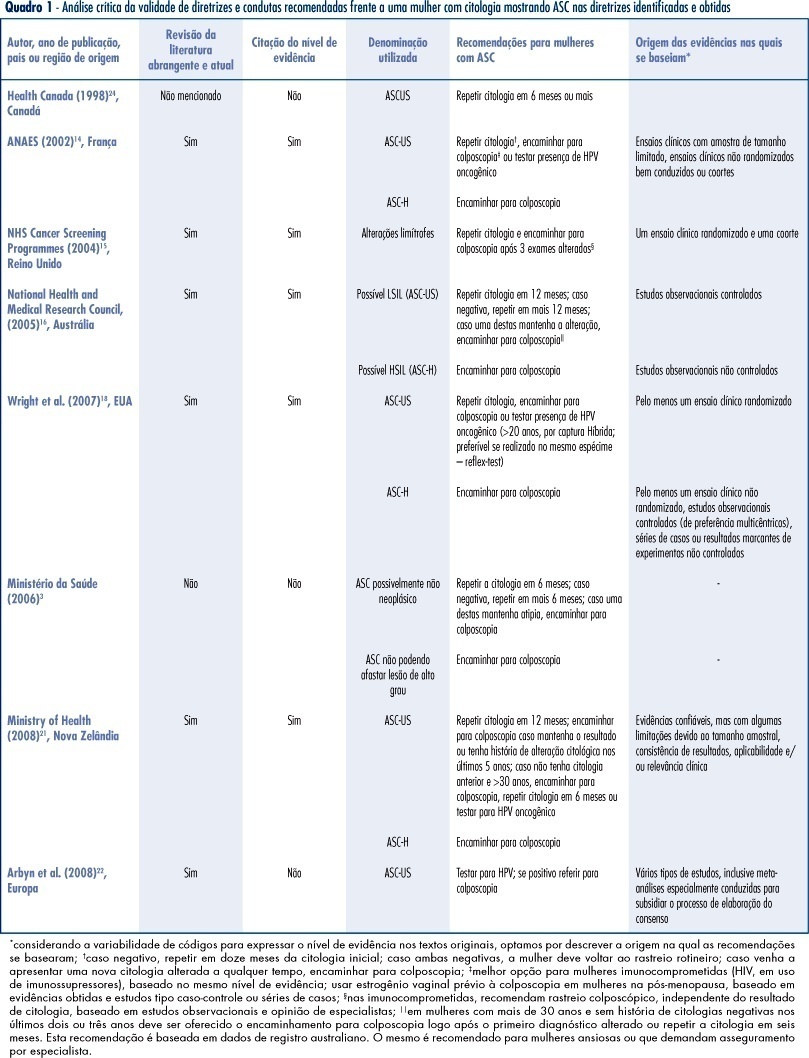
PURPOSE: to identify valid guidelines for the approach of women with cytopathological diagnosis of undetermined significance atypias in squamous cells (ASC), discussing its applicability to the Brazilian scenario. METHODS: an electronic search of publications at PubMed, National Guidelines Clearinghouse and Scholar Google was carried out, as well as a manual search of references from the texts found. The guidelines identified, and specifically related to the theme, were evaluated according to its validity and the recommendations were criticized and summarized. RESULTS: guidelines for the United Kingdom, France, Australia, the USA and New Zealand have been considered as valid. These documents recommend repeating the cytology in six or twelve months, in ASCs of undetermined significance (ASC-US) before referring to colposcopy, and immediate referral to colposcopy in ASCs, when it is not possible to disregard high degree lesions (ASC-H). We have also found valid colposcopy recommendations for women with ASC-US in special situations (immune deficient women requiring specialist assistance) and the use of oncogenic HPV test, which, when present in women over 20, should motivate referral to colposcopy. CONCLUSIONS: the clinical guidelines recommended for the Programa Nacional de Controle do Cancer do Colo do Útero in Brazil can be improved with the referral to colposcopy in special situations (immune deficient women requiring specialist assistance), the use of test for the detection of oncogenic HPV in women over 20 (when present, refer to colposcopy), the investigation of vaginal lesions, the use of estrogens before the colposcopy in post-menopausal women, and disregard biopsia in case of slighter alterations.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(10):524-530
DOI 10.1590/S0100-72032008001000008
Detection of endometrial cancer in asymptomatic women has not proved to be a cost-effective procedure. Studies on this matter have shown that ultrasonography as a detecting method presents a high ratio of false-positive results and a negligible effect on the mortality rate. This way, the assistance strategy should be based on earlier diagnosis and appropriate treatment in women who present postmenopause bleeding. Being a non-invasive method, largely available and with high sensitivity, the transvaginal ultrasonography should be the initial investigative method. Though there is no consensus about the echographical endometrial thickness, above which the investigation is to proceed, diagnostic hysteroscopy should be the next step. The risk of neoplasia in endometriums with thickness under or equal to 3 mm is low enough to limit hysteroscopy to exceptional cases. Biopsy must be a necessary part of the hysteroscopy, because the diagnosis, made on visual basis, alone may lead to false results. Outpatient hysteroscopy can be done in more than 95% of the cases, even in menopausal women, rarely with severe complications. The adoption of "non-contact" examination techniques and the progressive reduction of the hysteroscope diameter have decreased the discomfort associated to small outpatient procedures.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(9):470-479
DOI 10.1590/S0100-72032008000900008
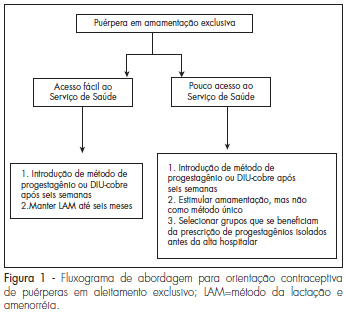
Adequate postpartum contraception is recommended in order to prevent mother and infant morbidity. The mother-infant benefits of lactation are well recognized, and exclusive, regular and frequent breastfeeding is an effective contraceptive method for amenorrheic patients. However, the resumption of fertility varies among women and access to health services is not guaranteed in many regions of the world. We searched the articles in Medline (PubMed) related to the subject published between 1971 to April 2008 and selected the most relevant articles in the literature about postpartum contraception. Short interpregnancy intervals increase maternal and fetal complications and therefore effective postpartum contraception is imperative. The ideal method prescribed should be effective and safe, id est, should not interfere with lactation or alter the hemostatic system. During the postpartum period, ideally non-hormonal methods should be used because they do not alter lactation or hemostasis. However, in populations with difficult access to health or with an early start of calorie supplementation to the newborn, the option should be for progestogens-only contraceptives, ideally initiated after six weeks or earlier in special situations.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(8):420-426
DOI 10.1590/S0100-72032008000800008
Vulvar intraepithelial neoplasia (VIN) is a pathological denomination coined by the International Society for Study of Vulvo-vaginal Diseases (ISSVD) and adopted by the International Society of Gynaecological Pathology (ISGYP) and by the World Health Organization. VIN is a heterogeneous pathological entity with a usual type (warty, basaloid and mixed) and a differentiated type. The incidence of the disease is increasing, especially in young women. The high-risk human papilomavirus (HR-HPV) infection, human immunodeficiency virus (HIV) infection, smoking, cervical, vaginal and rectal intraepithelial neoplasia are considered to be high risk factors for development of VIN. There are no specific symptoms or vulvar macroscopic aspects of VIN. However, a clinical lesion is always present. Liberal vulvar biopsies under colposcopy guidance should be done. Patients with diagnosis of VIN harbor an increased risk for vulvar invasive cancer. Surgical excision and laser CO2 vaporization are the most popular therapeutic modalities for VIN treatment, both with high rates of recurrence. A close follow-up of the patients is advised. Topical imiquimod seems to be a promising treatment option. Probably, prophylactic vaccination against HR-HPV will be an important tool for VIN prevention.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(6):312-321
DOI 10.1590/S0100-72032008000600008
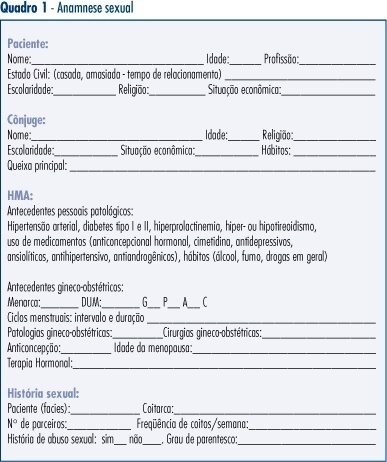
Sexual dysfunction prevalence is high among women. However, doctors rarely ask about their patients' sexual life, because they feel uncomfortable or because their knowledge about investigation techniques is insufficient. The PLISSIT model, a useful tool to access human sexual function, is composed by four elements: permission, limited information, specific suggestions, and intensive therapy, that favor dialogue between the doctor and the patient allowing the access to the sexual complaints. The therapeutics consists of counseling measures, drug prescription, basic orientations about sexual function and interventions on anatomic and functional aspects of the sexual apparatus with positive impact in the woman's sexual life. The present review shows how to use it. In addition, many aspects of female sexual dysfunction are discussed, such as prevalence, diagnostic and treatment options for female sexual dysfunction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(5):261-267
DOI 10.1590/S0100-72032008000500009
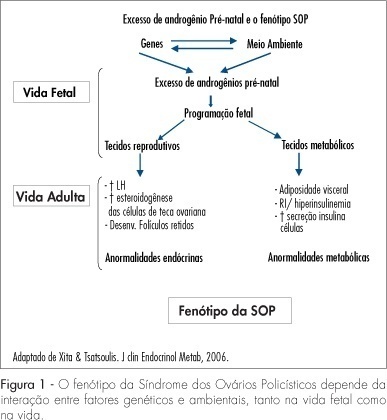
The polycystic ovaries syndrome (POS) is a heterogeneous endocrinal disorder prevalent in 5 to 10% of women in reproductive age. In POS, there is an association with risk factors linked to the development of cardiovascular disease such as insulin resistance, dislipidemia, diabetes mellitus, arterial hypertension, endothelial dysfunction, central obesity, metabolic syndrome and chronic pro-inflammatory markers. Physical exercise practice together with nutritional guidance have been recommended as first rate strategies in the treatment of oligomenorrhea, hirsutism, infertility and obesity in POS women. This way, the objective of the present review was to analyze the specific role played by exercise and/or physical activity in changes of the body shape, in biochemical and hormonal plasmatic levels, and in the POS women’s reproductive function.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(4):201-209
DOI 10.1590/S0100-72032008000400008
Polycystic ovary syndrome (PCOS) occurs in 6 to 10% of women during the reproductive age. Insulin resistance and compensatory hyperinsulinemia are currently two of the main factors involved in the etiopathogenesis of PCOS. The objective of the present review was to discuss the controversies related to the treatment of infertile women with PCOS and during their pregnancy, focusing on the European Society of Human Reproduction and Embryology (ESHRE) and the American Society for Reproductive Medicine (ASRM) current consensus.