-
Original Article
Psychometric Properties of Brief Screening Tests for Alcohol Use Disorders during Pregnancy in Argentina
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):322-329
07-01-2017
Summary
Original ArticlePsychometric Properties of Brief Screening Tests for Alcohol Use Disorders during Pregnancy in Argentina
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):322-329
07-01-2017Views118See moreAbstract
Background
Considering the physical, mental and behavioral problems related to fetal alcohol exposure, prenatal clinical guides suggest a brief evaluation of alcohol consumption during pregnancy to detect alcohol intake and to adjust interventions, if required. Even if any alcohol use should be considered risky during pregnancy, identifying women with alcohol use disorders is important because they could need a more specific intervention than simple advice to abstain. Most screening tests have been developed and validated in male populations and focused on the long-term consequences of heavy alcohol use, so they might be inappropriate to assess consumption in pregnant women.
Objective
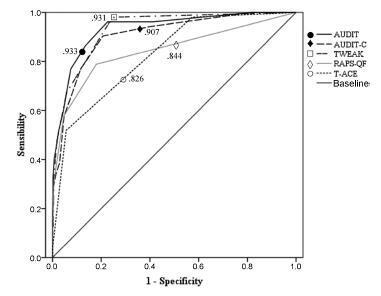
To analyze the internal reliability and validity of the alcohol screening instruments Alcohol Use Disorders Identification Test (AUDIT), Alcohol Use Disorders IdentificationTest- Consumption (AUDIT-C), Tolerance, Worried, Eye-Opener, Amnesia and Cut-Down (TWEAK), Rapid Alcohol Problems Screen - Quantity Frequency (RAPSQF) and Tolerance, Annoyed, Cut-Down and Eye-Opener (T-ACE) to identify alcohol use disorders in pregnant women.
Methods
A total of 641 puerperal women were personally interviewed during the 48 hours after delivery. The receiver operating characteristics (ROC) curves and the sensitivity and specificity of each instrument using different cut-off points were analyzed.
Results
All instruments showed areas under the ROC curves above 0.80. Larger areas were found for the TWEAK and the AUDIT. The TWEAK, the T-ACE and the AUDIT-C showed higher sensitivity, while the AUDIT and the RAPS-QF showed higher specificity. Reliability (internal consistency) was low for all instruments, improving when optimal cut-off points were used, especially for the AUDIT, the AUDIT-C and the RAPS-QF.
Conclusions
In other cultural contexts, studies have concluded that T-ACE and TWEAK are the best instruments to assess pregnant women. In contrast, our results evidenced the low reliability of those instruments and a better performance of the AUDIT in this population.
-
Original Article
Potential Drug Interactions and Drug Risk during Pregnancy and Breastfeeding: An Observational Study in a Women’s Health Intensive Care Unit
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(6):258-264
06-01-2017
Summary
Original ArticlePotential Drug Interactions and Drug Risk during Pregnancy and Breastfeeding: An Observational Study in a Women’s Health Intensive Care Unit
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(6):258-264
06-01-2017Views100See moreAbstract
Introduction
In the pregnancy-puerperal cycle, women may develop complications that require admission to the Intensive Care Unit (ICU). Thus, special attention to pharmacotherapy is necessary, particularly to potential drug interactions (PDIs) and to the effect of the drugs on the fetus and newborn.
Objective
The aim of this study was to determine the profile of PDIs and the potential risk of drugs used during pregnancy and breastfeeding among patients admitted to the ICU.
Methods
We conducted an observational, cross-sectional and prospective study, including pregnant and breastfeeding women admitted to the ICU at the Women’s Hospital of a university in the city of Campinas, Brazil, for one year. Online databases were used to identify and classify the PDIs and the potential risk of the drugs used during pregnancy and breastfeeding.
Results
We evaluated 305 prescriptions of 58 women, 31 pregnant and 27 breastfeeding, and 284 (91%) prescriptions presented PDIs. A total of 175 different combinations of PDIs were identified in the prescriptions, and adverse effects caused by the simultaneous use of drugs were not actually observed in the clinical practice. A total of 26 (1.4%) PDIs were classified as contraindicated. We identified 15 (13.8%) drugs prescribed with risk D, and 2 (1.8%) with risk X for pregnant women, as well as 4 (4.9%) drugs prescribed with high risk for breastfeeding women.
Conclusions
This study demonstrates that there is a high incidence of PDIs in prescriptions. Most drugs used by pregnant and breastfeeding women at the ICU did not present serious risks to their fetus and newborns, but sometimes drugs with risk D or X are necessary in the course of the treatment.
-
Original Article
Salivary Iron (Fe) Ion Levels, Serum Markers of Anemia and Caries Activity in Pregnant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(3):94-101
03-01-2017
Summary
Original ArticleSalivary Iron (Fe) Ion Levels, Serum Markers of Anemia and Caries Activity in Pregnant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(3):94-101
03-01-2017Views152See moreAbstract
Introduction
Anemia is a very frequent event among pregnant women. There are evidences of differences in the incidence of dental caries between pregnant and nonpregnant women, but the relationship between salivary iron (Fe) and serummarkers of anemia and caries development has not been investigated.
Objective
To evaluate the correlation between salivary (Fe) and serum iron (Fe, ferritin and hemoglobin) parameters in pregnant women with the development of dental caries.
Methods
A prospective cohort was conducted with 59 women. The outcome of interest was represented by new dental caries lesions during pregnancy, using the Nyvad criteria. Pregnant women were evaluated at three clinical times: up to the 16th week of gestational age (GA) (T1), in the last trimester of pregnancy (T2), and postpartum (T3), at the Mother and Child Unit ofUniversityHospital of the Universidade Federal doMaranhão.A stimulated saliva sample was collected for biochemical analysis of salivary Fe, and a blood sample was collected early in the morning. The correlation between salivary and serum Fe was evaluated through the Pearson correlation test. Analysis of variance (ANOVA) and Kruskal-Wallis were used to compare the means of anemia parameters at different times. The Student's t and Mann-Whitney tests were used to compare the anemia parameters between the groups of pregnant women (with and without new caries lesions).
Results
SerumFe concentrationswere higher in the first trimester of pregnancy and lower after delivery (p = 0.036). It was also observed that the ferritin concentrations were higher in the first trimester and lower at the end of gestation (p = 0.011). Therewas no association between the expositions of salivary iron and anemia, and the development of dental caries. There was a positive correlation between serum Fe in T1 and salivary Fe in T2 (p < 0.05).
Conclusion
The serummarkers of anemiaweremore prevalent in the last trimester of pregnancy.
-
Case Report
Lactation Induction in a Commissioned Mother by Surrogacy: Effects on Prolactin Levels, Milk Secretion and Mother Satisfaction
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):86-89
02-01-2017
Summary
Case ReportLactation Induction in a Commissioned Mother by Surrogacy: Effects on Prolactin Levels, Milk Secretion and Mother Satisfaction
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):86-89
02-01-2017Views107See moreAbstract
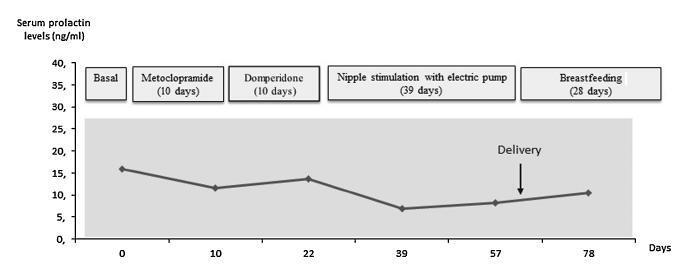
Case report of a 39-year-old intended mother of a surrogate pregnancy who underwent induction of lactation by sequential exposure to galactagogue drugs (metoclopramide and domperidone), nipple mechanical stimulation with an electric pump, and suction by the newborn. The study aimed to analyze the effect of each step of the protocol on serum prolactin levels, milk secretion and mother satisfaction, in the set of surrogacy. Serum prolactin levels and milk production had no significant changes. Nevertheless, themother was able to breastfeed for four weeks, and expressed great satisfaction with the experience. As a conclusion, within the context of a surrogate pregnancy, breastfeeding seems to bring emotional benefits not necessarily related to an increase in milk production.
-
Case Report
Pyometra and Pregnancy with Herlyn-Werner-Wunderlich Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(12):623-628
12-01-2016
Summary
Case ReportPyometra and Pregnancy with Herlyn-Werner-Wunderlich Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(12):623-628
12-01-2016Views151ABSTRACT
We describe a Herlyn-Werner-Wunderlich syndrome (HWWS) patient with previous history of infertility who got pregnant without treatment and presented a pyometra in the contralateral uterus throughout the gestational period, despite multiple antibiotic treatments. Due to the uterus' congenital anomaly and the possibility of ascending infection with subsequent abortion, this pregnancy was classified as high-risk. We believe that the partial horizontal septum in the vagina may have contributed to the closure of the gravid uterus cervix, thus ensuring that the pregnancy came to term, with an uneventful vaginal delivery.
Key-words Herlyn-Werner-Wunderlich syndromemagnetic resonance imaging and ultrasonographyPregnancypyometraSee more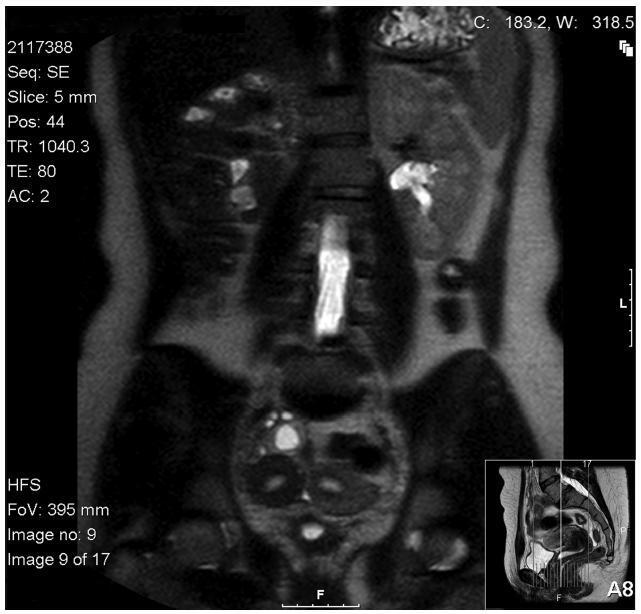
-
Original Articles
Prevalence of Sexual Dysfunction among Expectant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):559-563
11-01-2016
Summary
Original ArticlesPrevalence of Sexual Dysfunction among Expectant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):559-563
11-01-2016Views138See moreAbstract
Purpose
To identify pregnancy as a causative factor of sexual dysfunction among expectant women.
Methods
A prospective study with 225 expectant mothers seen in the prenatal clinic of a federal university. Sexual function was evaluated by means of the Female Sexual Function Index (FSFI), and all domains were analyzed (desire, arousal, lubrication, orgasm, satisfaction, and pain). Initially, a univariate analysis of the sample was done. The averages for each domain according to the risk of sexual dysfunction (FSFI ≤ 26.5) were compared using the Student’s t-test for independent samples. The strength of the correlation between sexual dysfunction and all sociodemographic, clinical and behavioral variables was measured by the Chi-Square (X2) test. Then, odds ratios (ORs) and their confidence intervals were assigned to perform a bivariate analysis. Any p values less than 0.05 were considered significant.
Results
Approximately two-thirds of the women (66.7%) showed signs of risk of sexual dysfunction (FSFI ≤ 26.5). Within these cases, all sexual dysfunction domains (desire, arousal, lubrication, orgasm, satisfaction, and pain) were found to be statistically significant (p < 0.001). The domains most affected were desire (2.67), satisfaction (2.71) and arousal (2.78).
Conclusions
Pregnancy appears to be an important causative factor of sexual dysfunction among pregnant women.
-
Original Articles
HIV Prevalence among Pregnant Women in Brazil: A National Survey
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):391-398
08-01-2016
Summary
Original ArticlesHIV Prevalence among Pregnant Women in Brazil: A National Survey
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):391-398
08-01-2016Views189See moreAbstract
Background
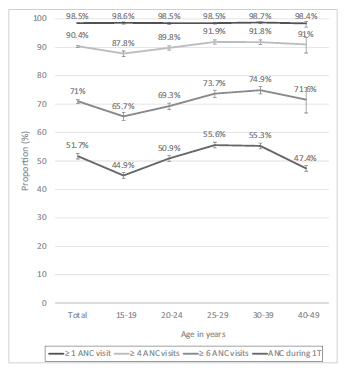
This study was conducted to determine the seroprevalence of HIV among pregnant women in Brazil and to describe HIV testing coverage and the uptake of antenatal care (ANC).
Methods
Between October 2010 and January 2012, a probability sample survey of parturient women aged 15-49 years who visited public hospital delivery services in Brazil was conducted. Data were collected from prenatal reports and hospital records. Dried blood spot (DNS) samples were collected and tested for HIV.We describe the agespecific prevalence of HIV infection and ANC uptake with respect to sociodemographic factors.
Results
Of the 36,713 included women, 35,444 (96.6%) were tested for HIV during delivery admission. The overall HIV prevalence was of 0.38% (95% confidence interval [CI]: 0.31-0.48), and it was highest in: the 30 to 39 year-old age group (0.60% [0.40- 0.88]), in the Southern region of Brazil (0.79% [0.59-1.04]), among women who had not completed primary (0.63% [0.30-1.31]) or secondary (0.67% [0.49-0.97]) school education, and among women who self-reported as Asian (0.94% [0.28-3.10]). The HIV testing coverage during prenatal care was of 86.6% for one test and of 38.2% for two tests. Overall, 98.5% of women attended at least 1 ANC visit, 90.4% attended at least 4 visits, 71% attended at least 6 visits, and 51.7% received ANC during the 1st trimester. HIV testing coverage and ANC uptake indicators increased with increasing age and education level of education, and were highest in the Southern region.
Conclusions
Brazil presents an HIV prevalence of less than 1% and almost universal coverage of ANC. However, gaps in HIV testing and ANC during the first trimester challenge the prevention of the vertical transmission of HIV. More efforts are needed to address regional and social disparities.
-
Original Article
Epidemiological Risk Factors and Perinatal Outcomes of Congenital Anomalies
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):348-355
07-01-2016
Summary
Original ArticleEpidemiological Risk Factors and Perinatal Outcomes of Congenital Anomalies
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):348-355
07-01-2016Views190See moreAbstract
Objectives
To identify the epidemiological risk factors for congenital anomalies (CAs) and the impact of these fetal malformations on the perinatal outcomes.
Methods
This prospective cohort study comprised 275 women whose fetuses had CAs. Maternal variables to establish potential risk factors for each group of CA and perinatal outcomes were evaluated. The primary outcome was CA. Secondary outcomes included: fetal growth restriction (FGR); fetal distress (FD); premature rupture of membranes (PROM); oligohydramnios or polyhydramnios; preterm delivery (PTD); stillbirth; cesarean section; low birth weight; Apgar score < 7 at the 1st and 5th minutes; need for assisted ventilation at birth; neonatal infection; need for surgical treatment; early neonatal death; and hospitalization time. Chi-square (x2) test and multilevel regression analysis were applied to compare the groups and determine the effects of maternal characteristics on the incidence of CAs.
Results
The general prevalence of CAs was of 2.4%. Several maternal characteristics were associated to CAs, such as: age; skin color; level of education; parity; folic acid supplementation; tobacco use; and history of previous miscarriage. There were no significant differences among the CA groups in relation to FGR, FD, PROM, 1-minute Apgar score > 7, and need for assisted ventilation at birth. On the other hand, the prevalence of the other considered outcomes varied significantly among groups. Preterm delivery was significantly more frequent in gastrointestinal tract/abdominal wall defects. The stillbirth rate was increased in all CAs, mainly in isolated fetal hydrops (odds ratio [OR]: 27.13; 95% confidence interval [95%CI]: 2.90-253.47). Hospitalization time was higher for the urinary tract and congenital heart disease groups (p < 0.01). Neonatal death was significantly less frequent in the central nervous system anomalies group.
Conclusion
It was possible to identify several risk factors for CAs. Adverse perinatal outcomes were presented in all CA groups, and may differ according to the type of CA considered.


