Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(6):260-266
DOI 10.1590/S0100-72032010000600002
PURPOSE: to describe the maternal complications due to therapeutic endoscopic procedures in fetal Medicine performed at an university center in Brazil. METHODS: retrospective observational study including patients treated from April 2007 to May 2010 who underwent laser ablation of placental vessels (LAPV) for severe twin-twin transfusion syndrome (TTTS); fetal tracheal occlusion (FETO) and endoscopic removal of tracheal balloon in cases of severe congenital diaphragmatic hernia (CDH); LAPV with or without bipolar coagulation of the umbilical cord in cases of twin reversed arterial perfusion (TRAP) sequence. The main variables described for each disease/type of surgery were maternal complications and neonatal survival (discharge from nursery). RESULTS: fifty-six patients underwent 70 procedures: Severe TTTS (34 patients; 34 surgeries); severe CDH (16 patients; 30 surgeries), and TRAP sequence (6 patients; 6 surgeries). Among 34 women who underwent LAPV for TTTS, two (2/34=5.9%) experienced amniotic fluid leakage to the peritoneal cavity and seven (7/34=20.6%) miscarried after the procedure. Survival of at least one twin was 64.7% (22/34). Among 30 interventions performed in cases of CDH, there was amniotic fluid leakage into the maternal peritoneal cavity in one patient (1/30=3.3%) and premature preterm rupture of membranes after three (3/30=30%) fetoscopies for removal of the tracheal balloon. Infant survival with discharge from nursery was 43.8% (7/16). Among six cases of TRAP sequence, there was bleeding into the peritoneal cavity after surgery in one patient (1/6=16.7%) and neonatal survival with discharge from nursery was 50% (3/6). CONCLUSIONS: in agreement with the available data in literature, at our center, the benefits related to therapeutic endoscopic interventions for TTTS, CDH and TRAP sequence seem to overcome the risks of maternal complications, which were rarely considered severe.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(2):94-98
DOI 10.1590/S0100-72032010000200008
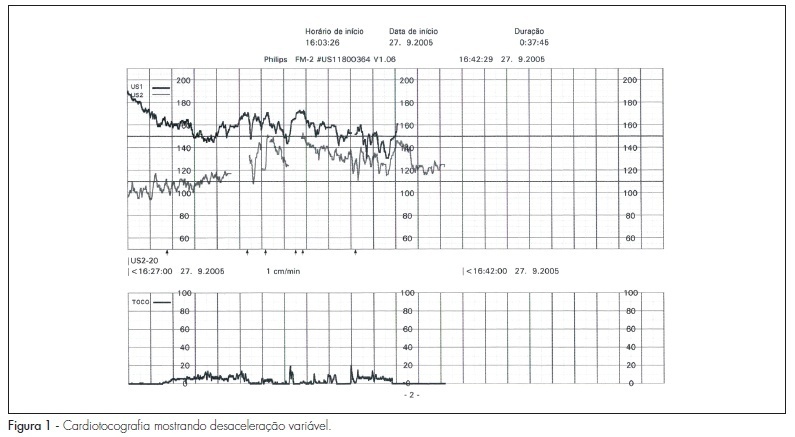
Monoamniotic twin pregnancies are very rare, but they are associated with high fetal morbidity and mortality. There is much controversy regarding the follow-up and obstetric procedures towards prenatal diagnosis of intertwined umbilical cords. In this article, we describe a case of monoamniotic pregnancy with diagnosis of intertwined umbilical cords, and we discuss aspects related to the follow-up and obstetric procedures through a brief literature review.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(12):604-608
DOI 10.1590/S0100-72032009001200005
PURPOSE: to evaluate the results of treatment to which patients with high grade intraepithelial cervical neoplasia (HSIL) are submitted, as well as their follow-up during pregnancy. METHODS: retrospective study based on the review of the medical report of 30 patients with diagnosis of high-grade squamous intraepithelial lesions (HSIL) during pregnancy and attended to at a tertiary hospital in southern Brazil from 1990 to 2002. Diagnosis was performed by colposcopy and biopsy, with repetition of the colposcopy during the pregnancy and after delivery. The diagnoses of regression and progression of lesions were evaluated. RESULTS: from 30 patients, 3 were excluded of the sample because the diagnosis of high-grade squamous intraepithelial lesions (HSIL) was not confirmed by the colposcopy with biopsia. Four patients were submitted to treatment during pregnancy, and one of them presented preterm delivery at the 32nd week. Twenty-three patients were submitted to expectant treatment, underwent a new colposcopy and biopsy, and then were submitted to conisation surgery at about the 11th week after the end of pregnancy. In 7.4% of the cases, there was lesion regression in the surgical specimen. CONCLUSIONS: all patients with diagnosis should be submitted to colposcopy and biopsy to exclude the possibility of invasive lesion. The expectant procedure for intraepithelial lesions is the most widely chosen and safe due to the possibility of regression in the postpartum period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(12):615-620
DOI 10.1590/S0100-72032009001200007
PURPOSES: to evaluate the influence of maternal hemoglobin (Hb) levels in the patterns of fetal heart rate (FHR) and in the fetal biophysical profile (FBP) in term gestations. METHODS: pregnant women with anemia (Hb<11.0 g/dL) were prospectively evaluated between the 36th and the 40th week of gestation, from January 2008 to March 2009. The Control Group was composed of term and healthy pregnant women, with normal values of hemoglobin (Hb>11,0 g/dL). Cases of anomalies or fetal growing restrictions were excluded. The FHR evaluation was performed by computerized cardiotocography (8002 System-Sonicaid), and by record analysis during 30 minutes of exam. The FBP was done in all the patients. Student's, χ2 and Fisher's exact tests were used, with 0.05 significance level. RESULTS: The average of maternal Hb in the group with anemia (n=18) was 9.4 g/dL (DP=1.4 g/dL), and in the control group, 12.4g/dL (DP=1.3 g/dL). There has been no significant mean differences between groups concerning the cardiotocography parameters, respectively: basal FHR(131.3 versus 133.7 bpm, p=0.5), FHR accelerations > 10b pm (7.9 versus 8.2, p=0.866), FHR accelerations > 15 bpm (5.2 versus. 5.4, p=0.9), episodes of high variation of the FHR (17.1 versus 15.5 min, p=0,5), episodes of variation of the FHR (4.4 versus 3.6 min, p=06), and short term variation (10.5 versus 10.9 ms, p=0.5). In both groups, all patients presented normal FBP. CONCLUSIONS: this study suggests that light or moderate maternal anemia, without other maternal or fetal comorbidity, is not associated with abnormalities in the parameters of fetal biophysical profile and of the FHR analyzed by computerized cardiotocography.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(9):440-446
DOI 10.1590/S0100-72032009000900004
PURPOSE: to verify the occurrence ratio of pica in pregnant women and its impact on the mother and newborn health. METHODS: prospective study with 227 adult pregnant women and their newborns treated at the Maternity School of Universidade Federal do Rio de Janeiro, between 2005 and 2006. Pica has been considered as the ingestion of inedible substances or atypical food combinations. The data was collected was done by medical chart review and interview. RESULTS: Pica was referred to by 14.4% of the women, 42.1% of whom practiced it daily. The onset occurred in the second gestational trimester in 46.7% of the cases, and, in the third trimester, in 30% of them. Among the alleged reasons, 65% of the women were unable to give them, 15% declared relief of nausea and heartburn and 10% reported reduced stress and anxiety. The practice in the previous gestation/puerperium was referred to by 15% of the women. Pica was not associated with the maternal anthropometric condition, the skin color, the marital status, the maternal schooling and the presence of parasitosis. There was no difference between the average of the total family income and the number of gestations for the women who did or did not have pica. Pica was associated with gestational anemia (p<0.009) and gestational intercurrences (OR=3.5; CI95%=1.6-7.9). As for the baby, pica did not interfere in the health parameters at birth: weight, gestational age and intercurrences. CONCLUSIONS: pica must be investigated at prenatal assistance and recognized as a risk factor for the mother's health.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(7):326-334
DOI 10.1590/S0100-72032009000700002
PURPOSE: to analyze the association of the mother's age, the perinatal outcome and the delivery route. METHODS: information about all the patients attended at the Service of Obstetrics and Gynecology of a tertiary university hospital in Maranhão, from July to December 2006, was analyzed. Patients have been allocated in three groups: adolescents (10 to 19 years old), adults (20 to 34 years old), and aged women (>35 years old). Variables studied were: skin color, schooling, marital status, family income, parity, number of appointments during pre-natal care, gestational age at the onset of pre-natal care, delivery route, Apgar index at the fifth minute and birth weight. Data were processed by the Epi-info program, version 3.4.1, and the association among the variables was analyzed by the Odds Ratio (OR) or the cross product ratio, with confidence intervals (CI) of 95%. The significance level was 0.05. RESULTS: among 2,196 patients, 25% of deliveries occurred in adolescents, 69% in adults and 6% in aged women. Among the adolescents, there was higher risk of prematurity (OR=1.46; CI95%=1.14-1.88), and low birth weight (OR=1.47; CI95%=1.13- 1.90), higher incidence of normal delivery as compared to the other groups (65.2%), besides the association with late onset of pre-natal care (OR=1.86; CI95%=1.43-2.43), lower number of appointments (OR=2.03; CI95%=1.57-2.63), and use of abortive procedures at the onset of gestation (OR=2.34; CI95%=1.38-3.98). Among aged women, there was strong association with diabetes mellitus (OR=9.00; CI95%=3.18-25.19), pre-eclampsia (OR=4.38; CI95%=3.02-6.34), premature membrane rupture (OR=5.81; CI95%=3.08-10.89), besides a higher chance of presenting Apgar index lower than seven at the fifth minute (OR=2.90; CI95%=1.37-6.01), and higher ratio of cesarean section (60.3%). CONCLUSIONS: pregnancy in adolescence is associated to late onset of pre-natal care and few appointments along it, use of abortive procedures at the onset of gestation, low schooling, no mates, low birth weight, prematurity, and lower incidence of cephalo pelvic disproportion and pre-eclampsia. Among aged pregnant women, there was association with diabetes, pre-eclampsia, premature membrane rupture, Apgar index lower than seven at the fifth minute and higher ratio of cesarean section.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(8):397-403
DOI 10.1590/S0100-72032009000800005
PURPOSE: to indentify the prevalence and risk factors of maternal colonization by group B streptococcus (GBS) in pregnant women with premature labor (PL) and/or premature membrane rupture (PMR). METHODS: two anal and two vaginal swabs were collected from 203 pregnant women with diagnosis of PL or PMR assisted at the practice along one year. Pregnant women with imminent labor at admission were excluded. One swab of each source was placed in a transfer milieu and sent for culture in blood-agar plates; the two remaining swabs were incubated for 24 hours in Todd-Hewitt milieu for further sowing in blood-agar plates. Risk factors were analyzed by the chi-square test, Student's t-test (p-value set at 0.05 and 95% confidence interval) and logistic regression. The following variables were analyzed: age, race, parity and mother schooling; culture results by source and type of culture; admission diagnosis; gestational age at admission; asymptomatic bacteriuria; gestational age at delivery; type of delivery; neonatal GBS colonization rate and immediate neonatal condition. RESULTS: prevalence of maternal GBS colonization was 27.6% (56 cases). The colonization rates according to gestational complications were 30% for PMR, 25.2% for PL and 17.8% for PL + PMR. Univariate analysis has shown that the variables Caucasian race, low level of schooling and bacteriuria were associated with higher colonization rates. Multivariate analysis showed that the presence of urinary infection was the only variable associated with maternal colonization. The GBS detection rate was significantly higher with the use of a selective milieu and collection from both anal and vaginal sources. The neonatal colonization rate was 3.1%. Two cases of early sepsis by GBS occurred in the sample, with prevalence of 10.8 cases per one thousand live births and 50% mortality rate. CONCLUSION: the studied sample showed high maternal colonization rates by Streptococcus agalactiae. To increase GBS detection rate, it is necessary to use a selective culture milieu and to combine anal-rectal and vaginal cultures. There was a high incidence of early neonatal sepsis.