Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(2):82-88
DOI 10.1590/S0100-72032009000200006
PURPOSE: to evaluate the effect of magnesium sulphate on the pulsatility index (PI) of the uterine, umbilical and fetal middle cerebral arteries, according to the persistency or not of the bilateral protodiastolic notch of the uterine arteries in severe pre-eclampsia. METHODS: a cohort study including 40 pregnant women with severe pre-eclampsia, 23 of them presenting bilateral protodiastolic notch, and 17, unilateral/absent notch. The patients were submitted to Doppler velocimetry before and 20 minutes after the intravenous administration of 6 g of magnesium sulphate. The examination was carried out with the patient in semi-Fowler position, the sonograms being obtained during fetal inactivity, in apnea and absent uterine contraction periods. All the exams were performed by two researchers, the average being considered as the final result. Wilcoxon's test was used to compare the PI, before and after magnesium sulphate in both groups. The difference between the two measurements (before and after magnesium sulphate) was compared between the groups (bilateral incision and unilateral/absent incision) using the Mann-Whitney test. RESULTS: there was a significant increase in the maternal heart rate (MHR) and decrease in the maternal blood pressure, and in the PI medians of the two uterine arteries and in the fetal middle cerebral artery, after magnesium sulphate in both groups. There was a significant decrease in the PI of the left uterine artery and in the umbilical artery, only in the protodiastolic unilateral/absent notch group. Nevertheless, it was not found any significant difference regarding the PI of the right uterine artery, or the cerebral/umbilical relationship, before and after magnesium sulphate in each group. No difference between the groups was found, before and after magnesium sulphate, for any of the studied outcomes. CONCLUSIONS: after the intravenous administration of 6 g of magnesium sulphate to patients with severe pre-eclampsia, a decrease in blood pressure and in the PI of the uterine, umbilical and fetal middle cerebral arteries occurs, besides the increase in the MHR, not influenced by the presence of bilateral protodiastolic notch in the uterine arteries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(2):112-121
DOI 10.1590/S0100-72032006000200007
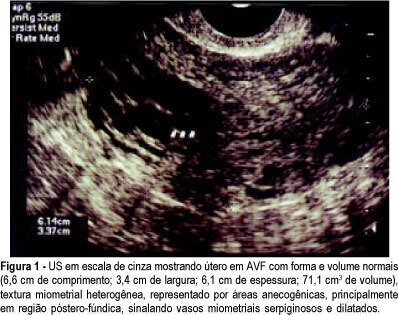
PURPOSE: to investigate the presence and outcome of uterinevascular malformations (UVAM) after gestational trophoblastic disease (GTD). METHODS: retrospective study of 2764 patients with GTD diagnosed from 1987 to 2004. All patients were followed up annually at the "Santa Casa da Misericórdia" Trophoblastic Disease Center (Rio de Janeiro, RJ, Brazil) with transvaginal ultrasonography (US) and color Doppler imaging. Seven patients had a final diagnosis of UVAM based on ultrasonographic analysis - pulsatility index (PI), resistance index (RI), peak systolic velocity (PSV) - and pelvic magnetic nuclear resonance (MNR) findings. Negative beta-hCG values were of utmost importance to establish differential diagnosis with persistent GTD. RESULTS: the incidence of UVAM after GTD was 0.2% (7/2764). US features of UVAM: PI mean 0.44±0,058 (extremes: 0.38-0.52); RI mean 0.36±0.072 (extremes: 0.29-0.50); PSV mean 64.6±23.99 cm/s (extremes: 37-96). MNR image showed a bulky uterus, myometrial inhomogeneity, serpiginous flow-related signal voids, and prominent parametrial vessels. The most common UVAM clinical presentation was vaginal hemorrhage, present in 52.7% (4/7). Pharmacological management with 150 mg medroxyprogesterone acetate was employed to control bleeding, after hemodynamic stabilization. These patients are still being followed and remain asymptomatic nowadays. Two patients with persistent UVAM became pregnant and had successful outcomes. CONCLUSION: patients with antecedent of GTD presenting transvaginal bleeding and negative beta-hCG may be considered to have UVAM and should be investigated through US with Doppler velocimetry. Conservative management is a valuable option in many of the acquired UVAM after GTD.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(5):355-361
DOI 10.1590/S0100-72032004000500003
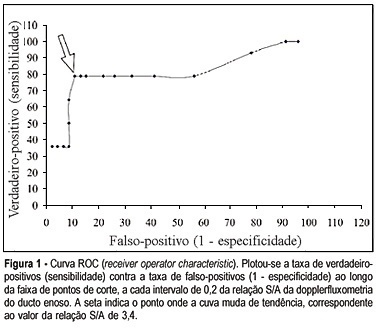
OBJECTIVE: to assess through Dopllerfluxometry the S/A ratio of the ductus venosus and determine the cut-off point to identify preterm fetuses with the 'brain sparing phenomenon". METHOD: a cross-sectional study was performed in 60 pregnant women that presented the "brain sparing phenomenon" (umbilical cerebral ratio >1) and gestational age between 25 and 33 weeks. The following parameters were studied: S/A ratio of the ductus venosus, pH and base excess (BE) of a fetal blood sample collected from the umbilical vein immediately after birth. The fetuses were classified according to the gas analysis result. They were considered abnormal when pH <7.20 and BE < -6 mmol/l. A receiver operator characteristic (ROC) curve analysis was performed to examine the relationship between S/A ratio and fetal acidemia. RESULTS: sixty pregnant women in the period of January 1998 to January 2003 were selected. In the moment of the study the gestational age varied from 25 to 33 weeks, with an average of 29.7 weeks (±1.8 weeks). All of the fetuses presented the "brain sparing phenomenon". Among them 14 presented abnormal gas analysis at birth and 46 presented normal gas analysis. The prevalence of fetuses with abnormal gas analysis in the studied material was 23.33%. Significant association was observed between the abnormal ductus venosus velocimetry and abnormal gas analysis at birth (chi2 = 784.44, p < 0.00001) in preterm fetuses with "brain sparing phenomenon". The best cut-off point of the S/A ratio (where the ROC curves bent) was 3.4. CONCLUSION: fetal acidemia in preterm fetuses with "brain sparing phenomenon" may be noninvasively identified by Doppler measurement of the ductus venosus when the S/A rises above 3.4.