Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo69
To compare the effectiveness and safety of non-mRNA versus mRNA COVID-19 vaccines on pregnant women and their newborns in a systematic review with meta-analysis.
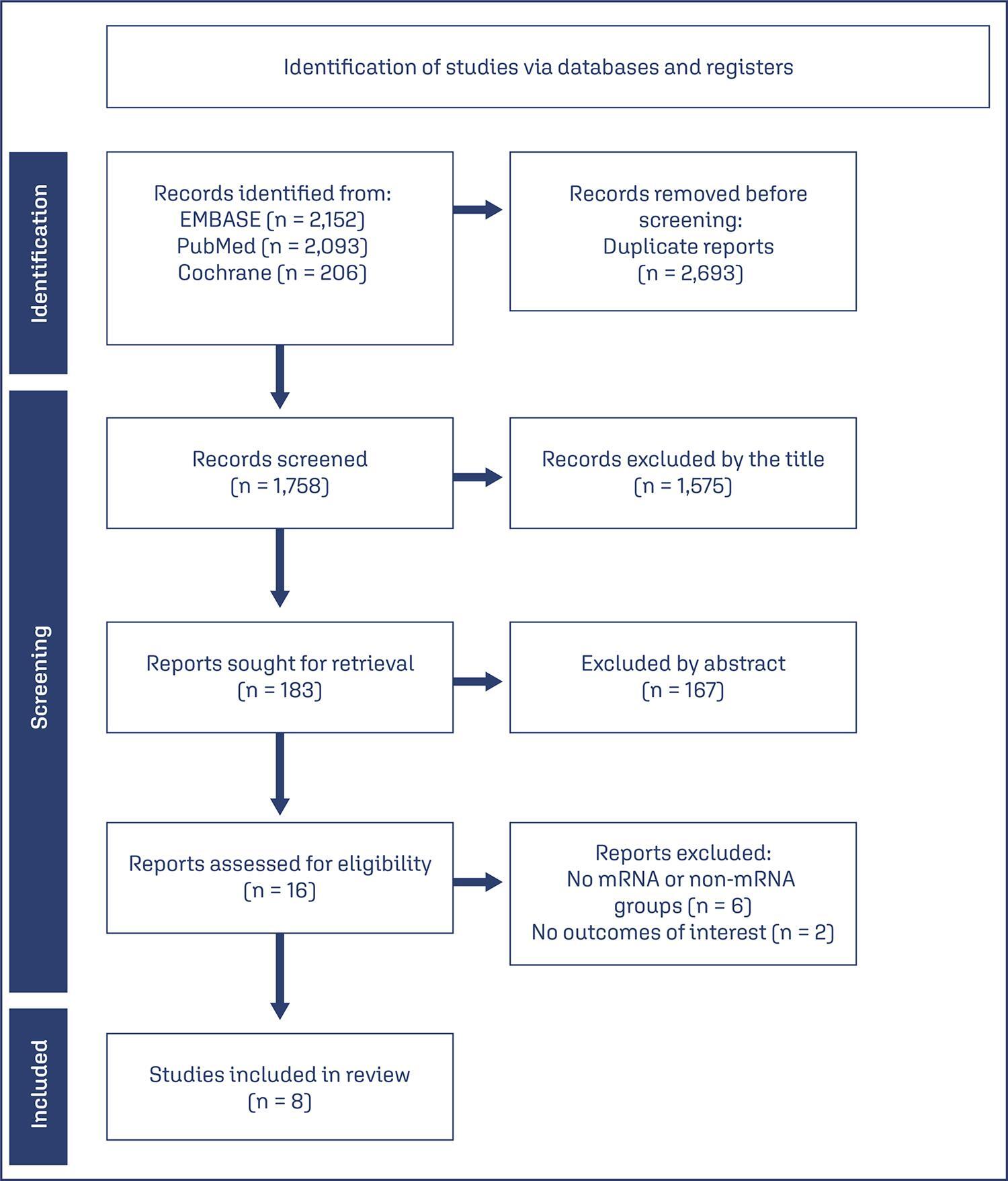
We searched PubMed, Embase, and Cochrane Central in May 2023.
The search strategy yielded 4451 results, 16 studies were fully reviewed. We selected case-control studies analysing non-mRNA versus mRNA vaccines. Data collection and analysis: we assessed the risk of bias using the Cochrane Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool. Standardised mean differences were pooled using random-effect models.
We identified 8 prospective and retrospective studies with a total of 32,153 patients. Non-mRNA vaccines were associated with a higher incidence of fever (OR 2.67; 95% CI 2.08-3.43; p<0.001), and a lower incidence of fetal or neonatal death (OR 0.16; 95% CI 0.08-0.33; p<0.001). In subgroup analyses, the Jansen vaccine (Ad26.COV2.S) was found to have a higher rate of premature labor/delivery (OR 4.48; 95% CI 1.45-13.83; p=0.009) and missed/spontaneous abortion (OR 1.90; 95% CI 1.09-3.30; p=0.02), as compared with the Pfizer (BNT162b2) vaccine.
non-mRNA vaccines are associated with a lower incidence of fetal or neonatal death among pregnant women who receive a Covid19 vaccine, although at an increased rate of pyrexia compared with mRNA vaccines. Other studies are required for better assessment.
CRD42023421814
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo52
To analyze the death of Brazilian pregnant and postpartum women due to COVID-19 or unspecific cause.
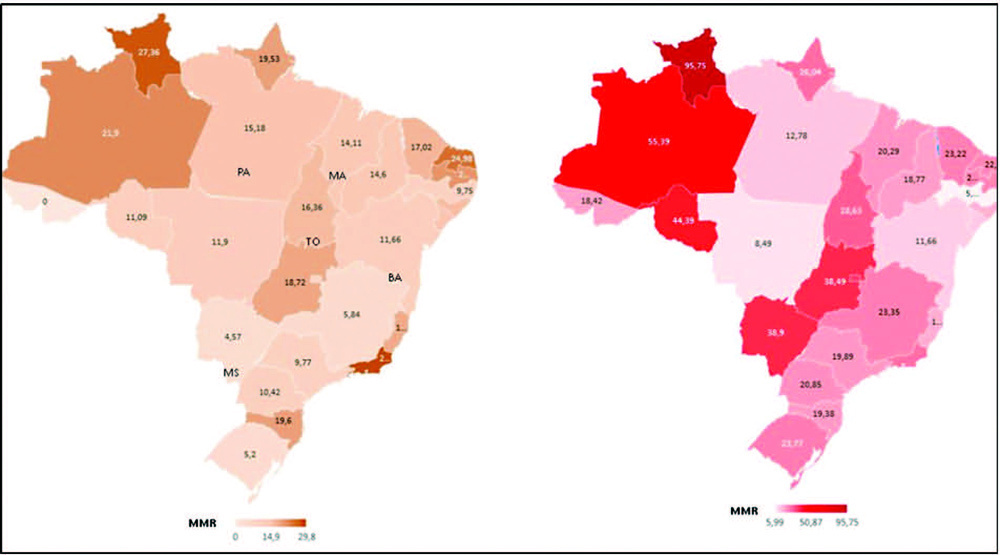
This is retrospective, descriptive-exploratory, population-based study carried out with the Sistema de Informação de Vigilância Epidemiológica da Gripe (SIVEP-Gripe) database, with pregnant and postpartum women of reproductive age who died from confirmed COVID-19 between 2020 and 2021. The chosen variables were: age, gestational period, type and number of comorbidities, skin color, using the statistical software R Foundation for Statistical Computing Platform, version 4.0.3 and Statistical Package for Social Science, version 29.0 for analysis.
A total of 19,333 cases of pregnant and postpartum women aged between 10 and 55 years diagnosed with SARS were identified, whether due to confirmed COVID-19 or unspecific causes. Of these, 1,279 died, these cases were classified into two groups according to the cause of death: deaths from COVID-19 (n= 1,026) and deaths from SARS of unspecific cause (n= 253).
The risk of death increased among black and brown women, in the postpartum period and with the presence of comorbidities, mainly diabetes, cardiovascular diseases and obesity. The data presented here draw attention to the number of deaths from SARS, especially among sociodemographic profiles, precarious access to health, such as the black population. In addition, limitations in adequate access to health care are reinforced by even lower rates of ICU admissions among women who died from SARS of an unspecified cause.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):439-446
To evaluate the fetal and maternal effects of the severe acute respiratory syndrome virus 2 (SARS-CoV-2) infection in women with hypertensive disorders of pregnancy.
Patients with hypertensive disorders of pregnancy and SARS-CoV-2 polymerase chain reaction (PCR) positivity (n = 55) were compared with cases with similar characteristics and PCR negativity (n = 53). The study group was further divided into two groups as severe (n = 11) and nonsevere (n = 44) coronavirus disease 2019 (COVID-19). The groups were compared in terms of clinical characteristics and perinatal outcomes.
The study and control groups were similar in terms of maternal age, parity, gestational age at diagnosis, type of hypertensive disorders, magnesium sulfate administration rate, gestational age at birth, birth weight, Apgar scores, and maternal complications. However, all cases of fetal loss (n = 6) were observed in the SARS-CoV-2 positive group (p = 0.027). From the 6 cases, there were 5 in the nonsevere group and 1 patient in the severe SARS-CoV-2 positive group. Moreover, higher rates of maternal complications, lower oxygen saturation values, and intensive care unit admissions were observed in the severe COVID-19 group.
Physicians should be cautious about the management of hypertensive disorders of pregnancy cases with SARS-CoV-2 positivity. Fetal loss seems to be more common in cases with SARS-CoV-2 positivity and severe COVID-19 seems to be associated with higher rates of maternal complications. Close follow-up for fetal wellbeing and active management of severe cases in terms of maternal complications seem to be favorable.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):261-265
To determine the existence of SARS-CoV-2 in the peritoneal fluid to assess the risk of exposure through surgical smoke and aerosolization threatening healthcare workers during abdominal surgery.
SARS-CoV-2 is a respiratory virus and possible ways of viral transmission are respiratory droplets, close contact, and fecal-oral route. Surgeries pose risk for healthcare workers due to the close contact with patients. Aerosolized particles may be inhaled via the leaked CO2 during laparoscopic procedures and surgical smoke produced by electrocautery.
All the data of 8 patients, who were tested positive for COVID–19, were collected between August 31, 2020 and April 30, 2021. Recorded clinicopathologic data included age, symptoms, radiological and laboratory findings, antiviral treatment before surgery, type of surgery and existence of the virus in the peritoneal fluid. Nasopharyngeal swab RT-PCR was used for the diagnosis. COVID–19 existence in the peritoneal fluid was determined by RT-PCR test as well.
All 8 COVID–19 positive patients were pregnant, and surgeries were cesarean sections. 1 of the 8 patients was febrile during surgery. Also only 1 patient had pulmonary radiological findings specifically indicating COVID-19 infection. Laboratory findings were as follows: 4 of 8 had lymphopenia and all had elevated D-dimer levels. Peritoneal and amniotic fluid samples of all patients were negative for SARS-CoV-2.
SARS-CoV-2 exposure due to aerosolization or surgical fumes does not seem to be likely, provided the necessary precautions are taken.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(6):347-355
To review the literature and synthesize evidence on pathophysiological interactions attributed to the simultaneous occurrence of COVID-19 and preeclampsia.
A systematic review was conducted from November (2021) to January (2022) to retrieve observational studies published on the PubMed, LILACS, SciELO Brazil and Google Scholar databases. The search was based on the descriptors [(eclampsia OR preeclampsia) AND (COVID-19)]. Quantitative studies that pointed to pathophysiological interactions were included. Literature reviews, studies with HIV participants, or with clinical approach only were excluded. The selection of studies was standardized and the evaluation was performed by pairs of researchers.
In this review, 155 publications were retrieved; 16 met the inclusion criteria. In summary, the physiological expression of angiotensin-converting enzyme-2 (ACE-2) receptors is physiologically increased in pregnant women, especially at the placental site. Studies suggest that the coronavirus binds to ACE-2 to enter the human cell, causing deregulation of the renin-angiotensin-aldosterone system and in the ratio between angiotensin-II and angiotensin-1-7, inducing manifestations suggestive of preeclampsia. Furthermore, the cytokine storm leads to endothelial dysfunction, vasculopathy and thrombus formation, also present in preeclampsia.
The studies retrieved in this review suggest that there is a possible overlap of pathophysiological interactions between COVID-19 and preeclampsia, which mainly involve ACE-2 and endothelial dysfunction. Given that preeclampsia courses with progressive clinical and laboratory alterations, a highly quality prenatal care may be able to detect specific clinical and laboratory parameters to differentiate a true preeclampsia superimposed by covid-19, as well as cases with hypertensive manifestations resulting from viral infection.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(3):142-148
To understand the impact of the coronavirus disease 2019 pandemic on in vitro fertilization (IVF) clinical pregnancy rates and analyze factors that may have influenced their outcome.
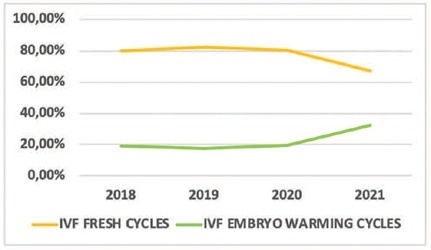
This was a retrospective observational study conducted at a tertiary-care Brazilian fertility center. All fresh IVF and embryo warming cycles performed from March 11 to December 31, 2018–2021 were analyzed, and their data were used to calculate fertilization, embryo cleavage, cycle cancellation, embryo transfer (ET), and clinical pregnancy rates. Statistical tests were used to evaluate the alterations found. Logistic regression models were used to explore the association of the categorical variables with the observed clinical pregnancy rates. Data from 2018 and 2019 (prepandemic) and 2020 and 2021 (pandemic) were grouped.
A total of 756 cycles were analyzed (n = 360 prepandemic and n = 396 pandemic). The age group of the patients, fertilization rates, and cleavage rates did not have significant differences (p > 0.05). There was a reduction in the percentage of fresh IVF and an increase in embryo warming cycles (p = 0.005) during the pandemic. There was also an increase in fresh cycle cancellations (p < 0.001) and a reduction in ET rates (p < 0.001). The pandemic had a negative impact on clinical pregnancy rates (p < 0.001) especially due to the increase in fresh cycle cancellations (p < 0.001).
Embryo warming cycles with subsequent frozen-thawed ET were presented as a viable alternative to continue assisted reproductive treatments against pandemic restrictions on fresh cycles, ensuring clinical pregnancy, albeit at a lower rate than that of the prepandemic period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):567-572
To compare death rates by COVID-19 between pregnant or postpartum and nonpregnant women during the first and second waves of the Brazilian pandemic.
In the present population-based evaluation data from the Sistema de Informação da Vigilância Epidemiológica da Gripe (SIVEP-Gripe, in the Portuguese acronym), we included women with c (ARDS) by COVID-19: 47,768 in 2020 (4,853 obstetric versus 42,915 nonobstetric) and 66,689 in 2021 (5,208 obstetric versus 61,481 nonobstetric) and estimated the frequency of in-hospital death.
We identified 377 maternal deaths in 2020 (first wave) and 804 in 2021 (second wave). The death rate increased 2.0-fold for the obstetric (7.7 to 15.4%) and 1.6-fold for the nonobstetric groups (13.9 to 22.9%) from 2020 to 2021 (odds ratio [OR]: 0.52; 95% confidence interval [CI]: 0.47–0.58 in 2020 and OR: 0.61; 95%CI: 0.56– 0.66 in 2021; p < 0.05). In women with comorbidities, the death rate increased 1.7-fold (13.3 to 23.3%) and 1.4-fold (22.8 to 31.4%) in the obstetric and nonobstetric groups, respectively (OR: 0.52; 95%CI: 0.44–0.61 in 2020 to OR: 0.66; 95%CI: 0.59–0.73 in 2021; p <0.05). In women without comorbidities, the mortality rate was higher for nonobstetric (2.4 times; 6.6 to 15.7%) than for obstetric women (1.8 times; 5.5 to 10.1%; OR: 0.81; 95%CI: 0.69–0.95 in 2020 and OR: 0.60; 95%CI: 0.58–0.68 in 2021; p <0.05).
There was an increase in maternal deaths from COVID-19 in 2021 compared with 2020, especially in patients with comorbidities. Death rates were even higher in nonpregnant women, with or without comorbidities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(2):194-200
To analyze the existing scientific literature to find out if the coronavirus disease 2019 (COVID-19) pandemic has an effect on gynecological health.
We performed an integrative review of articles published between April 2020 and April 2021 on the PubMed, SciELO, and LILACS databases, using COVID-19 and the following relevant terms: Menstrual change; Ovarian function; Violence against women; Contraception; HPV; Mental health; and Urogynecology.
Among the eligible studies found, editorials and primary research articles, which describe the dynamics between severe acute respiratory syndrome coronavirus (SARS-CoV-2) infection (the cause of the COVID-19 pandemic) and gynecological health, were included.
Through qualitative synthesis, data were extracted from the included publications and from guidelines of national and international societies of gynecology.
The 34 publications included in the present study showed that some factors of the SARS-CoV-2 infection, and, consequently, the COVID-19 pandemic, might be associated with menstrual abnormalities, effects on contraception, alterations in steroid hormones, changes in urogynecological care, effects on women’s mental health, and negative impact on violence against women.
The COVID-19 pandemic has significantly impacted the health of women. The scientific community encourages the development of recommendations for specialized care for women and strategies to prevent and respond to violence during and after the COVID-19 pandemic.