Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):562-568
DOI 10.1590/SO100-720320140005161
To verify the existence of associations between different maternal ages and the perinatal outcomes of preterm birth and intrauterine growth restriction in the city of São Luís, Maranhão, Northeastern Brazil.
A cross-sectional study using a sample of 5,063 hospital births was conducted in São Luís, from January to December 2010. The participants comprise the birth cohort for the study "Etiological factors of preterm birth and consequences of perinatal factors for infant health: birth cohorts from two Brazilian cities" (BRISA). Frequencies and 95% confidence intervals were used to describe the results. Multiple logistic regression models were applied to assess the adjusted odds ratio (OR) of maternal age associated with the following outcomes: preterm birth and intrauterine growth restriction.
The percentage of early teenage pregnancy (12–15 years old) was 2.2%, and of late (16–19 years old) was 16.4%, while pregnancy at an advanced maternal age (>35 years) was 5.9%. Multivariate analyses showed a statistically significant increase in preterm births among females aged 12–15 years old (OR=1.6; p=0.04) compared with those aged 20–35 years. There was also a higher rate in preterm births among females aged 16–19 years old (OR=1.3; p=0.01). Among those with advanced maternal age (>35 years old), the increase in the prevalence of preterm birth had only borderline statistical significance (OR=1.4; p=0.05). There was no statistically significant association between maternal age and increased prevalence of intrauterine growth restriction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):461-466
DOI 10.1590/SO100-720320140005029
To compare clinical and laboratory characteristics, obstetric and perinatal outcomes of patients with pre-eclampsia versus gestational hypertension.
A retrospective study was carried out to analyze medical records of patients diagnosed with pre-eclampsia and gestational hypertension whose pregnancies were resolved within a period of 5 years, for a total of 419 cases. We collected clinical and laboratory data, obstetric and perinatal outcomes. Comparisons between groups were performed using the test suitable for the variable analyzed: unpaired t test, Mann-Whitney U test or χ2test, with the level of significance set at p<0.05.
Were evaluated 199 patients in the gestational hypertension group (GH) and 220 patients in the pre-eclampsia group (PE). Mean body mass index was 34.6 kg/m2 in the GH group and 32.7 kg/m2 in the PE group, with a significant difference between groups. The PE group showed higher systolic and diastolic blood pressure and higher rates of abnormal values in the laboratory tests, although the mean values were within the normal range. Cesarean section was performed in 59.1% of cases of PE and in 47.5% of the GH group; and perinatal outcomes in terms of gestational age and birth weight were significantly lower in the PE group.
Women with gestational hypertension exhibit epidemiological characteristics of patients at risk for chronic diseases. Patients with pre-eclampsia present clinical and laboratory parameters of greater severity, higher rates of cesarean delivery and worse maternal and perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(2):65-71
DOI 10.1590/S0100-72032014000200004
To analyze the relationships among gestational risk, type of delivery and
immediate maternal and neonatal repercussions.
A retrospective cohort study based on secondary data was conducted in a
university maternity hospital. A total of 1606 births were analyzed over a 9-month
period. Epidemiological, clinical, obstetric and neonatal characteristics were
compared according to the route of delivery and the gestational risk characterized
on the basis of the eligibility criteria for high clinical risk. The occurrence of
maternal and neonatal complications during hospitalization was analyzed according
to gestational risk and cesarean section delivery using univariate and
multivariate logistic analysis.
The overall rate of cesarean sections was 38.3%. High gestational risk was
present in 50.2% of births, mainly represented by hypertensive disorders and fetal
malformations. The total incidence of cesarean section, planned cesarean section
or emergency cesarean section was more frequent in pregnant women at gestational
high risk (p<0.001). Cesarean section alone did not influence maternal outcome,
but was associated with poor neonatal outcome (OR 3.4; 95%CI 2.7-4.4). Gestational
high risk was associated with poor maternal and neonatal outcome (OR 3.8; 95%CI
1.3-8.7 and OR 17.5; 95%CI 11.6-26.3, respectively). In multivariate analysis, the
ratios were maintained, although the effect of gestational risk has determined a
reduction in the OR of the type of delivery alone from 3.4 (95%CI 2.7-4.4) to 1.99
(95%CI 1.5-2.6) for adverse neonatal outcome.
Gestational risk was the main factor associated with poor maternal and neonatal
outcome. Cesarean delivery was not directly associated with poor maternal outcome
but increased the chances of unfavorable neonatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(11):516-522
DOI 10.1590/S0100-72032013001100007
PURPOSE: To analyze the impact of vaginal delivery after a previous cesarean section on perinatal outcomes. METHODS: Case-control study with selection of incident cases and consecutive controls. Maternal and perinatal variables were analyzed. We compared secundiparas who had a vaginal delivery after a previous cesarean delivery (VBAC) (n=375) with secundiparas who had a second cesarean section (CS) (n=375). Inclusion criteria were: secundiparas who underwent a cesarean section in the previous pregnancy; singleton and term pregnancy; fetus in vertex presentation, with no congenital malformation; absence of placenta previa or any kind of bleeding in the third quarter of pregnancy. RESULTS: The rate of vaginal delivery was 45.6%, and 20 (5.3%) women had forceps deliveries. We found a significant association between VBAC and mothers younger than 19 years (p<0.01), Caucasian ethnicity (p<0.05), mean number of prenatal care visits (p<0.001), time of premature rupture of membranes (p<0.01), labor duration shorter than 12 hours (p<0.04), Apgar score lower than seven at 5th minute (p<0.05), fetal birth trauma (p<0.01), and anoxia (p<0.006). In the group of newborns delivered by cesarean section, we found a higher frequency of transient tachypnea (p<0.014), respiratory disorders (p<0.048), and longer time of stay in the neonatal intensive care unit (p<0.016). There was only one case of uterine rupture in the VBAC group. The rate of neonatal mortality was similar in both groups. CONCLUSIONS: Vaginal delivery in secundiparas who had previous cesarean sections was associated with a significant increase in neonatal morbidity. Further studies are needed to develop strategies aimed at improving perinatal results and professional guidelines, so that health care professionals will be able to provide their patients with better counseling regarding the choice of the most appropriate route of delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):35-39
DOI 10.1590/S0100-72032014000100008
O objetivo do presente estudo longitudinal foi avaliar o valor da ultrassonografia Doppler das artérias uterinas no segundo e terceiro trimestres de gestação para a predição de desfecho adverso da gravidez em mulheres de baixo risco.
De julho de 2011 até agosto de 2012, 205 gestantes de feto único atendidas em nossa clínica de pré-natal foram incluídas no presente estudo prospectivo e avaliadas em termos de dados demográficos e obstétricos. As pacientes foram submetidas à avaliação de ultrassom durante o segundo e terceiro trimestres, incluindo avaliação Doppler das artérias uterinas bilaterais, visando determinar os valores do índice de pulsatilidade (IP) e do índice de resistência (IR), bem como a presença de incisura diastólica precoce. O desfecho do presente estudo foi a avaliação da sensibilidade, especificidade, valor preditivo positivo (VPP) e valor negativo preditivo (VNP) da ultrassonografia Doppler das artérias uterinas para a predição de desfechos adversos da gravidez, incluindo pré-eclâmpsia, natimortalidade, descolamento prematuro da placenta e trabalho de parto prematuro.
A média de idade das gestantes foi de 26,4±5,11 anos. Os valores de IP e IR das artérias uterinas para o primeiro (IP: 1,1±0,42 versus 1,53±0,59, p=0,002; IR: 0,55±0,09 versus 0.72±0.13, p=0,000, respectivamente) e para o terceiro trimestre (IP: 0,77±0,31 versus 1,09±0,46, p=0,000; IR: 0,46±0,10 versus 0,60±0,14, p=0,010, respectivamente) foram significativamente maiores em pacientes com desfecho adverso da gravidez em relação às mulheres com desfecho normal. A combinação de IP e IR > percentil 95 e a presença de incisura bilateral apresentou sensibilidade e especificidade de 36,1 e 97%, respectivamente, no segundo trimestre e de 57,5 e 98,2% no terceiro trimestre.
Com base no presente estudo, o Doppler das artérias uterinas parece ser ferramenta valiosa para a predição de uma variedade de desfechos adversos no segundo e terceiro trimestres de gestação.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):35-39
DOI 10.1590/S0100-72032014000100008
The aim of this longitudinal study was to investigate the value of uterine artery Doppler sonography during the second and third trimesters in the prediction of adverse pregnancy outcome in low-risk women.
From July 2011 to August 2012, a total of 205 singleton pregnant women presenting at our antenatal clinic were enrolled in this prospective study and were assessed for baseline demographic and obstetric data. They underwent ultrasound evaluation at the time of second and third trimesters, both included Doppler assessment of bilateral uterine arteries to determine the values of the pulsatility index (PI) and resistance index (RI) and presence of early diastolic notch. The endpoint of this study was assessing the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of Doppler ultrasonography of the uterine artery, for the prediction of adverse pregnancy outcomes including preeclampsia, stillbirth, placental abruption and preterm labor.
The mean age of cases was 26.4±5.11. The uterine artery PI and RI values for both second (PI: 1.1±0.42 versus 1.53±0.59, p=0.002; RI: 0.55±0.09 versus 0.72±0.13, p=0.000 respectively) and third-trimester (PI: 0.77±0.31 versus 1.09±0.46, p=0.000; RI: 0.46±0.10 versus 0.60±0.14, p=0.010 respectively) evaluations were significantly higher in patients with adverse pregnancy outcome than in normal women. Combination of PI and RI >95th percentile and presence of bilateral notch in second trimester get sensitivity and specificity of 36.1 and 97% respectively, while these measures were 57.5 and 98.2% in third trimester.
According to our study, it seems that uterine artery Doppler may be a valuable tool for the prediction of a variety of adverse outcomes in second and third trimesters.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(4):148-152
DOI 10.1590/S0100-72032013000400003
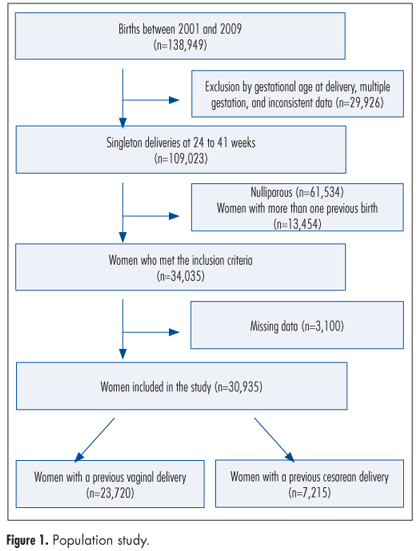
PURPOSE: To examine obstetric outcomes in the second birth of women who had undergone a previous cesarean delivery. METHODS: This was a large hospital-based retrospective cohort study. We included pregnant women who had a previous delivery (vaginal or cesarean) attending their second birth from 2001 to 2009. Main inclusion criteria were singleton pregnancies and delivery between a gestation of 24 and 41 weeks. Two cohorts were selected, being women with a previous cesarean delivery (n=7,215) and those with a vaginal one (n=23,720). Both groups were compared and logistic regression was performed to adjust for confounding variables. The obstetric outcomes included uterine rupture, placenta previa, and placental-related complications such as placental abruption, preeclampsia, and spontaneous preterm delivery. RESULTS: Women with previous cesarean delivery were more likely to have adverse outcomes such as uterine rupture (OR=12.4, 95%CI 6.8-22.3), placental abruption (OR=1.4, 95%CI 1.1-2.1), preeclampsia (OR=1.4, 95%CI 1.2-1.6), and spontaneous preterm delivery (OR=1.4, 95%CI 1.1-1.7). CONCLUSIONS: Individuals with previous cesarean section have adverse obstetric outcomes in the subsequent pregnancy, including uterine rupture, and placental-related disorders such as preeclampsia, spontaneous preterm delivery, and placental abruption.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(2):71-77
DOI 10.1590/S0100-72032013000200006
PURPOSE: To evaluate the anthropometric characteristics of morbidity and mortality of premature newborns (NB) of hypertensive mothers according to the presence or absence of flow (DZ) or reverse (DR) diastolic flow in the dopplervelocimetry of the umbilical artery. METHODS: A prospective study was conducted on preterm newborns of pregnant women with hypertension between 25 and 33 weeks of gestational age, submitted to umbilical artery Doppler study during the five days before delivery. Delivery occurred at Hospital Regional da Asa Sul, Brasília - Federal District, between November 1st, 2009 and October 31st, 2010. The infants were stratified into two groups according to the results of Doppler velocimetry: Gdz/dr=absent end-diastolic velocity waveform or reversed end-diastolic velocity waveform, and Gn=normal Doppler velocimetry. Anthropometric measurements at birth, neonatal morbidity, and mortality were compared between the two groups. RESULTS: We studied 92 infants, as follows: Gdz/dr=52 infants and Gn=40 infants. In Gdz/dr, the incidence of infants small for gestational age was significantly greater, with a relative risk of 2.5 (95%CI 1.7 - 3.7). In Gdz/dr, infants remained on mechanical ventilation for a longer time: median 2 (0‒28) and Gn median 0.5 (0‒25) p=0.03. The need for oxygen at 28 days was higher in G dz/dr comparing to Gn (33 versus 10%; p=0.01). Neonatal mortality was higher in Gdz/dr compared to Gn (36 versus 10%; p=0.03; relative risk of 1.6; 95%CI 1.2‒2.2). Logistic regression showed that, with each 100 grams lower birth weight, the chance of death increased 6.7 times in G dz/dr (95%CI 2.0 - 11.3; p<0.01). CONCLUSION: In preterm infants of mothers with hypertensive changes in Doppler velocimetry of the umbilical artery, intrauterine growth restriction and neonatal prognosis are often worse, with a high risk of death related to birth weight.