Summary
Revista Brasileira de Ginecologia e Obstetrícia. 07-01-2018;40(7):410-416
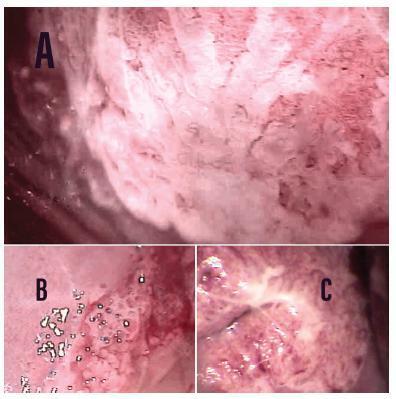
To estimate the cytological and colposcopic performances for the diagnosis of cervical neoplasias.
Cross-sectional retrospective study with data from patients’ charts. The participants underwent colposcopy, guided biopsies, and excision when needed. The cytological and colposcopic categorization followed the Bethesda System and the international colposcopic terminologies. The cytology and colposcopy performances were evaluated by sensitivity (SE), specificity (SP), positive predictive value (PPV), and negative predictive value (NPV) analyses with 95% confidence interval (95% CI).
From 1,571 participants, a total of 1,154 (73.4%) were diagnosed with cervical squamous intraepithelial neoplasia grade 2 or worse (CIN 2+), 114 (7.2%) with adenocarcinoma in situ or worse (AIS+), 615 (39.2%) presented atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion or worse (ASC-H+) cytology, and 934 (59.4%) presented major or suspicious for invasion colposcopic abnormalities. The SE, SP, PPV, and NPV of ASC-H+ for diagnoses of CIN 2+ and AIS+ were, respectively: 44% (95% CI: 41-47) and 72% (95% CI: 67-76), 79% (95% CI: 77-81) and 79% (95% CI: 75-83), 88% (95% CI: 87-90) and 55% (95% CI: 50-60), and 28% (95% CI: 26-31) and 88% (95% CI: 85-91). The SE, SP, PPV, and NPV of major or suspicious for invasion colposcopic abnormalities for diagnoses of CIN 2+ and AIS+were, respectively: 62% (95% CI: 60-65) and 86% (95% CI: 83-89), 59% (95% CI: 57-62) and 59% (95% CI: 55-64), 85% (95% CI: 83-87) and 44% (95% CI: 40-49), and 29% (95% CI: 27-32) and 92% (95% CI: 89-94).
The SE analyses results of ASC-H+ and major or suspicious for invasion colposcopic abnormalities were higher for diagnoses of glandular neoplasias. These results confirm the role of cytology in identifying women at risk who will have their final diagnoses settled by colposcopy and histology.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 05-11-2012;34(5):209-214
DOI 10.1590/S0100-72032012000500004
PURPOSE: To assess the prevalence of bacterial vaginosis and to compare the accuracy of testing pH and KOH with the Nugent gradient, the gold standard for the diagnosis of bacterial vaginosis (BV) in asymptomatic and symptomatic pregnant women at low risk. METHODS: We conducted a cross-sectional study on 321 pregnant women with gestational age between 14 and 26 weeks, 218 of them asymptomatic and 103 with vaginal complaints suggestive of bacterial vaginosis. All women were assessed by the criteria of Nugent and subjected to the measurement of vaginal pH and to the 10% KOH test. The Kappa coefficient was used to evaluate the methods in terms of diagnostic agreement. RESULTS: Most patients were adolescents (mean age 21.0±5.6 years), nulliparous and mulattos. The prevalence of bacterial vaginosis was 33.3% as estimated by the pH and KOH method and 35.5% by the Nugent method. Excellent agreement of the methods was found among asymptomatic pregnant women, with 72.5% of them showing negative results to both tests, which resulted in a high Kappa coefficient (k=0.82). The group of symptomatic women showed 49.5% positivity to both diagnostic methods, with excellent agreement (k=0.74). CONCLUSION: The prevalence of bacterial vaginosis determined by both the pH and KOH method and the Nugent score was high. The pH and KOH method can diagnose bacterial vaginosis as accurately as the Nugent criterion.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 06-29-2009;31(4):203-209
DOI 10.1590/S0100-72032009000400008
Among the clinical factors for preterm birth, some confer substantial increased risk, including a history of preterm birth, multiple gestation and vaginal bleeding in the second trimester. However, these factors are present only in a minority of women who ultimately deliver preterm and thus have low sensitivity. Cervical dilatation, effacement and position as determined by manual examination have been related to an increased risk of preterm birth but also suffer from low sensitivity and positive predictive values. Cervical length measured with transvaginal ultrasound has also been related to an increased risk of preterm birth as cervical length decreases. The reported sensitivity is better than other tests, but positive predictive value is low. The principal utility of the fetal fibronectin assay lies in its negative predictive value in symptomatic women. Increased sensitivity has been reported when cervical length is used in combination with fetal fibronectin.