-
Review Article08-15-2022
The Correlation between Chlamydia Trachomatis and Female Infertility: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):614-620
Abstract
Review ArticleThe Correlation between Chlamydia Trachomatis and Female Infertility: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):614-620
Views371Abstract
The impact of Chlamydia trachomatis (CT) infection on female’s fertility is not completely established yet, since the level of evidence associating these factors is still weak. Hence, the goal of the present review is to contribute to a better elucidation of this matter. The electronic database chosen was the Medline/PubMed, with the last survey on May 11, 2021. Publication date was used as a filter, with the previous 5 years having been selected. The following describers were used: chlamydia trachomatis AND infertility; chlamydia trachomatis AND tubal alteration AND infertility; chlamydia AND low pregnancy rates. From the 322 studies screened, 293 that failed to meet our eligibility criteria were excluded. Subsequently, we removed seven studies for not having the possible correlation between CT infections and female infertility as its main focus, and three for being about sexually transmitted infections (STIs) in general. Moreover, two studies designed as reviews were also excluded. Ergo, we included 17 studies in our qualitative analysis. The authors conducted research individually and analyzed carefully the studies selected. As we retrieved the information needed for our study through reading the texts, no contact was made with the authors of the studies selected. This systematic review corroborates the hypothesis that CT infection potentiates female infertility, as 76.47% of the included studies found a positive correlation between them. We conclude that there is an important association between CT infection and female infertility. Ergo, making CT screening part of the infertility investigation routine is relevant and has a reasonable justification.
Key-words Chlamydia trachomatishuman reproductionInfertilitySexually transmitted diseasestubal factor infertilitySee more -
Original Article02-28-2022
Assistance to Victims of Sexual Violence in a Referral Service: A 10-Year Experience
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):47-54
Abstract
Original ArticleAssistance to Victims of Sexual Violence in a Referral Service: A 10-Year Experience
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):47-54
Views182See moreAbstract
Objective
To evaluate the assistance provided to women victims of sexual violence and their participation in the follow-up treatment after the traumatic event, presenting a sociodemographic profile, gynecological background, and circumstances of the event, and reporting the results, acceptance, and side effects of prophylaxis for sexually transmitted infections (STIs) and pregnancy.
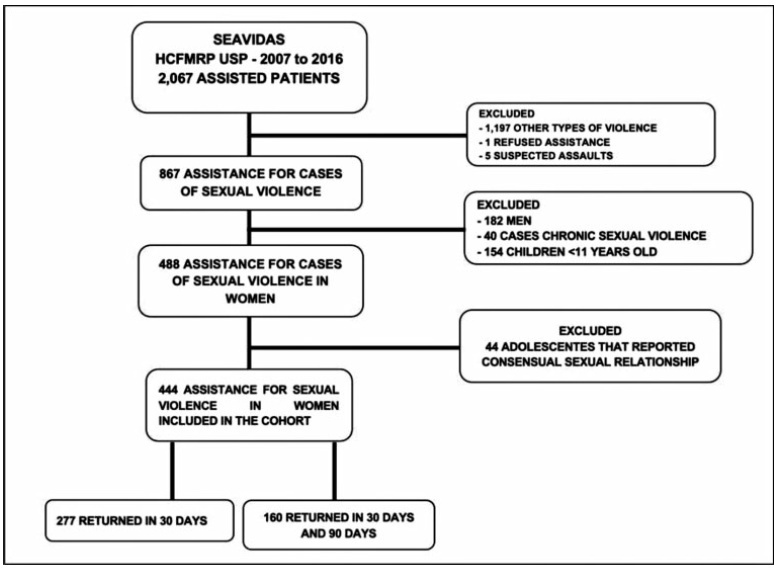
Methods
A retrospective cohort study comprising the period between 2007 and 2016. All women receiving medical care and clinical follow-up after a severe episode of sexual violence were included. Records of domestic violence, male victims, children, and adolescents who reported consensual sexual activity were excluded. The present study included descriptive statistics as frequencies and percentages.
Results
A total of 867medical records were reviewed and 444 cases of sexual violence were included. The age of the victims ranged from10 to 77 years old, most of them selfdeclared white, with between 4 and 8 years of education, and denying having a sexual partner. Sexual violence occurred predominantly at night, on public thoroughfare, being committed by an unknown offender. Most victims were assisted at the referral service center within 72 hours after the violence, enabling the recommended prophylaxis. There was high acceptance of antiretroviral therapy (ART), although half of the users reported side effects. Seroconversion to human immunodeficiency virus (HIV) or to hepatitis B virus (HBV) was not detected in women undergoing prophylaxis.
Conclusion
In the present cohort, the profile of victims of sexual violence was loweducated, young, white women. The traumatic event occurred predominantly at night, on public thoroughfare, being committed by an unknown offender. Assistance within the first 72 hours after sexual violence enables the healthcare center to provide prophylactic interventions against STIs and unwanted pregnancies.
-
Original Article09-01-2018
Sexually Transmitted Infections Detected by Multiplex Real Time PCR in Asymptomatic Women and Association with Cervical Intraepithelial Neoplasia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):540-546
Abstract
Original ArticleSexually Transmitted Infections Detected by Multiplex Real Time PCR in Asymptomatic Women and Association with Cervical Intraepithelial Neoplasia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):540-546
Views222Abstract
Objective
To determine the frequency of sexually transmitted infections (STIs) in asymptomatic women and the association of STIs with cervical intraepithelial neoplasia (CIN).
Methods
A cross-sectional studywas performed, enrollingwomen examined in a general gynecology clinic and in a colposcopy referral center fromOctober 2014 to October 2015. The colposcopy groupconsisted of 71women, and the general gynecologygroupconsisted of 55 women. Cervical samples were collected for cervical cytology and a multiplex realtime polymerase chain reaction (PCR) was developed to detect human papillomavirus (HPV) and the STIs caused by the following microorganisms: Chlamydia trachomatis, Mycoplasma hominis, Mycoplasma genitalium, Ureaplasma urealyticum, and Neisseria gonorrhoeae. A multivariate analysis was performed by logistic regression, considering the significance level of 0.05.
Results
The general frequency of STIs was: 46.8% (HPV); 27.8% (C. trachomatis); 28.6% (M. genitalium); 0.8% (M. hominis); 4.8% (U. urealyticum); and 4.8% (N. gonorrhoeae). The significant risk factors for CIN were: HPV infection (odds ratio [OR] = 2.53; p = 0.024); C. trachomatis (OR = 3.04; p = 0.009); M. genitalium (OR = 2.37; p = 0.04); and HPV and C. trachomatis coinfection (OR = 3.11; p = 0.023). After the multivariate analysis, a significant associationwas found betweenHPVand CIN(OR = 2.48; 95% confidence interval [95%CI]: 1.04-5.92; p = 0.04); and between C. trachomatis and CIN (OR = 2.69; 95%CI: 1.11-6.53; p = 0.028).
Conclusion
The frequency of STIs was high in asymptomatic patients. Infections by HPV and C. trachomatis were independently associated with the presence of CIN. The high frequency of STIs in asymptomatic women suggests the need for routine screening of these infections.
Key-words Cervical intraepithelial neoplasiaChlamydiaPapillomavirus infectionsPolymerase chain reactionSexually transmitted diseasesSee more -
Original Article07-01-2017
Prevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian Amazon
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):350-357
Abstract
Original ArticlePrevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian Amazon
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):350-357
Views262Abstract
Purpose
The aim of this study was to evaluate the overall and type-specific prevalence of human papillomavirus (HPV) infection among females living in riverside communities in the state of Pará, in the Eastern Brazilian Amazon. These communities are inhabited by low-income people, and are accessible only by small boats. Cervical cytology and risk factors for HPV infection were also assessed.
Methods
Cervical samples from 353 women of selected communities were collected both for Papanicolau (Pap) test and HPV detection. Conventional polymerase chain reaction (PCR) and real-time PCR were used to assess the overall and type-specific prevalence of HPV-16 and HPV-18, the main oncogenic types worldwide. Epidemiological questionnaires were used for the assessment of the risk factors for HPV infection.
Results
The mean age of the participants was 37 years (standard deviation [SD] ± 13.7). Most were married or with a fixed sexual partner (79%), and had a low educational level (80%) and family monthly income (< U$ 250; 53%). Overall, HPV prevalence was 16.4% (n = 58), with 8 cases of HPV-16 (2.3%) and 5 of HPV-18 (1.4%). Almost 70% of the women surveyed had never undergone the Pap test. Abnormal cytology results were found in 27.5% (n = 97) of the samples, with higher rates of HPV infection according to the severity of the lesions (p = 0.026).
Conclusions
The infections by HPV-16 and HPV-18 were not predominant in our study, despite the high prevalence of overall HPV infection. Nevertheless, the oncogenic potential of these types and the low coverage of the Pap test among women from riverside communities demonstrate a potential risk for the development of cervical lesions and their progression to cervical cancer, since the access to these communities is difficult and, in most cases, these women do not have access to primary care and public health services.
Key-words cervical cancer screeningEpidemiologyhuman papillomavirus 16human papillomavirus 18Sexually transmitted diseasesSee more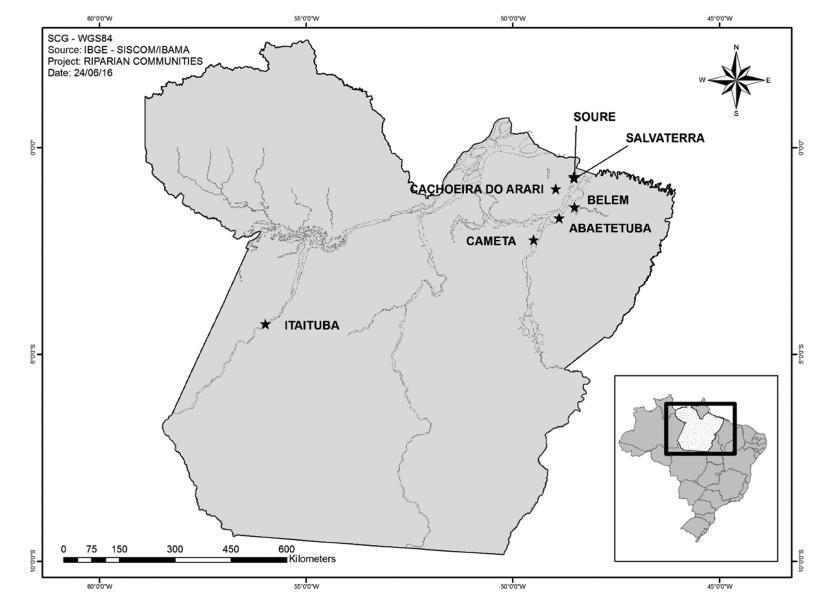
-
Original Article09-01-2015
Prevalence of congenital and perinatal infection in HIV positive pregnant in Belo Horizonte metropolitan region
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(9):421-427
Abstract
Original ArticlePrevalence of congenital and perinatal infection in HIV positive pregnant in Belo Horizonte metropolitan region
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(9):421-427
DOI 10.1590/SO100-720320150005355
Views128PURPOSE:
To evaluate the prevalence of toxoplasmosis, rubella, cytomegalovirus, hepatitis B&C and syphilis (Torchs) in a cohort pregnant women and to identify the sociodemographic, clinical and laboratory factors.
METHODS:
A total of 1,573 HIV-infected pregnant women from a Brazilian metropolitan region were studied between 1998 and 2013. The results of serological tests were available for 704 (44.8%) pregnant women. Pregnant women were considered to be Torchs positive (Gtp) when they had positive results for at least one of these infections, and to be Torchs negative (Gtn) when they had negative results for all of them. Maternal covariables were: age, marital status, educational level, time and mode of infection, CD4 lymphocyte count, viral load at delivery, and use of antiretroviral therapy (ARV). Neonatal covariables were: HIV infection, prematurity, low birth weight, neonatal complications, abortion and neonatal death. Odds ratios with 95% confidence interval were used to quantify the association between maternal and neonatal variables and the presence of Torchs.
RESULTS:
Among 704 pregnant women, 70 (9.9%; 95%CI 7.8-12.4) had positive serological tests for any Torchs factor. The individual prevalence rates were: 1.5% (10/685) for toxoplasmosis; 1.3% (8/618) for rubella; 1.3% (8/597) for cytomegalovirus; 0.9% (6/653) for hepatitis B and 3.7% (20/545) for hepatitis C; and 3.8% (25/664) for syphilis. The HIV Vertical HIV transmission was 4.6% among Gtp pregnant women and 1.2% among Gtn women. Antiretroviral therapy (ARV), vertical transmission, low birth weight and neonatal complications were significantly associated with Torchs positivity in univariate analysis.
CONCLUSIONS:
The Torchs prevalence found in the study was high for some infections. These findings emphasize the need to promote serological Torchs screening for all pregnant women, especially HIV-infected women, so that an early diagnosis can be made and treatment interventions can be implemented to prevent vertical HIV transmission.
Key-words Child transmission of infectious diseaseHIV infectionsPregnancyPregnancy complications, infectiousSexually transmitted diseasesSee more -
Original Article05-01-2015
Frequency of Human Papillomavirus in the placenta, in the colostrum and in the umbilical cord blood
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(5):203-207
Abstract
Original ArticleFrequency of Human Papillomavirus in the placenta, in the colostrum and in the umbilical cord blood
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(5):203-207
DOI 10.1590/SO100-720320150005293
Views64PURPOSE:
To determine the frequency of Human Papillomavirus (HPV) in the placenta, in the
colostrum and in the umbilical cord blood of parturient women and their newborns
assisted at the Clinic of Gynecology and Obstetrics of the University Hospital of
Rio Grande (RS), Brazil.METHODS:
Biopsies were collected from 150 placentas on the maternal side, 150 on the fetal
side, 138 samples of umbilical cord blood and 118 of the colostrum. The placenta
biopsies were collected from the central and peripheral portions. DNA was
extracted according to the manufacturer's protocol and to a reference found in the
literature. HPV was detected by the nested polymerase chain reaction (PCR-Nested)
using primers MY09/11 and GP5/GP6. Genotyping was performed by direct sequencing.
The participants responded to a self-applied questionnaire with demographic and
clinical data, in order to characterize the sample.RESULTS:
HPV was detected in 4% (6/150) of cases on the mother's side of the placentas, in
3.3% (5/150) on the fetal side, in 2.2% (3/138) in umbilical cord blood and in
0.84% (1/118) in colostrum samples. The vertical transmission rate was 50%. HPV-6
was the low-risk genotype found (60%) and the high-risk genotypes were HPV-16 and
HPV-18 (20% each).CONCLUSIONS:
These results suggest that HPV can infect the placenta, the colostrum and the
umbilical cord blood.Key-words GenotypeInfectious disease transmission, verticalMolecular biologySexually transmitted diseasesSee more -
Original Article08-01-2014
Chlamydia trachomatis and Neisseria gonorrhoeae infection: factors associated with infertility in women treated at a human reproduction public service
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(8):353-358
Abstract
Original ArticleChlamydia trachomatis and Neisseria gonorrhoeae infection: factors associated with infertility in women treated at a human reproduction public service
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(8):353-358
DOI 10.1590/SO100-720320140005009
Views88PURPOSE:
To evaluate the prevalence of Chlamydia trachomatis and Neisseria gonorrhoeae in women undergoing assisted reproduction in a public reference service in the midwestern region of Brazil.
METHODS:
A cross-sectional study was conducted on 340 women aged from 20 to 47 years with a history of infertility, undergoing assisted reproduction techniques. Infections with Chlamydia trachomatis and Neisseria gonorrhoeae identified in urine specimens by PCR, and the profile of infertility were analyzed. We used the χtest or Fisher's exact test to evaluate the association between infection and variables.
RESULTS:
The prevalence of Chlamydia trachomatis infection was 10.9%, and Neisseria gonorrhoeae co-infection was observed in 2 cases. Women infected with Chlamydia trachomatis had more than 10 years of infertility (54.1%; p<0.0001). The tubal factor was the main cause in infected cases (56.8%; p=0.047). Tubal occlusion was found in 67.6% of cases with positive infection (p=0.004).
CONCLUSION:
There was an association of tubal obstruction with infection by Chlamydia trachomatis and Neisseria gonorrhoeae, reinforcing the need for effective strategies for an early detection of sexually transmitted diseases, especially in asymptomatic women of childbearing age.
Key-words assistedChlamydia infectionsGonorrheaInfertilityPrevalenceReproductive techniquesSexually transmitted diseasesSee more -
Original Article10-10-2013
Prevalence of Chlamydia trachomatis and risk factors associated with infection detected in endocervical sample
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):379-383
Abstract
Original ArticlePrevalence of Chlamydia trachomatis and risk factors associated with infection detected in endocervical sample
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):379-383
DOI 10.1590/S0100-72032013000800008
Views74PURPOSE: It was to determine the prevalence of Chlamydia trachomatis and the risk factors associated with infection in endocervical specimens from women seen in outpatient Obstetrics and Gynecology. METHODS: Samples of endocervical secretion of 200 women treated at the University Hospital of the Federal University of Rio Grande were analyzed for the presence of C. trachomatis by polymerase chain reaction (PCR) using primers that amplify CT05/CT06 281 base pairs of the main outer membrane protein of C. trachomatis. All participants completed a pre-coded and self-report questionnaire. Data were analyzed with the SPSS 17.0 software; for multivariate analysis it was used Poisson regression. RESULTS: Of the 200 women who were included in the study, the prevalence of infection with C. trachomatis was 11% (22 patients) and these 55 (27.5%) were positive for HPV. Risk factors associated with infection by C. trachomatis were: 8 years or less of schooling (p<0.001), family income below the poverty level (p=0.005), first intercourse at age 15 or less (p=0.04) and being a carrier of the virus HIV (p<0.001). After multivariate analysis, only the variables of schooling or less than eight years (PR 6.0; 95%CI 1.26 - 29.0; p=0.02) and presence of HIV (RP 14.1; 95%CI 3.4 - 57.5; p<0.001) remained statistically significant. CONCLUSIONS: The prevalence of C. trachomatis in endocervical specimens by PCR was 11%. The factors associated with a higher infection by C. trachomatis were lower education and being HIV positive.
Key-words Chlamydia infectionsPolymerase chain reactionPrevalenceQuestionnairesRisk factorsSexually transmitted diseasesSee more


