-
Original Article07-01-2018
First-trimester Combined Screening Test for Aneuploidies in Brazilian Unselected Pregnancies: Diagnostic Performance of Fetal Medicine Foundation Algorithm
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):384-389
Abstract
Original ArticleFirst-trimester Combined Screening Test for Aneuploidies in Brazilian Unselected Pregnancies: Diagnostic Performance of Fetal Medicine Foundation Algorithm
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):384-389
Views146Abstract
Objective
The main objective of this study was to examine the diagnostic performance of the first-trimester combined test for aneuploidies in unselected pregnancies from Rio de Janeiro and compare it with the examples available in the literature.
Methods
We investigated 3,639 patients submitted to aneuploidy screening from February 2009 to September 2015. The examination is composed of the Fetal Medicine Foundation risk evaluation based on nuchal translucency evaluation, mother’s age, presence of risk factors, presence of the nasal bone and Doppler of the ductus venous in addition to biochemical analysis of pregnancy-associated plasma protein A (PAPP-A) and beta-human chorionic gonadotropin (β-hCG) markers. The cut-off point for high risk for aneuploidies was defined as greater than 1:100, with intermediate risk defined between 1:100 and 1:1,000, and low risk defined as less than 1:1,000. The variable aneuploidy was considered as a result not only of trisomy of chromosome 21 but also trisomy of chromosomes 13 and 18.
Results
Excluding the losses, the results of 2,748 patients were analyzed. The firsttrimester combined test achieved 71.4% sensitivity with a 7.4% false-positive (FP) rate, specificity of 92.6%, positive predictive value (PPV) of 6.91% and negative predictive value (NPV) of 99.76%, when the cut-off point considered was greater than 1:1,000. Through a receiving operating characteristics (ROC) curve, the cut-off point that maximized the sensitivity and specificity for the diagnosis of aneuploidies was defined as 1:1,860. When we adjusted the false-positive (FP) rate to 5%, the detection rate for this analysis is 72.7%, with a cut-off point of 1:610.
Conclusion
The combined test of aneuploidy screening showed a detection rate inferior to those described in the literature for a higher FP rate.
Key-words Aneuploidybiomarkerschromosomal anomaliesNuchal translucency measurementPAPP-APregnancy complicationsscreen tests on maternal serumTrisomy 21β-HCGSee more -
Case Report06-01-2018
Febrile Neutropenia following Parvovirus B19 Infection and Cross Anti-Kell Reaction to E. Coli in Pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):372-376
Abstract
Case ReportFebrile Neutropenia following Parvovirus B19 Infection and Cross Anti-Kell Reaction to E. Coli in Pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):372-376
Views277Abstract
Parvovirus B19 has tropism for red line blood cells, causing immune hydrops during pregnancy. A positive anti-Kell Coombs reaction usually happens during pregnancy when there is production of antibodies that target Kell antigens, but cross reactions to other antigens may occur. A 24-year-old Gypsy primigravida, 0 Rhesus positive, presented with persistent isolated hyperthermia for 2 weeks and a positive indirect Coombs test result with anti-Kell antibodies at routine tests. She had a 19-week live fetus. The blood tests revealed bicytopenia with iron deficiency anemia, leucopoenia with neutropenia, and elevated C-reactive protein. She was medicated with imipenem, and had a slow clinical recovery. Blood, urine and sputum samples were taken to perform cultures and to exclude other systemic infections. Escherichia coli was isolated in the urine, which most probably caused a transient cross anti-Kell reaction. Haemophilus influenza in the sputum and seroconversion to parvovirus B19 was confirmed, causing unusual deficits in the white cells, culminating in febrile neutropenia. Despite the patient’s lack of compliance to the medical care, both maternal and fetal/neonatal outcomes were good. This a rare case report of 2 rare phenomena, a cross anti-Kell reaction to E. coli and parvovirus B19 infection with tropism for white cells causing febrile neutropenia, both events occurring simultaneously during pregnancy.
Key-words coombs testescherichia coliInfectionskell-active proteinsparvovirus antenatal infectionPregnancy complicationsSee more -
Case Report02-01-2018
Modified Pereira Suture as an Effective Option to Treat Postpartum Hemorrhage due to Uterine Atony
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(2):92-95
Abstract
Case ReportModified Pereira Suture as an Effective Option to Treat Postpartum Hemorrhage due to Uterine Atony
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(2):92-95
Views187See moreAbstract
Nowadays, postpartum hemorrhage is the major cause of maternal mortality and morbidity worldwide. Uterine atony is its main cause; thus, prophylactic measures, as well as medical and surgical fast approaches, have been developed to manage it. The uterine compression sutures are a possible treatment that preserves the uterus and, consequently, the fertility potential. Bearing that in mind, we report two cases of postpartum hemorrhage after caesarean section, successfully treated with a new modification of Pereira suture - longitudinal and transverse uterine sutures were applied after no response was registered to the first-line therapies. Both women recovered, and the postpartum evaluation revealed a normal uterus with an adequate blood supply, suggesting potential fertility, as described in the literature regarding this kind of therapeutic approach.
-
Original Article11-01-2017
Prevalence of Maternal Morbidity and Its Association with Socioeconomic Factors: A Population-based Survey of a City in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):587-595
Abstract
Original ArticlePrevalence of Maternal Morbidity and Its Association with Socioeconomic Factors: A Population-based Survey of a City in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):587-595
Views161See moreAbstract
Purpose
To identify the prevalence of maternal morbidity and its socioeconomic, demographic and health care associated factors in a city in Northeastern Brazil.
Methods
A cross-sectional and population-based study was conducted, with a design based on multi-stage complex sampling. A validated questionnaire was applied to 848 women aged between 15 and 49 years identified in 8,227 households from 60 census tracts of Natal, the capital of the state of Rio Grande do Norte (RN), Brazil. The main outcome measure was maternal morbidity. The Poisson regression analysis, with 5% significance, was used for the analysis of the associated factors.
Results
The prevalence of maternal morbidity was of 21.2%. A bivariate analysis showed the following variables associated with an increased number of obstetric complications: non-white race (prevalence ratio [PR] =1.23; 95% confidence interval [95%CI]: 1.04-1.46); lower socioeconomic status (PR = 1.33; 95%CI: 1.12-1.58); prenatal care performed in public services (PR = 1.42; 95%CI: 1.16-1.72): women that were not advised during prenatal care about where they should deliver (PR = 1.24; 95%CI: 1.05-1.46); delivery in public services (PR = 1.63; 95%CI: 1.30-2.03); need to search for more than one hospital for delivery (PR = 1.22; 95%CI: 1.03-1.45); and no companion at all times of delivery care (PR = 1.25, 95%CI: 1.05-1.48). The place where the delivery occurred (public or private) and the socioeconomic status remained significant in the final model.
Conclusion
Women in a worse socioeconomic situation and whose delivery was performed in public services had a higher prevalence of maternal morbidity. Such an association reinforces the need to strengthen public policies to tackle health inequalities through actions focusing on these determinants.
-
Case Report11-01-2017
Pregnancy in Non-Communicating Unicornuate Uterus: Diagnosis Difficulty and Outcomes – a Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):640-644
Abstract
Case ReportPregnancy in Non-Communicating Unicornuate Uterus: Diagnosis Difficulty and Outcomes – a Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):640-644
Views230See moreAbstract
Approximately 1 in every 76,000 pregnancies develops within a unicornuate uterus with a rudimentary horn.Müllerian uterus anomalies are often asymptomatic, thus, the diagnosis is a challenge, and it is usually made during the gestation or due to its complications, such as uterine rupture, pregnancy-induced hypertension, antepartum, postpartum bleeding and intrauterine growth restriction (IUGR). In order to avoid unnecessary cesarean sections and the risks they involve, the physicians should consider the several approaches and for how long it is feasible to perform labor induction in suspected cases of pregnancy in a unicornuate uterus with a rudimentary horn, despite the rarity of the anomaly. This report describes a case of a unicornuate uterus in which a pregnancy developed in the non-communicating rudimentary horn and the consequences of the delayed diagnosis.
-
Review Article09-01-2017
Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):496-512
Abstract
Review ArticlePreeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):496-512
Views650Abstract
The authors review hypertensive disease during pregnancy with an academic and practical view, and using the best evidence available. This disease, which is the most important clinical disease in Brazilian pregnant women, may have its incidence reduced with prevention through the use of calcium and aspirin in pregnant women at risk. Previously, it was a disease that presented with hypertension with proteinuria, but it has now been classified with new clinical parameters besides proteinuria. Morbidity and mortality should be reduced in a continental country such as Brazil using protocols for the early treatment of complications by calculating severe outcomes in preeclampsia. The early treatment of acute hypertension, use of magnesium sulfate and early hospitalization in cases of preeclampsia are concepts to pursue the reduction of our pregnant women’s mortality.
Key-words HELLP syndromeHigh risk pregnancyPreeclampsiapregnancy arterial hypertensionPregnancy complicationsSee more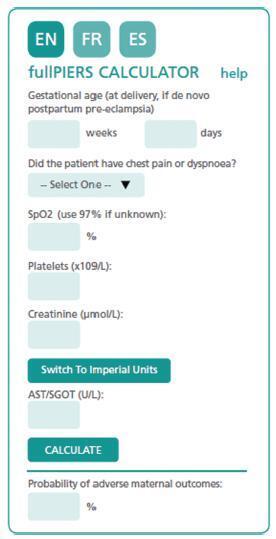
-
Original Article07-01-2017
Qualitative Determination of Human Chorionic Gonadotropin in Vaginal Washings for the Early Diagnosis of Premature Rupture of Fetal Membranes
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):317-321
Abstract
Original ArticleQualitative Determination of Human Chorionic Gonadotropin in Vaginal Washings for the Early Diagnosis of Premature Rupture of Fetal Membranes
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):317-321
Views233Abstract
Purpose
This study aimed to evaluate and validate the qualitative human chorionic gonadotropin β subunit (β-hCG) test of the vaginal fluid washings of pregnant women with premature rupture of fetal membranes (PROM).
Methods
Cross-sectional study of pregnant women between gestational weeks 24 and 39 who underwent consultations in one of our institutions. They were divided into two groups: group A (pregnant women clinically diagnosed with PROM) and group B (pregnant women without loss of amniotic liquid). The patients were subjected to a vaginal fluid washing with 3 mL of saline solution, which was aspirated subsequently with the same syringe. The solution was immediately sent to the laboratory to perform the vaginal β-hCG test with cut-off points of 10 mIU/mL (β-hCG-10) and/or 25 mIU/mL (β-hCG-25).
Results
The β-hCG-10 test of the vaginal secretion was performed in 128 cases. The chi-squared test with Yates’ correction showed a statistically significant difference between the 2 groups (p = 0.0225). The sensibility, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy parameters were 77.1%, 43.6%, 52.3%; 70.4%; and 58.6% respectively. The β-hCG-25 test of the vaginal washing was performed in 49 cases. The analysis by Fisher’s exact test showed a statistically significant difference between the groups (p = 0.0175). The sensibility, specificity, PPV, NPV, and accuracy parameters were 44.4%, 87.1%, 66.6%; 72.9%; and 71.4% respectively.
Conclusions
The β-hCG-25 test showed better accuracy for the diagnosis of PROM, and can corroborate the early diagnosis of PROM because it is a simple and quick exam.
Key-words DiagnosisHuman chorionic gonadotropinObstetricsPregnancy complicationspremature rupture of fetal membranesβ subunitSee more


