-
Original Article06-09-2025
Impact of the Zero Maternal Death by Hemorrhage Strategy on health professionals’ self-perceived knowledge in managing postpartum hemorrhage
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo25
Abstract
Original ArticleImpact of the Zero Maternal Death by Hemorrhage Strategy on health professionals’ self-perceived knowledge in managing postpartum hemorrhage
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo25
Views125Abstract
Objective:
This study aimed to evaluate the results of the Obstetric Hemorrhage Prevention and Management Course – Zero Maternal Death by Hemorrhage Strategy (0MMxH) among healthcare professionals before and after participation.
Methods:
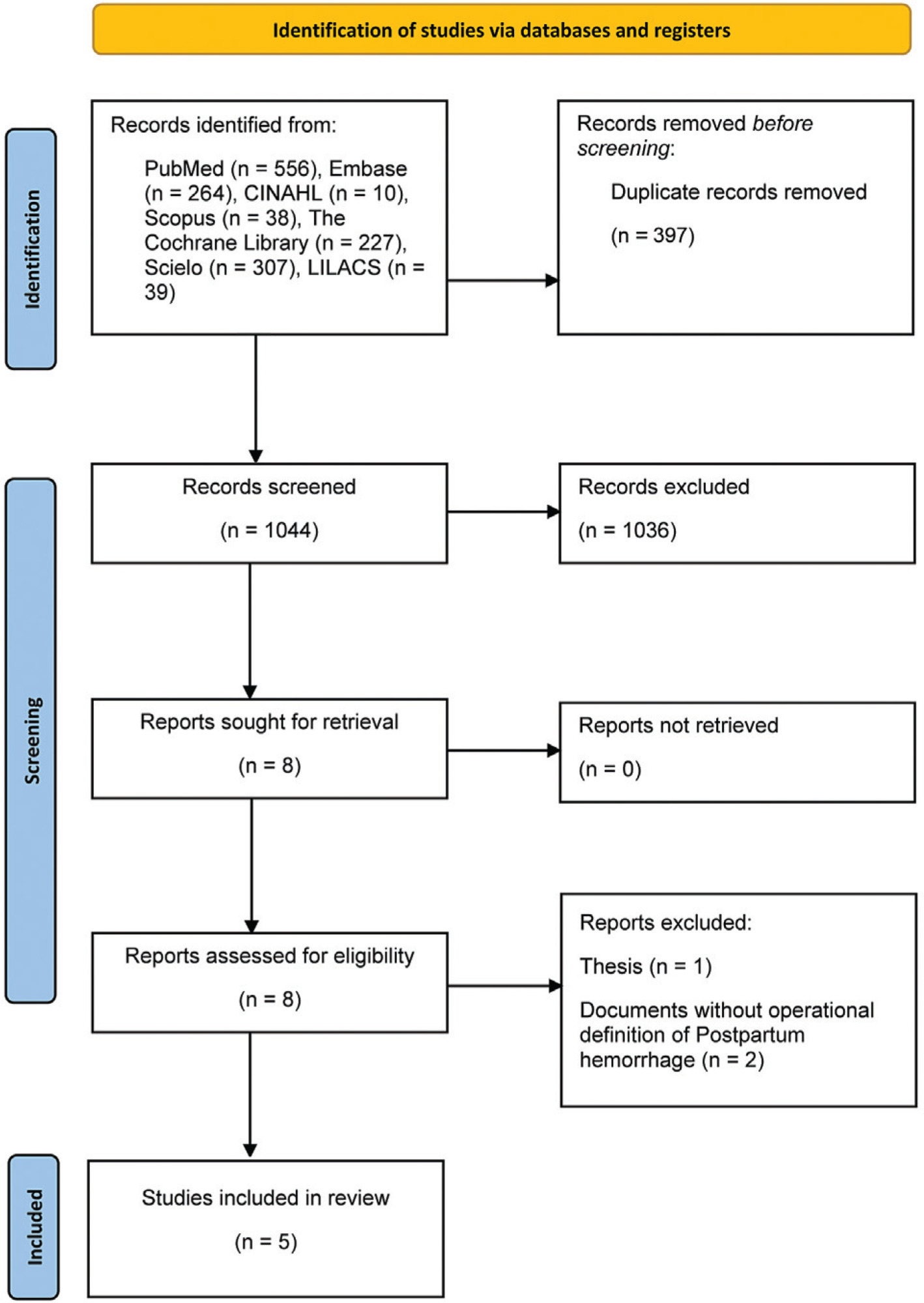
A quasi-experimental design was employed, assessing the educational intervention in a convenience sample of healthcare professionals who had participated in the 0MMxH at least one year prior. Participants completed a retrospective pre-post questionnaire sent via email, focusing on self-perceived knowledge levels and the adoption of best practices in postpartum hemorrhage (PPH) management.
Results:
Out of 129 professionals who completed the 0MMxH training, 85 (65.9%) responded to the questionnaire. The percentages of respondents reporting no or low knowledge before and after the course were: shock index (52.8% to 0%, before and after, respectively), blood loss estimation (35.2% to 1.1%), care sequence for PPH (44.6% to 0%), rational use of crystalloids (37.5% to 1.1%), non-pneumatic anti-shock garment (83.5% to 3.4%), and damage control surgery (74.1% to 8.1%). These results indicate a significant improvement in self-perceived knowledge. After the course, the highest adoption rates of best practices were for shock index (83.5%), blood loss estimation (67.1%), and use of warm crystalloids (58.8%). However, gaps remained regarding non-pharmacological interventions for PPH management.
Conclusion:
Participants reported improved knowledge on most topics covered by the 0MMxH. The program was recognized as a crucial factor in adopting effective PPH management practices, underscoring the importance of training in enhancing obstetric care.
Key-words Health strategiesHealthcare professionalsMaternal mortalityMedical EducationPostpartum hemorrhageSee more -
Original Article09-18-2024
Multidisciplinary team training in postpartum hemorrhage: impact on the use of blood products
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo67
Abstract
Original ArticleMultidisciplinary team training in postpartum hemorrhage: impact on the use of blood products
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo67
Views341See moreAbstract
Objective
Compare the number of puerperal women submitted to blood transfusion before and after the implementation of a care protocol for postpartum hemorrhage (PPH) with multidisciplinary team training.
Methods
Cross-sectional study in a university hospital, analyzing births from 2015 to 2019, compared the use of blood products before and after the adoption of a PPH protocol with multidisciplinary training.
Results
Between 2015 and 2019, there were 17,731 births, with 299 (1.7%) postpartum women receiving blood products and 278 postpartum women were considered for this analysis, 128 (0.7%) at Time 1 and 150 (0.8%) at Time 2. After the multiprofessional team training (T2), there was a difference in the complete use of the PPH protocol (use of oxytocin, misoprostol and tranexamic acid) (T1 = 5.1% x T2 = 49.5%, p≤0.0001). An individual categorized analysis revealed that, in the T2 period, there was lower use of blood component units per patient compared to T1 (Mann-Whitney, p=0.006). It should be noted that at T1 and T2, 54% and 24% respectively received two units of blood products. It is important to highlight that after the multidisciplinary team training for the PPH protocol, the goal of zero maternal death due to hemorrhage was reached.
Conclusion
The adoption of a specific protocol for PPH, combined with the training of a multidisciplinary team, had an impact on the ability to identify women at high risk of hemorrhage, resulting in a decrease in the use of blood components.
-
Original Article06-27-2024
Risk factors for postpartum hemorrhage according to the Robson classification in a low-risk maternity hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo53
Abstract
Original ArticleRisk factors for postpartum hemorrhage according to the Robson classification in a low-risk maternity hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo53
Views288Abstract
Objective
To evaluate the risk factors for postpartum hemorrhage (PPH) according to the Robson Classification in a low-risk maternity hospital.
Methods
We conducted retrospective cohort study by analyzing the medical records of pregnant women attended in a low-risk maternity hospital, during from November 2019 to November 2021. Variables analyzed were: maternal age, type of delivery, birth weight, parity, Robson Classification, and causes of PPH. We compared the occurrence of PPH between pregnant women with spontaneous (Groups 1 and 3) and with induction of labor (2a and 4a). Chi-square and Student t-tests were performed. Variables were compared using binary logistic regression.
Results
There were 11,935 deliveries during the study period. According to Robson’s Classification, 48.2% were classified as 1 and 3 (Group I: 5,750/11,935) and 26.1% as 2a and 4a (Group II: 3,124/11,935). Group II had higher prevalence of PPH than Group I (3.5 vs. 2.7%, p=0.028). Labor induction increased the occurrence of PPH by 18.8% (RR: 1.188, 95% CI: 1.02-1.36, p=0.030). Model including forceps delivery [x2(3)=10.6, OR: 7.26, 95%CI: 3.32-15.84, R2 Nagelkerke: 0.011, p<0.001] and birth weight [x2(4)=59.0, OR: 1.001, 95%CI:1.001-1.001, R2 Nagelkerke: 0.033, p<0.001] was the best for predicting PPH in patients classified as Robson 1, 3, 2a, and 4a. Birth weight was poor predictor of PPH (area under ROC curve: 0.612, p<0.001, 95%CI: 0.572-0.653).
Conclusion
Robson Classification 2a and 4a showed the highest rates of postpartum hemorrhage. The model including forceps delivery and birth weight was the best predictor for postpartum hemorrhage in Robson Classification 1, 3, 2a, and 4a.
Key-words Hospitals, maternityPostpartum hemorrhagePostpartum periodPregnancyRisk factorsrobson classificationSee more -
Original Article06-27-2024
The profile of patients with postpartum hemorrhage admitted to the obstetric intensive care: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo47
Abstract
Original ArticleThe profile of patients with postpartum hemorrhage admitted to the obstetric intensive care: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo47
Views315See moreAbstract
Objective
In Brazil, postpartum hemorrhage (PPH) is a major cause of maternal morbidity and mortality. Data on the profile of women and risk factors associated with PPH are sparse. This study aimed to describe the profile and management of patients with PPH, and the association of risk factors for PPH with severe maternal outcomes (SMO).
Methods
A cross-sectional study was conducted in Instituto de Medicina Integral Prof. Fernando Figueira (IMIP) obstetric intensive care unit (ICU) between January 2012 and March 2020, including patients who gave birth at the hospital and that were admitted with PPH to the ICU.
Results
The study included 358 patients, of whom 245 (68.4%) delivered in the IMIP maternity, and 113 (31.6%) in other maternity. The mean age of the patients was 26.7 years, with up to eight years of education (46.1%) and a mean of six prenatal care. Uterine atony (72.9%) was the most common cause, 1.6% estimated blood loss, 2% calculated shock index (SI), 63.9% of patients received hemotransfusion, and 27% underwent hysterectomy. 136 cases of SMO were identified, 35.5% were classified as maternal near miss and 3.0% maternal deaths. Multiparity was associated with SMO as an antepartum risk factor (RR=1.83, 95% CI1.42-2.36). Regarding intrapartum risk factors, abruptio placentae abruption was associated with SMO (RR=2.2 95% CI1.75-2.81). Among those who had hypertension (49.6%) there was a lower risk of developing SMO.
Conclusion
The principal factors associated with poor maternal outcome were being multiparous and placental abruption.
-
Original Article00-00-2024
Postpartum hemorrhage in electronic health records: risk factors at admission and in-hospital occurrence
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo14
Abstract
Original ArticlePostpartum hemorrhage in electronic health records: risk factors at admission and in-hospital occurrence
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo14
Views511Abstract
Objective:
Postpartum hemorrhage (PPH) is the leading cause of maternal death globally. Therefore, prevention strategies have been created. The study aimed to evaluate the occurrence of PPH and its risk factors after implementing a risk stratification at admission in a teaching hospital.
Methods:
A retrospective cohort involving a database of SISMATER® electronic medical record. Classification in low, medium, or high risk for PPH was performed through data filled out by the obstetrician-assistant. PPH frequency was calculated, compared among these groups and associated with the risk factors.
Results:
The prevalence of PPH was 6.8%, 131 among 1,936 women. Sixty-eight (51.9%) of them occurred in the high-risk group, 30 (22.9%) in the medium-risk and 33 (25.2%) in the low-risk group. The adjusted-odds ratio (OR) for PPH were analyzed using a confidence interval (95% CI) and was significantly higher in who presented multiple pregnancy (OR 2.88, 95% CI 1.28 to 6.49), active bleeding on admission (OR 6.12, 95% CI 1.20 to 4.65), non-cephalic presentation (OR 2.36, 95% CI 1.20 to 4.65), retained placenta (OR 9.39, 95% CI 2.90 to 30.46) and placental abruption (OR 6.95, 95% CI 2.06 to 23.48). Vaginal delivery figured out as a protective factor (OR 0.58, 95% CI 0.34 to 0.98).
Conclusion:
Prediction of PPH is still a challenge since its unpredictable factor arrangements. The fact that the analysis did not demonstrate a relationship between risk category and frequency of PPH could be attributable to the efficacy of the strategy: Women classified as "high-risk" received adequate medical care, consequently.
Key-words Electronic health recordsMaternal mortalityPostpartum hemorrhagePuerperal disordersRisk factorsSee more -
Original Article11-29-2021
Understanding How Health Providers Identify Women with Postpartum Hemorrhage: A Qualitative Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):648-654
Abstract
Original ArticleUnderstanding How Health Providers Identify Women with Postpartum Hemorrhage: A Qualitative Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):648-654
Views238See moreAbstract
Objective
To identify how health providers recognize postpartum hemorrhage early and the difficulties involved in it.
Methods
An exploratory, descriptive study using a qualitative approach through a semi-structured interview technique. In total, 27 health professionals (nursing tech nicians, nurses, medical residents in Gynecology and Obstetrics, hired medical doctors, and medicine professors) working in a tertiary-level hospital of reference in women’s health care in the State of São Paulo, Brazil, participated in the study through an invitation. After they accepted the invitation, they signed the free and informed consent form. All interviews were recorded and transcribed, and a thematic analysis was conducted. We found three analysis categories: a) perception of the severity: “there is something wrong with the women”; b) difficulties in the early diagnosis of postpartum hemorrhage; and c) the process to improve obstetrical care.
Results
Caregivers believe teamwork and communication should be improved. Besides the visual estimation of blood loss, the nursing team is attentive to behavioral symptoms like irritability, while the medical staff follow protocols and look for objective signs, such as altered vital signs.
Conclusion
Besides the objective evaluations, the subjective perceptions of the providers are involved in the clinical judgement regarding the diagnosis of postpartum hemorrhage, and this should be included in a broader diagnosis strategy.
-
Original Article11-29-2021
Clinical Experience Over 15 Years with the B-Lynch Compression Suture Technique in the Management of Postpartum Hemorrhage
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):655-661
Abstract
Original ArticleClinical Experience Over 15 Years with the B-Lynch Compression Suture Technique in the Management of Postpartum Hemorrhage
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):655-661
Views258See moreAbstract
Objective
To describe the clinical experience with the B-Lynch technique in the management of postpartum hemorrhage as well as the factors related to the indication of the technique and to present the success rates of the application of the B-Lynch technique.
Methods
Observational, retrospective, cross-sectional, and analytical study. Patient data was obtained through the study of medical records. The study population comprised of patients who underwent hemostatic suture using the B-Lynch technique, including 104 patients within the period from January 1, 2005, to December 31, 2019.
Results
Of the total of 104 patients, 82.7% did not present any complications. Blood transfusion and intensive care unit admission were the most prevalent complications, with 13.5% and 15.4%, respectively. Only 1% of the patients had puerperal and surgical site infections. The factors most related to the application of the technique were the presence of previous cesarean section (30.8%), use of oxytocin (16.3%), and pre-eclampsia (11.6%). Puerperal hysterectomy was performed in 4.8% of the patients due to failure of the method.
Conclusion
The clinical experience with the B-Lynch technique was satisfactory since it presented few complications, with excellent results in hemorrhagic control. Previous cesarean section, the use of oxytocin, and preeclampsia stood out as factors related to the indication of the application of the technique, and the success rate in controlling postpartum hemorrhage was 95.2%.