Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):216-221
DOI 10.1590/S0100-7203201400050006
To assess the effects of aerobic physical exercise on the Doppler velocimetry of fetal vessels in pregnant women with no clinical or obstetrical complications.
A cross-sectional study was conducted on 10 healthy low-risk pregnant women at 2 different gestational times: between the 26th and 29th week and 6 days, and at the end of pregnancy, between the 30th and 35th week. The patients were submitted to aerobic physical exercise on a treadmill until reaching fatigue. Ultrasonographic data were obtained at rest and after physical exercise (Doppler velocimetry indices for the umbilical artery, middle cerebral artery, ductus venosus, and uterine arteries). Data were analyzed statistically by the paired and independent Student's t-test using the Statistical Package for the Social Sciences (SPSS) package, version 21.0.
A change in the pulsatility index was observed, with an indication of vasodilatation, with a median value of 1.1±0.1 before exercise and of 1.0±0.1 after exercise; the median value of the resistance index was 0.7±0.04 before exercise and 0.6±0.07 after exercise. The median systole/diastole ratio of the umbilical artery was 3.1±0.4 before exercise and 2.9±0.2 (p=0.03) after exercise at the beginning of pregnancy. No changes in the Doppler velocimetry parameters were observed for the uterine arteries, the middle cerebral artery or the ductus venosus after physical activity at either testing time. Paired analysis of pre- and post-activity data showed a reduction of resistance from the first to the second period (p<0.04).
Physical exercise does not lead to changes in systemic blood flow or fetal-placental flow in healthy pregnant women, confirming that exercises of mild to moderate intensity can be prescribed.
Summary
. ;
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):357-362
DOI 10.1590/S0100-72032013000800004
PURPOSE: To establish reference values for the first trimester uterine artery resistance index (UtA-RI) and pulsatility index (UtA-PI) in healthy singleton pregnant women from Northeast Brazil. METHODS: A prospective observational cohort study including 409 consecutive singleton pregnancies undergoing routine early ultrasound screening at 11 - 14 weeks of gestation was performed. The patients responded to a questionnaire to assess maternal epidemiological characteristics. The left and right UtA-PI and UtA-RI were examined by color and pulsed Doppler by transabdominal technique and the mean UtA-PI, mean UtA-RI and the presence of bilateral protodiastolic notching were recorded. Quartile regression was used to estimate reference values. RESULTS: The mean±standard deviation UtA-RI and UtA-PI were 0.7±0.1 and 1.5±0.5, respectively. When segregated for gestation age, mean UtA-PI was 1.6±0.5 at 11 weeks, 1.5±0.6 at 12 weeks, 1.4±0.4 at 13 weeks and 1.3±0.4 at 14 weeks' gestation and mean UtA-RI was 0.7±0.1 at 11 weeks, 0.7±0.1 at 12 weeks, 0.6±0.1 at 13 weeks and 0.6±0.1 at 14 weeks' gestation. Uterine artery bilateral notch was present in 261 (63.8%) patients. We observed that the 5th and 95th percentiles of the UtA-PI and UtA-RI uterine arteries were 0.7 and 2.3 and, 0.5 and 0.8, respectively. CONCLUSION: Normal reference range of uterine artery Doppler in healthy singleton pregnancies from Northeast Brazil was established. The 95th percentile of UtA-PI and UtA-RI values may serve as a cut-off for future prediction of pregnancy complications studies (i.e., pre-eclampsia) in Northeast Brazil.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(4):171-177
DOI 10.1590/S0100-72032013000400007
PURPOSE: To evaluate changes in the venous axillary-subclavian and lymphatic systems of women with lymphedema after axillary lymphadenectomy for breast cancer treatment. METHODS: This was a case series involving 11 women with unilateral upper limb lymphedema after axillary lymphedenectomy for the treatment of breast cancer. The study was carried out in the Mastology Program of the Clinical Hospital of the Federal University of Goiás, Goiânia, GO, during the period between March 2010 and March 2011. Doppler velocimetry ultrasonography was used to detect the presence of venous changes in the subclavian and axillary veins. Lymphatic changes were evaluated by lymphoscintigraphy in both upper limbs. Fisher's exact test was used for the comparison between limbs. RESULTS: Subclavian vein flow volume in the upper limb with lymphedema was significantly different from that in the contralateral limb (p<0.001), 54.6% of the women had increased flow. In the axillary vein, 45.4% had increased flow and 45.4% had decreased flow, with a statistically significant difference (p<0.01) between limbs. Compared to the contralateral limb, significant lymphatic changes (p<0.05) were also found in the vessel route (not visualized), number of lymphatic vessels (none), axillary lymph nodes (absent) and dermal reflux (present). In the contralateral upper limb without lymphedema, no venous or lymphatic alterations were encountered. CONCLUSION: The women subjected to axillary lymphadenectomy for the treatment of breast cancer presented both venous and lymphatic changes in the upper limb with lymphedema.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(10):510-515
DOI 10.1590/S0100-72032010001000007
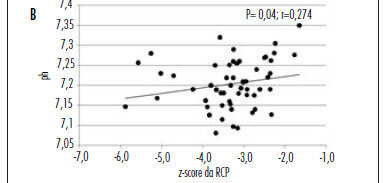
PURPOSE: to evaluate the hypothesis that the fetal cerebroplacental ratio (CPR) is related to acidemia at birth in pregnancies complicated by placental insufficiency detected before 34 weeks of gestation. METHODS: this is a prospective cohort study of 55 patients between 26 and 34 weeks of gestation with a diagnosis of placental insufficiency characterized by abnormal umbilical artery Doppler (pulsatility index>95p). Fetal assessment was performed for each patient by dopplervelocimetry of the umbilical artery, middle cerebral artery and ductus venosus, and by the fetal biophysical profile. CPR was calculated using the ratio between middle cerebral artery pulsatility index and umbilical artery pulsatility index, and the z-score was obtained (number of standard deviations of the mean value at each gestational age). Acidemia at birth was characterized when pH<7.2. RESULTS: of 55 patients, 29 (52.7%) presented acidemia at birth. In the group of fetal acidemia, when compared with the group with pH>7.2, a significant association was observed with CPR values (median 0.47 versus 0.58; p=0.009), pulsatility index of the umbilical artery (median 2.45 versus 1.93; p=0.003), ductus venosus pulsatility index for veins (PIV) (median 1.08 versus 0.85; p=0.034) and suspected or abnormal fetal biophysical profile (37 versus 8%; p=0.031). CPR analysis by z-score showed a negative tendency, but was not statistically significant (p=0.080). Significant correlations were found between pH at birth and CPR (r=0.45; p<0.01), z-score of CPR (r=0.27; p<0.05) and ductus venosus PIV (r=-0.35 p<0.01). CONCLUSION: CPR is associated with the presence of acidemia at birth in pregnancies with placental insufficiency detected before 34 weeks of gestation and this parameter could potentially represent a factor for assessing the severity of fetal involvement.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):549-555
DOI 10.1590/S0100-72032010001100006
PURPOSE: the purpose of this research was to evaluate the morphological aspects and vasculature of the corpus luteum (CL) based on ultrasound parameters during early pregnancy and to assess their relationship with early pregnancy loss. METHODS: this was a prospective cohort study of 90 pregnant patients between 6 and 8 weeks plus 6 days weeks of gestation. We included women at low risk, without acute or chronic systemic disease and with spontaneous conception. Exclusion criteria: use of drugs or smoking, drugs inducing ovulation, history of more than one abortion, no heartbeat visible in the embryo and impossibility of visualization of the corpus luteum. The size, volume, morphological aspects, resistive index, and peak systolic velocity of the corpus luteum were measured by transvaginal sonography. RESULTS: ninety patients were included in the study. Maternal age ranged from 15 to 41 years (mean 28.6±5.8 years). The corpus luteum could be visualized in 87 patients (96.7%), 79 patients had normal pregnancies (90.1%), whereas spontaneous losses occurred in 8 cases (9.9%). In a comparison of the survivors and losses, there was no difference in mean CL diameter (21.8 versus 20.0 mm; p=0.108, Mann-Whitney test), mean CL volume (4.2 versus 3.0 cm³; p=0.076, Mann-Whitney test), mean resistive index (0.55 versus 0,58; p=0.220, Mann-Whitney test), peak systolic velocity (15 versus 15 cm/s; p=0.757, Mann-Whitney test). There was a positive relation between maternal age and resistive index. CONCLUSIONS: no apparent correlation was found between the morphological and vascular aspects of the corpus luteum in early normal pregnancies and first-trimester pregnancy losses.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):352-358
DOI 10.1590/S0100-72032010000700008
PURPOSE: to evaluate the antenatal and postnatal risk factors of neonatal death in pregnancies with absent (DZ) or reverse (DR) end-diastolic flow in the umbilical artery. METHODS: a cross-sectional retrospective study based on data from 48 medical records of singleton pregnancies with DZ or DR, and gestational age of 24 to 34 weeks, at a maternity in the Brazilian Northeast. Mean age was 27.3 (SD: 7.9) years. Twenty (41.7%) patients were primiparas. Hypertensive disorders were found in 44 (91.7%) cases. Thirty-five women (72.9%) had DZ and 13 (27.1%) had DR. Univariate analysis was firstly done (Student's t-test and Fisher's exact test) correlating the parameters with the assessed outcome (neonatal death). Variables that showed significant association were included in the logistic regression model (Wald statistics). The level of significance was set at 5%. RESULTS: The perinatal mortality rate was 64.6% (31/48). There were five stillbirths and 26 neonatal deaths. The mean gestational age at diagnosis was 27.9 (SD: 2.8) weeks. Deliveries before 24 hours after diagnosis occurred in 52.1% of the cases. Cesarean section was performed in 85.4% of the sample. The newborns weighed 975.9 g on average (SD: 457.5). Twenty-four (57.1%) presented Apgar scores below 7 in the first minute and 21.4% in the fifth minute. Gestational age at diagnosis, birth weight and Apgar of the first minute proved to be variables significantly related to neonatal death (p values were: 0.008, 0.004, and 0.020, respectively). The Odds Ratio was 6.6, 25.3 and 13.8 for neonatal death, when the diagnosis was established at the 28th week, weight was <1000 g and first minute Apgar score was <7, respectively. CONCLUSIONS: gestational age at diagnosis, birth weight and Apgar score at the first minute were factors that could predict neonatal death in pregnancies with DV or DR determined by umbilical artery Doppler velocimetry.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(1):11-18
DOI 10.1590/S0100-72032010000100003
PURPOSE: to describe adverse perinatal outcomes in patients with fetal blood flow centralization, using the relationship between the pulsatility indexes of the middle cerebral and umbilical arteries (MCAPI/UAPI), and between the resistance indexes of the middle cerebral and umbilical arteries (MCARI/UARI), as well as to compare both diagnostic indexes. METHODS: 151 pregnant women with diagnosis of blood flow centralization, attended to at the maternity hospital of Universidade Estadual de Campinas, whose delivery occurred up to 15 days after the ultrasonographic diagnosis, were included. It was considered as adverse perinatal outcomes: Apgar index lower than 7 at the fifth minute, permanence in neonatal ICU, small fetus for the gestational age, severe fetal suffering, perinatal death, hypoglycemia, polycythemia, necrotizing enterocolitis, brain hemorrhage, lung hemorrhage, anemia, septicemia, hyaline membrane disease, convulsive syndromes, hyperreflexia syndrome and kidney insufficiency. Rates of the perinatal adverse outcomes (PAO) for the brain-placentary ratios have been compared, using Fisher's exact or Pearson's χ2 tests, at 5% significance level. Adverse perinatal outcomes according to the gestational age have been evaluated using the Cochrane-Armitage test for trend. RESULTS: the adverse perinatal outcomes for the group with the two indexes altered were: 62.5% of the newborns needed to be placed in an ICU, 75.2% were small for the gestational age (SGA), 35.3% were under severe fetal suffering, 84.4% had hypoglycemia, 8.3% polycythemia, 4.2% necrotizing enterocolitis, and 2.1% brain hemorrhage. There has been significant association between the MCAPI/UAPI and MCARI/UARI ratios along the gestational age, and the need for neonatal intensive care, small fetuses for the gestational age, septicemia, necrotizing enterocolitis, kidney insufficiency, hyaline membrane disease, and anemia. There has been no significant difference between the two indexes of adverse perinatal outcome.