-
Review Article12-04-2024
Female genital tract microbiome: the influence of probiotics on assisted reproduction
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo82
Abstract
Review ArticleFemale genital tract microbiome: the influence of probiotics on assisted reproduction
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo82
Views229Abstract
Assisted reproductive technology (ART) has been evolving since 1978, with the number of techniques performed increasing over the years. Despite continued advances, some couples continue to have difficulties getting pregnant, and it has recently been considered that the microbiome of the female genital tract (FGT) may influence embryo implantation and the establishment of pregnancy. This review aims to evaluate the role of probiotics on reproductive outcomes in infertile women on ART. A search throughout medical databases was performed, and six articles met the criteria. Five studies showed improvements in pregnancy rates, with only one demonstrating statistical significance. One article showed no improvement but reported a statistically significant reduction in the miscarriage rate in the probiotic group. Further research is needed to evaluate the true potential of probiotics, namely to assess whether they effectively modulate the FGT microbiome and if these changes are maintained over time.
Key-words Abortion, spontaneousEmbryo implantationGenitalia, femaleInfertility, femalePregnancy outcomePregnancy rateProbioticsReproductive techniques, assisted, MicrobiotaSee more -
Original Article05-16-2022
One Plus One is Better than Two: An Approach Towards a Single Blastocyst Transfer Policy for All IVF Patients
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):578-585
Abstract
Original ArticleOne Plus One is Better than Two: An Approach Towards a Single Blastocyst Transfer Policy for All IVF Patients
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):578-585
Views214See moreAbstract
Objective
It is known that the single embryo transfer (SET) is the best choice to reduce multiples and associated risks. The practice of cryopreserving all embryos for posterior transfer has been increasingly performed for in vitro fertilization (IVF) patients at the risk of ovarian hyperstimulation syndrome or preimplantation genetic testing for aneuploidy. However, its widespread practice is still controverse. The aim of this study was to evaluate how effective is the transfer of two sequential SET procedures compared with a double embryo transfer (DET) in freeze-only cycles.
Methods
This retrospective study reviewed 5,156 IVF cycles performed between 2011 and 2019, and 506 cycles using own oocytes and freeze-only policy with subsequent elective frozen-thawed embryo transfers (eFET) were selected for this study. Cycles having elective SET (eSET, n = 209) comprised our study group and as control group we included cycles performed with elective DET (eDET, n = 291). In the eSET group, 57 couples who had failed in the 1st eSET had a 2nd eFET, and the estimated cumulative ongoing pregnancy rate was calculated and compared with eDET.
Results
After the 1st eFET, the ongoing pregnancy rates were similar between groups (eSET: 35.4% versus eDET: 38.5%; p =0.497), but the estimated cumulative ongoing pregnancy rate after a 2nd eFET in the eSET group (eSET + SET) was significantly higher (48.8%) than in the eDET group (p < 0.001). Additionally, the eSET +SET group had a 2.7% rate of multiple gestations, which is significantly lower than the eDET group, with a 30.4% rate (p < 0.001).
Conclusion
Our study showed the association of freeze-only strategy with until up to two consecutive frozen-thawed eSETs resulted in higher success rates than a frozenthawed DET, while drastically reducing the rate of multiple pregnancies.
-
Original Article02-28-2022
Is There Any Effect of the Physician Performing Embryo Transfer in IVF-ICSI Treatment: A Prospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):19-24
Abstract
Original ArticleIs There Any Effect of the Physician Performing Embryo Transfer in IVF-ICSI Treatment: A Prospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):19-24
Views139See moreAbstract
Objective
To evaluate whether there is an effect of the physician who transfers the embryos on pregnancy rates in in vitro fertilization-intracytoplasmic sperm injection (IVF-ICSI) treatment.
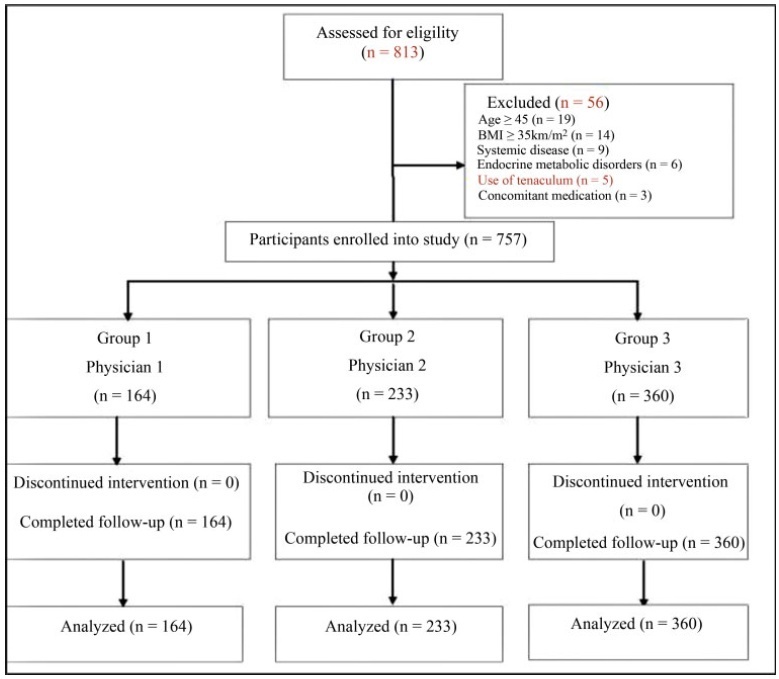
Methods
A total of 757 participants were analyzed between 2012 and 2017. Participants were classified according to 3 physicians who transferred the embryos: ([group 1=164 patients]; [group 2=233 patients]; [group 3=360 patients]). Baseline parameters and IVF-ICSI outcomes were compared between the groups.
Results
No differences were determined between the groups regarding the baseline parameters (age, age subgroups [20-29, 30-39, and ≥ 40 years old)], body mass index (BMI), smoking status, infertility period, cause of infertility, baseline follicle stimulating hormone, luteinizing hormone, estradiol (E2), thyroid stimulating hormone, prolactin levels, antral follicle count, duration of stimulation, stimulation protocol, gonadotropin dose required, maximum E2 levels, progesterone levels, endometrial thickness on human chorionic gonadotropin (hCG) administration and transfer days (p>0.05). The numbers of oocytes retrieved,metaphase II (MII), 2 pronucleus (2PN), transferred embryo, fertilization rate, day ofembryo transfer, the catheter effect and embryo transfer technique, and clinical pregnancy rates (CPRs) were also comparable between the groups (p>0.05).
Conclusion
Our data suggests that the physician who transfers the embryos has no impact on CPRs in patients who have undergone IVF-ICSI, but further studies with more participants are required to elucidate this situation.
-
Original Article07-29-2009
The age as a predictive factor in in vitro fertilization cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):230-234
Abstract
Original ArticleThe age as a predictive factor in in vitro fertilization cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):230-234
DOI 10.1590/S0100-72032009000500005
Views142See morePURPOSE: to evaluate the patient's age as an outcome predictor in an in vitro fertilization (IVF) program. METHODS: transversal study, which has included 302 women with ages varying from 24 to 46 years old, submitted to IVF, from May 2005 to July 2007. The patients were divided in three groups, according to their age: G<35 (n=161), G 36-39 (n=89) e G>40 (n=52). The number of collected oocytes, the fertilization rates, the number of transferred embryos, the embryonary quality and the pregnancy rate were evaluated. Statistical analysis was realized through Kruskal-Wallis variance analysis and χ2 test. RESULTS: in the G<35 group, an average of 8.8 oocytes by patient was obtained; in the G 36-49 group, 7.4; and in the G>40 group, 1.6. The number of oocytes obtained in G>40 group was significantly lower than in the other two groups (p<0.001).The fertilization rate was similar in the three groups, 61.4, 65.8 e 64.6% (p=0.2288), respectively. The percentage of good quality embryos was not statistically different among the three groups either, with rates of 57.4, 63.2 and 56.0% (p=0.2254), respectively. The average number of transferred embryos in each group was 3.1 (G<35), 2.8 (G 36-39) and 1.5 (G>40), respectively, with statistically significant decrease in the G>40 group (p<0.001). Concerning pregnancy rates, the G>40 group has presented a rate of 9.6%, a result which is significantly lower (p=0.0330) than the one presented by the G<35 and G 36-39 groups (26.1 e 27.0%, respectively), with no significant difference between themselves. CONCLUSIONS: though the embryonary quality is not different among women from different age groups, the number of collected oocytes, the number of transferred embryos and the pregnancy rate indicate that the women's age is an important predictive factor of success for the techniques of assisted reproduction and should be taken into consideration when this kind of treatment is proposed to women over 40.
-
Original Article09-04-2008
Tubal reanastomosis: analysis of the results of 30 years of treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(6):294-299
Abstract
Original ArticleTubal reanastomosis: analysis of the results of 30 years of treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(6):294-299
DOI 10.1590/S0100-72032008000600005
Views110PURPOSE: to verify the ratio of intra-uterine gestation in patients submitted to recanalization in the Hospital Regional da Asa Sul in the last 30 years and to assess the rate of ectopic gestation of such procedures, the influence of age and time interval between salpingectomy and recanalization in the therapeutic success. METHODS: medical files of 71 patients were analyzed, after exclusion of those presenting other alterations that could influence fertility prognosis, plus the cases when recanalization was impossible. Variables collected were: occurrence of intra-uterine gestation, coming to term or to abortion; occurrence of ectopic pregnancy after salpingectomy; no-conception after reversion, women's age at the recanalization, and time interval between salpingectomy and its reversion. RESULTS: there has been a pregnancy rate of 67.6%, 73.2% for bilateral recanalization and 46.6% for unilateral, as well as 5.6% of ectopic pregnancies. Concerning the patients' age group, it was observed a pregnancy rate of 33%, from 20 to 24; 60%, from 25 to 29; 69.2%, from 30 to 34; 65%, from 35 to 39, and 42.9%, from 40 to 44 years old. The number of cases was small for age the groups 20 to 24 and 40 to 44 years old. The time interval between salpingectomy and recanalization (TISR) has varied from one to 18 years. TISR has been divided in three groups presenting the following pregnancy rates: one to six year interval, 59%; seven to 12, 66.6%; 13 to 18, 57%. CONCLUSIONS: gestation rate has been 67.6%, 5.6% being ectopic. In the comparison of age groups, there has been no significant influence of age on the therapeutic success of patients from 25 to 39 years old. Sterility duration did not influence the reversion results.
Key-words Anastomosis, surgicalMicrosurgeryPregnancy ratePregnancy, ectopicSterilization reversalTreatment outcomeSee more -
Original Article07-02-2008
Safe gametes acquisition through association of seminal processing techniques with HIV serodiscordant couples
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(4):171-176
Abstract
Original ArticleSafe gametes acquisition through association of seminal processing techniques with HIV serodiscordant couples
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(4):171-176
DOI 10.1590/S0100-72032008000400003
Views139See morePURPOSE: the propose of this study was to analyze the clinical and laboratorial parameters of patients submitted to human assisted reproduction techniques with association of sperm processing techniques, in order to remove virus particles from semen samples of couples in which men was infected by human immunodeficiency virus (HIV). METHODS: it was assessed 11 intracytoplasmatic sperm injection (ICSI) cycles from couples whose men were HIV seropositive (HIV Group), and 35 cycles in which semen donors' samples were used in ICSI procedures (Control Group). Semen samples from Control Group were submitted to routine semen analysis, sperm wash and cryopreservation. The man from HIV Group received previous antibiotic therapy; the semen samples were analyzed routinely and prepared by sperm wash and density gradient method before cryopreservation. Those samples were evaluated to viral load and ICSI was performed when no HIV was detected. RESULTS: regards to semen analysis the groups were similar to sperm concentration and progressive motility. Nevertheless, the percentage of sperm with normal morphology were higher on Control Group (14.3%) than HIV (5.8%; p=0.002). On embryo parameters assessment, the normal fertilization (CT: 74.7% and HIV: 71.7; p=0.838, respectively) and good embryos rate (CT: 42.4% and HIV: 65.1%; p=0.312, respectively) were comparable. On the other hand, the Control Group presented better clinic results than HIV Group (ongoing pregnancy rate: 52.9% versus 12.5%; p=0.054, and implantation rate: 42.6 versus 10.4%; p=0.059, respectively), however the differences were not statistically significant. After delivery, no seroconversion was observed on mother and child. CONCLUSIONS: the association of sperm processing techniques in order to remove HIV from semen samples does not influence in laboratorial parameters of assisted reproduction techniques cycles. On the other hand, it has been demonstrated excellent results getting safety gametes to serodiscordant couples.
-
Original Article04-10-2005
Outcome of assisted reproductive technologies in women with oocyte donation in the treatment cycle
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(11):661-664
Abstract
Original ArticleOutcome of assisted reproductive technologies in women with oocyte donation in the treatment cycle
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(11):661-664
DOI 10.1590/S0100-72032005001100005
Views54See morePURPOSE: to compare the outcome of treatment in patients undergoing assisted reproductive technology (ART) cycles who donated eggs during their own ART treatment with the outcome of patients undergoing ART without egg donation. METHODS: we studied retrospectively the pregnancy and implantation rates of 50 patients who donated eggs during the course of their ART treatment (donor group), and the pregnancy and implantation rates of 50 patients who underwent ART cycles and kept all their eggs (non-donor group). between the years 2001-2003. The inclusion criteria used were as follows: age <35 years old, normal menstrual cycles, FSH<10 mIU/mL, first attempt of ART treatment and more than six mature oocytes retrieved. The results were analyzed statistically using the chi2 test. RESULTS: both groups were comparable in terms of age, indication, and duration of infertility. The mean age was 30.6 years for the donor group and 31.1 years for the non-donor group. All the patients of the donor group produced more than 6 eggs. From the donor group we collected 590 oocytes; 215 eggs were donated to recipients (36.5%) and 152 embryos were transferred. A total of 15 pregnancies were achieved (pregnancy rate per transfer: 30%); the implantation rate was 11.2% and there were 2 miscarriages (miscarriage rate: 13.3%). From the non-donor group, 545 oocytes were collected and 153 embryos were transferred. A total 17 pregnancies were achieved (pregnancy rate per transfer: 34%); the implantation rate was 14.3% and there were 3 miscarriages (miscarriage rate: 17.6%). The pregnancy and implantation rates were similar in both groups, and there were no significant statistical differences regarding the miscarriage rate (p>0.05). CONCLUSION: this study suggests that in patients who produce more than 6 oocytes, egg donation in the treatment cycle does not influence adversely the outcome of ART cycles and does not increase the miscarriage rate.
-
Original Article09-08-2003
Comparison between three embryo scoring systems as predictive of the outcome of in vitro fertilization
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(3):177-183
Abstract
Original ArticleComparison between three embryo scoring systems as predictive of the outcome of in vitro fertilization
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(3):177-183
DOI 10.1590/S0100-72032003000300006
Views114See morePURPOSE: to evaluate three embryo scoring systems specific for 3-day embryos and to correlate them with positive in vitro fertilization outcome. METHOD: retrospective study of the In Vitro Fertilization Program of the University Hospital, Faculty of Medicine of Ribeirão Preto, University of São Paulo. A total of 137 patients submitted to the transfer of 439 embryos were evaluated. The main outcomes measured were pregnancy and implantation rates. RESULTS: a significant difference in the three scoring systems was observed between pregnant (n=53) and non-pregnant (n=84) patients (p<0.0001). In the first embryo scoring system, in which cell number alone was used, higher pregnancy (70%) and implantation rates (42%) were observed when embryos with a mean blastomere number higher than 8 were transferred. Scoring system 2, based on a total four-point score (cleavage stage, blastomere number, fragmentation and symmetry), showed increased pregnancy (52.8%) and implantation rates (31%) for scores above 2. Scoring system 3, based on cell number and morphological criteria, also showed higher pregnancy and implantation rates with increasing average scores of the transferred embryos. CONCLUSION: the three scoring systems assessed in 3-day embryos were positively correlated with pregnancy and implantation rates.


