-
Original Article10-13-2000
Effects of tamoxifen and conjugated estrogens on the mammary epithelium of rats in persistent estrus
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):33-36
Abstract
Original ArticleEffects of tamoxifen and conjugated estrogens on the mammary epithelium of rats in persistent estrus
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):33-36
DOI 10.1590/S0100-72032000000100006
Views174See morePurpose: to evaluate the morphologic and morphometric alterations produced by tamoxifen and conjugated estrogens in the mammary epithelium of rats in persistent estrus. Methods: thirty-three adult female rats in persistent estrus induced with 1.25 mg testosterone propionate were divided at random into three groups: GI — which received only water, control group (n = 12); GII — treated with 500 mug tamoxifen daily (n = 10); GIII — treated with 30 mug conjugated estrogens per day (n = 11). The first inguinal-abdominal pair of mammary glands of the animals was extirpated and processed for morphologic and morphometric study. Data were analyzed statistically by the Kruskal-Wallis rank analysis of variance (p < 0.05). Results: the morphologic study revealed signs of epithelial atrophy and the morphometric study showed a statistically significant reduction in the mean number of ducts and alveoli in groups II (10.1 and 1.9, respectively) and III (11.1 and 3.5, respectively) compared to group I (25.0 and 6.6, respectively). There was no significant difference between groups II and III. Conclusions: the results of this study indicate that tamoxifen as well as conjugated estrogens at the tested doses produced mammary epithelial atrophy in rats in persistent estrus.
-
Original Article10-13-2000
Is it safe to withold magnesium sulfate in preeclamptic women?
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):13-17
Abstract
Original ArticleIs it safe to withold magnesium sulfate in preeclamptic women?
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):13-17
DOI 10.1590/S0100-72032000000100003
Views94See morePurpose: to determine magnesium sulfate effectiveness to prevent eclamptic seizures in pregnant women diagnosed with preeclampsia. Methods: a case-control study involving 489 pregnant patients admitted to the Hospital de Clínicas de Porto Alegre (HCPA) with the diagnosis of hypertension between January 1990 and January 1997. The patients were divided into two groups: those who received magnesium sulfate (Group I) and those who did not (Group II). All patients were treated according to the hospital’s standard protocol for the treatment of hypertensive pregnant women. The following variables were assessed: maternal age, race, number of seizures, number of seizures in patients receiving magnesium sulfate, period of magnesium sulfate administration, before and after delivery, maternal mortality, need of ICU care, need of mechanical ventilation and length of hospital stay after delivery. Data were assessed with Epi-Info 6.0 statistical package, using multivariate analysis. The main outcome measure was magnesium sulfate use. Results: no differences were found between the two groups in terms of maternal age, race or gestational age. Women who received magnesium sulfate had a higher mean systolic and diastolic blood pressure. Women in the intervention group had a longer hospital stay and a greater need of ICU care. Need of mechanical ventilation and maternal mortality were similar in the two groups. Twenty-two out of 353 women had one or more seizures before admission to the hospital. Six women (27.3%) had one or two additional seizures after magnesium sulfate administration. No subjects had three or more seizures after receiving magnesium sulfate. Conclusion: the results show that eclamptic seizures can be prevented by routine prophylactic magnesium sulfate administration.
-
Original Article10-13-2000
Diagnostic capacity of oligohydramnios by ultrasound using different measures of the maximum pool depth of amniotic fluid in comparison to AFI
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):7-12
Abstract
Original ArticleDiagnostic capacity of oligohydramnios by ultrasound using different measures of the maximum pool depth of amniotic fluid in comparison to AFI
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):7-12
DOI 10.1590/S0100-72032000000100002
Views144See morePurpose: to compare the capacity of diagnosing oligohy-dramnios by ultrasound using different measures of the maximum pool depth of amniotic fluid in comparison to the amniotic fluid index among normal pregnant women from the 36th to the 42nd week of gestation. Methods: a descriptive study of diagnostic validity was perfomed, on 875 normal pregnant women who were studied through routine obstetric ultrasound examinations, including the measure of the maximum pool depth for the diagnosis of oligohydramnios, using the amniotic fluid index as the gold standard. The data were analyzed through sensitivity and specificity of the maximum pool depth of amniotic fluid using 10, 20 and 30 mm cut-offs, in comparison to the amniotic fluid index values of the normal curve in percentiles 2.5 and 10 for different gestational ages. Results: the maximum pool depth had a poor sensitivity to diagnose oligohydramnios when 10 and 20 mm were used as cut-offs, and good sensitivity and specificity when 30 mm was used, in comparison to the amniotic fluid values in percentiles 2.5 and 10. The best sensitivity and specificity of the maximum pool depth were when found using a 30 mm cut-off in comparison to 2.5 percentile to diagnose oligohydramnios. Conclusions: the capacity to diagnose oligohydramnios by the measure of the maximum pool depth is satisfactory only with the cut-off of 30 mm
-
10-13-2000
Femina, RBGO e o ano 2000
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):6-6
-
10-10-2000
Distribuição de Macrófagos, Linfócitos T e Linfócitos B em Vilosidades Placentárias de Gravidezes Humanas a Termo
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):119-119
Abstract
Distribuição de Macrófagos, Linfócitos T e Linfócitos B em Vilosidades Placentárias de Gravidezes Humanas a Termo
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):119-119
DOI 10.1590/S0100-72032000000200015
Views63Distribuição de Macrófagos, Linfócitos T e Linfócitos B em Vilosidades Placentárias de Gravidezes Humanas a Termo […]See more -
10-10-2000
Preditores Clínicos, Histopatológicos e Curva de Regressão do beta-hcg para Tumor Trofoblástico Gestacional em Portadoras de Mola Hidatiforme Completa
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):119-119
Abstract
Preditores Clínicos, Histopatológicos e Curva de Regressão do beta-hcg para Tumor Trofoblástico Gestacional em Portadoras de Mola Hidatiforme Completa
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):119-119
DOI 10.1590/S0100-72032000000200014
Views60Preditores Clínicos, Histopatológicos e Curva de Regressão do b-hcg para Tumor Trofoblástico Gestacional em Portadoras de Mola Hidatiforme Completa […]See more -
10-10-2000
Bacteriúria após Drenagem Vesical no Pós-Operatório de Cirurgias Ginecológicas Vaginais: Comparação entre as Vias Transuretral e Suprapúbica
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):118-118
Abstract
Bacteriúria após Drenagem Vesical no Pós-Operatório de Cirurgias Ginecológicas Vaginais: Comparação entre as Vias Transuretral e Suprapúbica
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):118-118
DOI 10.1590/S0100-72032000000200013
Views66Bacteriúria após Drenagem Vesical no Pós-Operatório de Cirurgias Ginecológicas Vaginais: Comparação entre as Vias Transuretral e Suprapúbica […]See more -
10-10-2000
Avaliação do Risco de Parto Prematuro através da Autopalpação e da Monitorização Computadorizada da Contração Uterina
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):118-118
Abstract
Avaliação do Risco de Parto Prematuro através da Autopalpação e da Monitorização Computadorizada da Contração Uterina
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):118-118
DOI 10.1590/S0100-72032000000200012
Views68Avaliação do Risco de Parto Prematuro através da Autopalpação e da Monitorização Computadorizada da Contração Uterina […]See more
-
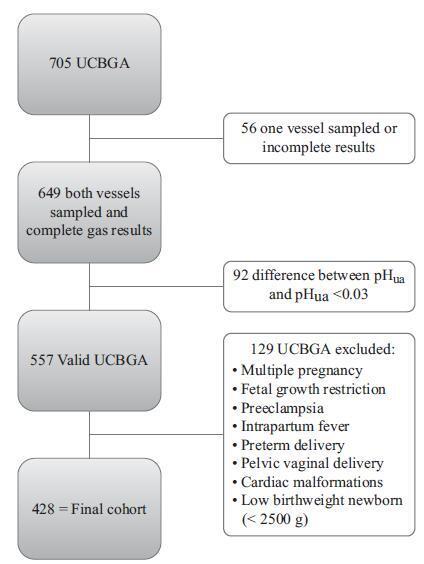
Original Article12-01-2018
Umbilical Cord Blood Gas Analysis, Obstetric Performance and Perinatal Outcome
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):740-748
Abstract
Original ArticleUmbilical Cord Blood Gas Analysis, Obstetric Performance and Perinatal Outcome
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):740-748
Views230See moreAbstract
Objective
To analyze if umbilical artery pH (pHua) ≤7.00 and umbilical artery blood deficit (BDua) ≥12.00 mmol/L are good predictors of adverse neonatal outcomes.
Methods
This was an observational, longitudinal and retrospective cohort study, conducted at the department of obstetrics and gynecology of Centro Hospitalar Tondela Viseu between September 2013 and September 2015. Total cohort and subgroup analysis were performed: group A-women with umbilical cord blood gas analysis (UCBGA) performed for non-reassuring fetal cardiotocographic patterns, placental abruption, or shoulder dystocia; and group B-all the others. Assays were made with the software SPSS for Windows, Versions 20.0 and 21.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 428 UCBGAs met the inclusion criteria. The group analysis revealed an association between group A and pHua ≤7.00, as well as between BDua ≥12.00 mmol/L and 1st minute Apgar score ≤4 (p = 0.011). After the application of the logistic regression models in the total cohort analysis, pHua ≤7.00 had an impact in the occurrence of acute neonatal hypoxia (odds ratio [OR]: 6.71; 95% confidence interval [CI]: 1.21-37.06; p = 0.029); multiparous women had a higher risk of delivering a newborn with first minute Apgar score ≤4 and acute neonatal hypoxia (OR: 5.38; 95% CI: 1.35-21.43; p = 0.017; and OR: 2.66; 95% CI: 1.03-6.89, p = 0.043, respectively); women who had urologic problems during pregnancy had a higher risk of delivering a newborn with 5th minute Apgar score ≤7 (OR: 15.17; 95% CI: 1.29-177.99; p = 0.030); and shoulder dystocia represented a 15 times higher risk of acute neonatal hypoxia (OR: 14.82; 95% CI: 2.20-99.60; p = 0.006).
Conclusion
The pHua and the BDua are predictors of adverse neonatal outcome, and UCBGA is a useful tool for screening newborns at risk. Universal UCBGA should be considered for all deliveries, as it is an accurate screening test for neonatal hypoxia.
-
Case Report06-27-2019
Ectopia Cordis Associated with Pentalogy of Cantrell-A Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):352-356
Abstract
Case ReportEctopia Cordis Associated with Pentalogy of Cantrell-A Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):352-356
Views230Abstract
Pentalogy of Cantrell (PC) is a rare congenital anomaly characterized by changes in the mesodermal median structures and congenital heart disease, often with a poor prognosis. In 1958, Cantrell et al2 defined the full spectrum of the syndrome with the following anomalies: defects of the anterior diaphragm, of the lower part of the sternum, of the supraumbilical region and the abdominal wall, of the diaphragmatic pericardium, and various intracardiac congenital abnormalities. The present report describes a case of ectopia cordis associated with PC and the importance of the participation of a multidisciplinary team in the treatment of this condition.
Key-words abdominal wall defectscongenital heart defectsectopia cordispentalogy of Cantrellumbilical herniaSee more -
Original Article07-10-2023
Quality of Life and Depression Conditions of Women with Gestational Diabetes during Pregnancy and Postpartum Period
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):065-073
Abstract
Original ArticleQuality of Life and Depression Conditions of Women with Gestational Diabetes during Pregnancy and Postpartum Period
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):065-073
Views220See moreAbstract
Objective
The study was conducted to determine the quality of life and depression of women with gestational diabetes during pregnancy and the postpartum period.
Methods
100 pregnant women with gestational diabetes and 100 healthy pregnant women were included in the present study. Data were obtained from pregnant women in their third trimester who agreed to take part in the study. The data was collected during the third trimester and six to eight weeks after the baby was born. The data were obtained by socio-demographic characteristics form, postpartum data collection form, the MOS 36 Item Short Form Health Survey and Center for Epidemiologic Studies Depression Scale (CESD).
Results
The mean age of pregnant women with gestational diabetes in the study was the same as the average age of healthy pregnant women. The CESD score of pregnant women with gestational diabetes was 26,77 ± 4,85 while the corresponding score was 25,19 ± 4,43 for healthy women. Additionally, the score in the postpartum period was 32.47 ± 5.94 for pregnant women with gestational diabetes and 35.47 ± 8.33 for healthy pregnant women. CESD scores were found to be higher than the cut-off score of 16 in both groups, and the mean scores increased during the postpartum period.
Conclusion
During the postpartum period, the quality of life of pregnant women with gestational diabetes was affected more negatively than healthy pregnant women. Depressive symptoms of women with both gestational diabetes and healthy pregnancy were found to be high in pregnancy and postpartum periods.
-
Review Article06-19-2019
Hormonal Biomarkers for Evaluating the Impact of Fetal Growth Restriction on the Development of Chronic Adult Disease
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):256-263
Abstract
Review ArticleHormonal Biomarkers for Evaluating the Impact of Fetal Growth Restriction on the Development of Chronic Adult Disease
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):256-263
Views210Abstract
The hypothesis of fetal origins to adult diseases proposes that metabolic chronic disorders, including cardiovascular diseases, diabetes, and hypertension originate in the developmental plasticity due to intrauterine insults. These processes involve an adaptative response by the fetus to changes in the environmental signals, which can promote the reset of hormones and of the metabolism to establish a “thrifty phenotype”. Metabolic alterations during intrauterine growth restriction can modify the fetal programming. The present nonsystematic review intended to summarize historical and current references that indicated that developmental origins of health and disease (DOHaD) occur as a consequence of altered maternal and fetal metabolic pathways. The purpose is to highlight the potential implications of growth factors and adipokines in “developmental programming”, which could interfere in the development by controlling fetal growth patterns. These changes affect the structure and the functional capacity of various organs, including the brain, the kidneys, and the pancreas. These investigations may improve the approach to optimizing antenatal as well as perinatal care aimed to protect newborns against long-termchronic diseases.
Key-words biomarkersdevelopmentdevelopmental origins of health and diseaseFetal growth restrictiongrowthSee more -
Original Article02-28-2022
Epidemiological Survey on the Perception of Adverse Effects in Women Using Contraceptive Methods in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):25-31
Abstract
Original ArticleEpidemiological Survey on the Perception of Adverse Effects in Women Using Contraceptive Methods in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):25-31
Views237Abstract
Objective
The present study aimed to understand patient perception of the adverse effects of contraceptives to improve health care and adherence to treatment.
Methods
An online questionnaire was available for women in Brazil to respond to assess their perception of adverse effects and their relationship with contraceptive methods.
Results
Of all 536 women who responded, 346 (64.6%) reported current contraceptive use. One hundred and twenty-two (122-34.8%) women reported having already stopped using contraception because of the adverse effects. As for the contraceptive method used, the most frequent was the combined oral contraceptive (212-39.6%). When we calculated the relative risk for headache, there was a relative risk of 2.1282 (1.3425-3.3739; 95% CI), suggesting that the use of pills increases the risk of headache, as well as edema, in which a relative risk of 1.4435 (1.0177-2.0474; 95% CI) was observed. For low libido, the use of oral hormonal contraceptives was also shown to be a risk factor since its relative risk was 1.8805 (1.3527-2.6142; 95% CI). As for acne, the use of hormonal contraceptives proved to be a protective factor, with a relative risk of 0.3015 (0.1789-0.5082; 95% CI).
Conclusion
The choice of a contraceptive method must always be individualized, and the patients must be equal participants in the process knowing the expected benefits and harms of each method and hormone, when present.
Key-words Contraceptiondrug-related side effects and adverse reactionsEpidemiologyGynecologyhormonal contraceptionSee more -
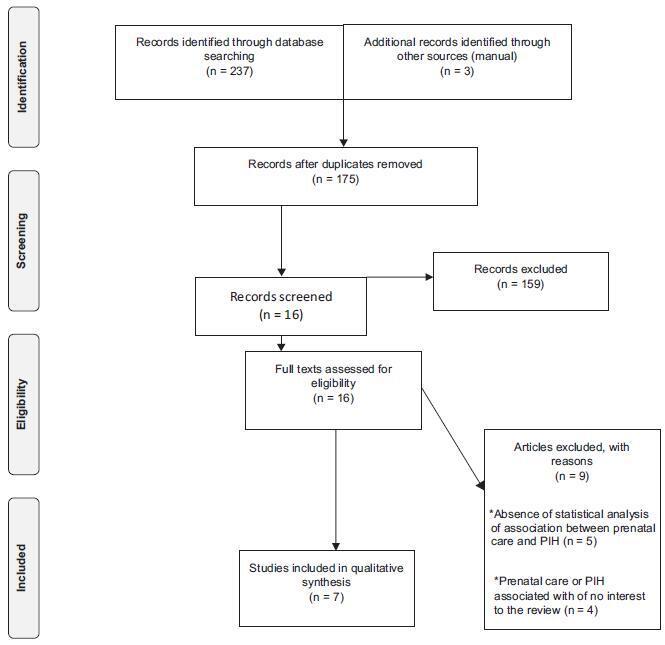
Review Article08-01-2018
Prenatal Care and Hypertensive Gestational Syndromes: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):471-476
Abstract
Review ArticlePrenatal Care and Hypertensive Gestational Syndromes: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):471-476
Views237See moreAbstract
Objective
Evaluate the influence of prenatal care on the occurrence of gestational hypertension.
Methods
The Web of Science, Scopus, Pubmed, Cochrane and ClinicalTrials electronic databases were searched for articles published between January 1st, 2012 and December 31st, 2016. No language restrictions were imposed. The following keywords were used: prenatal care, medical assistance, prenatal education, pregnancy-induced hypertension. The preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist was employed. Two hundred and forty articles were identified during the initial search, but only seven met the inclusion criteria. This systematic review is registered with the international prospective register of systematic reviews (PROSPERO; #CRD42017064103).
Results
The seven studies hada lowriskof bias,withmethodological quality scores ranging fromsix to eight points. Five studies found a positive relationship between prenatal care and pregnancy-induced hypertension, whereas two studies found no significant association between the two variables. The divergence among the studies may have been due to the type of healthcare service at which the study was conducted and the sample size.
Conclusion
Although the studies analyzed differed with regard to methodological aspects, the findings demonstrate the importance of prenatal care during the gestational period as a prevention and health promotion measure.
-
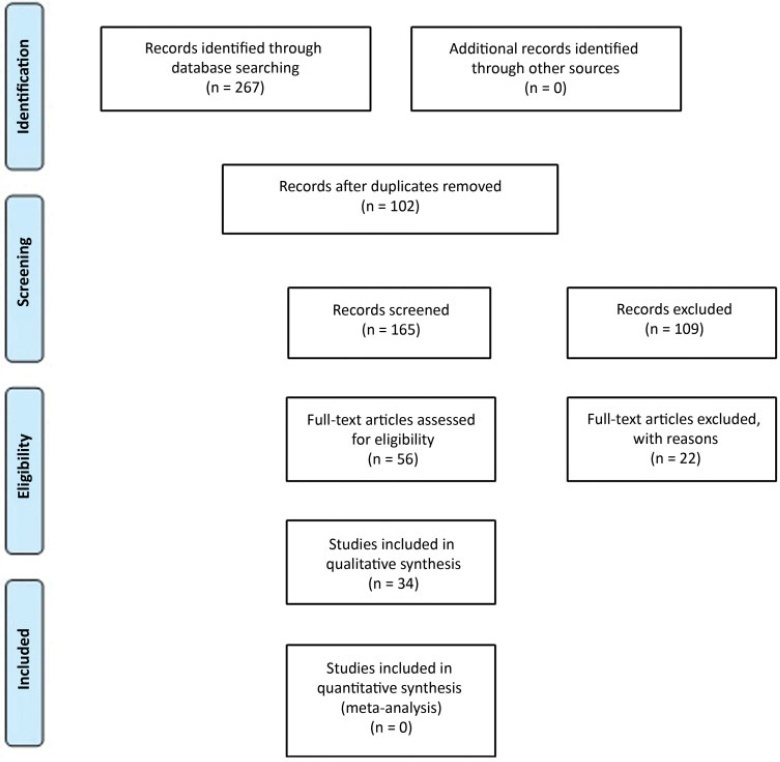
Review Article01-24-2021
Clinical and Obstetric Aspects of Pregnant Women with COVID-19: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):949-960
Abstract
Review ArticleClinical and Obstetric Aspects of Pregnant Women with COVID-19: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):949-960
Views237See moreAbstract
Objective
To analyze the clinical and obstetric aspects of pregnant women with COVID-19.
Methods
A systematic literature review in the MEDLINE/PubMed, LILACS, SCIELO, and CNKI databases was performed from March to May 2020, with the descriptors: Pregnancy; 2019-nCov; Coronavirus; SARS-Cov-2, Covid-19. Of those chosen were original titles, without language and period restriction and that addressed pregnant women with a clinical and/or laboratory diagnosis of COVID-19. Revisions, editorials, and duplicate titles were excluded. The Newcastle-Ottawa (NOS) and Murad et al. scales were used to assess the quality of the studies.
Results
We included 34 articles with 412 pregnant women infected with severe acute respiratory syndrome (SARS-Cov-2), with an average age of 27.5 years of age and 36.0 gestational weeks. The most common symptom was fever (205 [49.7%]), and 89 (21.6%) pregnant women progressed to severe viral pneumonia. Laboratory tests showed an increase in C-reactive protein (154 [37.8%]), and radiological tests showed pneumonia with peripheral ground-glass pattern (172 [51.4%]). Emergency cesarean delivery was indicated for most pregnant women, and the most common gestational complication was premature rupture of ovarian membranes (14 [3.4%;]). We detected 2 (0.5%) neonatal deaths, 2 (0.5%) stillbirths, and 1 (0.2%) maternal death.
Conclusion
Pregnant women with COVID-19 presented a clinical picture similar to that of non-infected pregnant women, with few obstetric or neonatal repercussions. There was a greater indication of cesarean deliveries before the disease aggravated, and there was no evidence of vertical transmission of the infection.
-
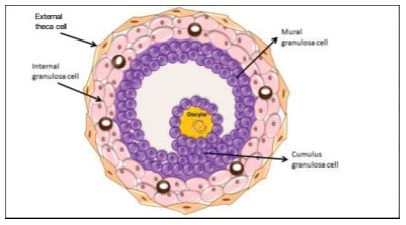
Review Article07-27-2021
Morphology and Biochemistry of Ovulation Morfologia e bioquímica da ovulação
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):480-486
Abstract
Review ArticleMorphology and Biochemistry of Ovulation Morfologia e bioquímica da ovulação
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):480-486
Views337See moreAbstract
The process of ovulation involves multiple and iterrelated genetic, biochemical, and morphological events: cessation of the proliferation of granulosa cells, resumption of oocyte meiosis, expansion of cumulus cell-oocyte complexes, digestion of the follicle wall, and extrusion of the metaphase-II oocyte. The present narrative review examines these interrelated steps in detail. The combined or isolated roles of the folliclestimulating hormone (FSH) and luteinizing hormone (LH) are highlighted. Genes indiced by the FSH genes are relevant in the cumulus expansion, and LH-induced genes are critical for the resumption ofmeiosis and digestion of the follicle wall. A nonhuman model for follicle-wall digestion and oocyte release was provided.
Search
Search in:
Tag Cloud
Pregnancy (252)Breast neoplasms (104)Pregnancy complications (104)Risk factors (103)Menopause (88)Ultrasonography (83)Cesarean section (78)Prenatal care (71)Endometriosis (70)Obesity (61)Infertility (57)Quality of life (55)prenatal diagnosis (51)Women's health (48)Maternal mortality (46)Postpartum period (46)Pregnant women (45)Breast (44)Prevalence (43)Uterine cervical neoplasms (43)


