-
Original Article
Negative Correlation between Placental Growth Factor and Endocan-1 in Women with Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):593-598
10-01-2018
Summary
Original ArticleNegative Correlation between Placental Growth Factor and Endocan-1 in Women with Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):593-598
10-01-2018Views129See moreAbstract
Objective
To analyze endocan-1, a biomarker of vascular endothelial related pathologies, and the placental growth factor (PlGF), an angiogenic factor and a placental dysfunction marker in patients with preeclampsia (PE).
Methods
Case-control study conducted at Hospital São Lucas, in the city of Porto Alegre, Brazil. Endocan-1 and PlGF levels were quantified in the maternal plasma using the MagPlexTH-C microsphere system (MAGPIX System, Luminex, Austin, Texas, US) and evaluated through analysis of covariance (ANCOVA) and adjusted by body mass index (BMI), gestational age and maternal age. To estimate the difference between the groups, the mean ratio (MR) and the 95% confidence interval (95%CI) were calculated. The Pearson correlation test was used to establish any association between endocan-1 and PlGF levels. The null hypothesis was rejected when p < 0.05.
Results
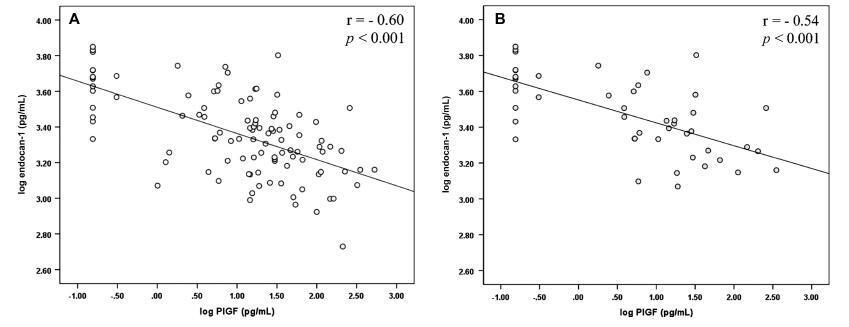
The group of patients was composed by normotensive (n = 67) patients and patients with PE (n = 50). A negative correlation between endocan-1 and the PlGF was noted in the entire normotensive group (linear correlation coefficient [r] = -0.605; p < 0.001), as well as in the PE group (r = -0.545; p < 0.001).
Conclusion
Endocan-1 levels are increased in patients with PE, and are inversely correlated with PlGF levels. We suggest that it is important to analyze angiogenic and proinflammatory molecules concomitantly in women with PE to better understand the pathophysiology of the disease. Both molecules are strong candidates for PE biomarkers, and future studies will examine any mechanisms connecting these factors in PE.
-
Review Article
Uterine Artery Doppler in Screening for Preeclampsia and Fetal Growth Restriction
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):287-293
05-01-2018
Summary
Review ArticleUterine Artery Doppler in Screening for Preeclampsia and Fetal Growth Restriction
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):287-293
05-01-2018Views289See moreAbstract
Objective
To perform a comprehensive review of the current evidence on the role of uterine artery Doppler, isolated or in combination with other markers, in screening for preeclampsia (PE) and fetal growth restriction (FGR) in the general population. The review included recently published large cohort studies and randomized trials.
Methods
A search of the literature was conducted usingMedline, PubMed, MeSH and ScienceDirect. Combinations of the search terms “preeclampsia,” “screening,” “prediction,” “Doppler,” “Doppler velocimetry,” “fetal growth restriction,” “small for gestational age” and “uterine artery” were used. Articles in English (excluding reviews) reporting the use of uterine artery Doppler in screening for PE and FGR were included.
Results
Thirty articles were included. As a single predictor, uterine artery Doppler detects less than 50% of the cases of PE and no more than 40% of the pregnancies affected by FGR. Logistic regression-based models that allow calculation of individual risk based on the combination of multiple markers, in turn, is able to detect ~ 75% of the cases of preterm PE and 55% of the pregnancies resulting in small for gestational age infants.
Conclusion
The use of uterine artery Doppler as a single predictive test for PE and FGR has poor accuracy. However, its combined use in predictive models is promising, being more accurate in detecting preterm PE than FGR.
-
Systematic Review
Preterm Preeclampsia and Timing of Delivery: A Systematic Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):622-631
11-01-2017
Summary
Systematic ReviewPreterm Preeclampsia and Timing of Delivery: A Systematic Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):622-631
11-01-2017Views100See moreAbstract
Introduction
Preeclampsia, a multifactorial disease with pathophysiology not yet fully understood, is a major cause of maternal and perinatal morbidity and mortality, especially when preterm. The diagnosis is performed when there is an association between arterial hypertension and proteinuria or evidence of severity. There are unanswered questions in the literature considering the timing of delivery once preterm preeclampsia has been diagnosed, given the risk of developingmaternal complications versus the risk of adverse perinatal outcomes associated with prematurity. The objective of this systematic review is to determine the best timing of delivery for women diagnosed with preeclampsia before 37 weeks of gestation.
Methods
Systematic literature review, performed in the PubMed database, using the terms preeclampsia, parturition and timing of delivery to look for studies conducted between 2014 and 2017. Studies that compared the maternal and perinatal outcomes of women who underwent immediate delivery or delayed delivery, in the absence of evidence of severe preeclampsia, were selected.
Results
A total of 629 studies were initially retrieved. After reading the titles, 78 were selected, and their abstracts, evaluated; 16 were then evaluated in full and, in the end, 6 studies (2 randomized clinical trials and 4 observational studies) met the inclusion criteria. The results were presented according to gestational age range (< 34 weeks and between 34 and 37 weeks) and by maternal and perinatal outcomes, according to the timing of delivery, considering immediate delivery or expectant management. Before 34 weeks, thematernal outcomeswere similar, but the perinatal outcomes were significantly worse when immediate delivery occurred. Between 34 and 37 weeks, the progression to severe maternal disease was slightly higher among women undergoing expectant management, however, with better perinatal outcomes.
Conclusions
When there is no evidence of severe preeclampsia or impaired fetal wellbeing, especially before 34 weeks, the pregnancy should be carefully surveilled, and the delivery, postponed, aiming at improving the perinatal outcomes. Between 34 and 37 weeks, the decision on the timing of delivery should be shared with the pregnant woman and her family, after providing information regarding the risks of adverse outcomes associated with preeclampsia and prematurity.
-
Review Article
Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):496-512
09-01-2017
Summary
Review ArticlePreeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):496-512
09-01-2017Views404Abstract
The authors review hypertensive disease during pregnancy with an academic and practical view, and using the best evidence available. This disease, which is the most important clinical disease in Brazilian pregnant women, may have its incidence reduced with prevention through the use of calcium and aspirin in pregnant women at risk. Previously, it was a disease that presented with hypertension with proteinuria, but it has now been classified with new clinical parameters besides proteinuria. Morbidity and mortality should be reduced in a continental country such as Brazil using protocols for the early treatment of complications by calculating severe outcomes in preeclampsia. The early treatment of acute hypertension, use of magnesium sulfate and early hospitalization in cases of preeclampsia are concepts to pursue the reduction of our pregnant women’s mortality.
Key-words HELLP syndromeHigh risk pregnancyPreeclampsiapregnancy arterial hypertensionPregnancy complicationsSee more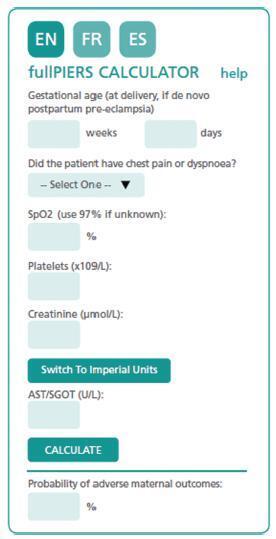
-
Original Article
High Blood Pressure during Pregnancy is not a Protective Factor for Preterm Infants with Very Low Birth Weight. A Case-Control Study
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):155-161
04-01-2017
Summary
Original ArticleHigh Blood Pressure during Pregnancy is not a Protective Factor for Preterm Infants with Very Low Birth Weight. A Case-Control Study
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):155-161
04-01-2017Views165See moreAbstract
Objective
To evaluate whether the presence of maternal blood pressure reduces the risks of morbidity, perinatal mortality and morbidity at 24 months of age in very low birth weight infants (VLBWIs) compared with a control group.
Methods
A retrospective, observational, case-control study. Total 49 VLBWIs were allocated to the study group, called the maternal arterial hypertension group (AHG), and matched with 44 in the control group (CG). The infants were assessed during hospitalization and at 12 and 24 months corrected age at a specialized clinic. For the assessment of growth, the World Health Organization (WHO) Anthro software (Geneva, 2006) was used, and for the psychomotor assessment, the Denver II test was used.
Results
In relation to the antenatal variables, the infants of the AHG had more centralized circulation assessed by Doppler, received more corticosteroids and magnesium sulfate, and were born by cesarean section more frequently. In terms of the postnatal and in-hospital outcomes, the AHG had a higher gestational age at birth (30.7 versus 29.6 weeks) and a lower frequency of 5-minute Apgar scores of less than 7 (26.5% versus 52.3%). The CG had a higher rate of pulmonary dysplasia (30.2% versus 8.3%). There were no differences in terms of hospital mortality, complications, somatic growth and functional problems at 24 months of corrected age.
Conclusion
The presence of maternal hypertension, especially preeclampsia, was not a protective factor against morbidity, mortality and evolution in VLBWIs aged up to 24 months. Therefore, the clinical practice should be focused on prolonging the pregnancy for as long as possible in these conditions as well.
-
Review Article
Impacts of Preeclampsia on the Brain of the Offspring
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):416-422
08-01-2016
Summary
Review ArticleImpacts of Preeclampsia on the Brain of the Offspring
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):416-422
08-01-2016Views151See moreAbstract
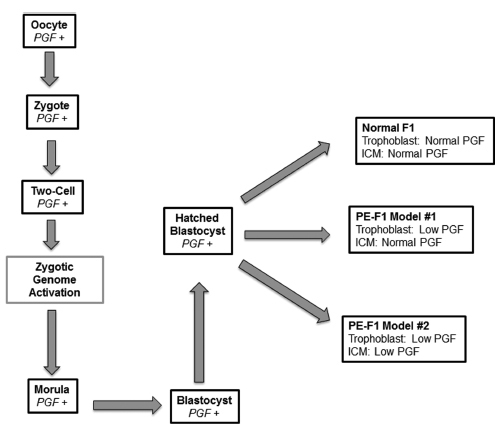
Preeclampsia (PE) is a significant gestational disorder that causes complications in 3- 5% of all human pregnancies. Apart from the immediate risks and complications for mother and fetus, both additionally carry elevated lifelong risks for specific complications. Offspring of PE pregnancies (PE-F1) have higher risks for hypertension, stroke and cognitive impairment compared with well-matched offspring (F1) fromuncomplicated pregnancies. Prior to the clinical onset of PE, placental angiokines secreted into the maternal plasma are deviated. In many PE patients this includes deficits in placental growth factor (PGF). Our laboratory found that mice genetically-deleted for PGF (PGF - / -) have altered cerebrovascular and brain neurological development detectable from midgestation to adulthood. We hypothesized that the PGF deficits seen in human PE, deviate fetal cerebrovascular and neurological development in a manner that impairs cognitive functions and elevates stroke risk. Here we summarize the initial analytical outcomes from a pilot study of 8-10 year old male and female PE-F1s and matched controls. Our studies were the first to report magnetic resonance imaging (MRI), magnetic resonance angiography (MRA) and functional brain region assessment by eyemovement control and clinical psychometric testing in PE-F1s. Further studies in larger cohorts are essential to define whether there are image-based biomarkers that describe unique anatomical features in PE-F1 brains.
-
Revisão
Preeclampsia: oxidative stress, inflammation and endothelial dysfunction
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(12):609-616
04-13-2010
Summary
RevisãoPreeclampsia: oxidative stress, inflammation and endothelial dysfunction
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(12):609-616
04-13-2010DOI 10.1590/S0100-72032010001200008
Views61See morePreeclampsia is a systemic syndrome characterized by inflammatory and antiangiogenic states. The pathogenesis of preeclampsia involves deficient trophoblast invasion that is responsible for altered uterine blood flow and placental oxidative stress. The damaged placenta produces higher concentrations of sFlt-1, a soluble receptor for VEGF and PlGF that is released in the maternal circulation and is involved in endothelial dysfunction. Actually, all processes involved in inflammation, endothelial dysfunction and oxidative stress are strongly correlated and act in a synergistic way. Recent data have shown that an increase in serum concentrations of sFlt-1 initiates 5 to 6 weeks before the clinical manifestations of preeclampsia and these alterations correlate with a decrease in serum concentrations of PlGF. Therefore, both sFlt-1 and PlGF have been suggested to be useful for an early-diagnosis of preeclampsia. The knowledge about the role of antiangiogenic factors in the pathogenesis of preeclampsia has raised the possibility of a therapy involving these factors.In this article we revisited the pathogenesis of preeclampsia addressing its antiangiogenic and inflammatory states.In conclusion, we correlated these alterations with the higher risk for cardiovascular diseases presented by these women in future life.
-
Artigos Originais
Early-onset preeclampsia: is it a better classification for maternal and perinatal outcomes?
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(12):584-590
04-13-2010
Summary
Artigos OriginaisEarly-onset preeclampsia: is it a better classification for maternal and perinatal outcomes?
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(12):584-590
04-13-2010DOI 10.1590/S0100-72032010001200004
Views78See morePURPOSE: to evaluate the differences between the maternal and perinatal outcomes of pregnancies complicated by preeclampsia, according to the classification as the severe/mild form, and the early/late onset form. METHODS: a retrospective study with 211 pregnancies complicated by preeclampsia, assessed at a university reference center from 2000 to 2010. The diagnosis and disease severity were based on the values of blood pressure, proteinuria, and clinical and laboratory findings. The pregnant's age, skin color, parity, blood pressure, urine protein semiquantitative values, presence of bilateral notch in the uterine artery dopplervelocimetry and birth conditions were compared between patients with mild and severe disease, as well as between those of early/late onset. The disease was considered to be of early onset when diagnosed at less than 34 weeks of gestational age. RESULTS: most patients had the severe form of preeclampsia (82.8%), and the onset of the condition was early in 50.7%. Blood pressure values (133.6±14.8 versus 115.4 mmHg, p=0.0004 and 132.2±16.5 versus 125.7 mmHg, p=0.0004) and semiquantitative proteinuria (p=0.0003 and p=0.0005) were higher in the early and severe forms compared to mild and late forms. Infant birth weight (1,435.4±521.6 versus 2,710±605.0 g, 1,923.7±807.9 versus 2,415.0±925.0 g, p<0.0001 for both) and Apgar score (p=0.01 for both) were smaller for severe and early preeclampsia compared to mild and late preeclampsia. On the other hand, the presence of a bilateral notch in the uterine arteries was linked to the forms of early onset (69.2 versus 47.9%, p=0.02), whereas fetal growth restriction was more frequent in the severe forms of preeclampsia (30 versus 4.4%, p=0.008). CONCLUSION: the preeclampsia classification based on maternal clinical parameters better reflected the conditions of fetal nutrition, while the early onset of the condition was associated with placental vasculopathy detected by dopplervelocimetry.


