-
Original Article
Anal High-risk HPV and Liquid-based Cytology of Immunocompetent Brazilian Women with Genital High-risk HPV
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):280-286
02-09-2022
Summary
Original ArticleAnal High-risk HPV and Liquid-based Cytology of Immunocompetent Brazilian Women with Genital High-risk HPV
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):280-286
02-09-2022Views109See moreAbstract
Objective
The purpose of this study was to compare the frequency of the occurrence of high-risk human papillomavirus (HPV) and abnormal anal cytology in immunocompetent women with and without HPV-induced genital lesions.
Methods
This analytical cross-sectional, observational study was conducted between July 2017 and December 2018 in a specialized outpatient clinic of a tertiary hospital in Fortaleza, CE. Fifty-seven immunocompetent women with and without genital intraepithelial lesions were assessed; they were divided into two groups: group 1 was comprised of women with HPV-associated genital lesions (n=26), and group 2 was comprised of those without HPV-associated genital lesions (n=31). Samples for liquidbased cytology and high-risk DNA-HPV polymerase chain reaction real-time tests were collected from the cervix and anus. All cases were evaluated using high-resolution anoscopy; biopsies were performed when required. The Fisher exact and chi-squared tests were applied for consolidated data in the contingency table, and the Student ttest and Mann-Whitney U-test for independent variables.
Results
Anal high-risk HPV infections were more frequent in group 1 (odds ratio [OR], 4.95; 95% confidence interval [CI], 1.34-18.3; p=0.012), along with concomitant highrisk HPV infections in the uterine cervix and the anus (OR 18.8; 95% CI, 2.20-160; p<0.001). The incidence of high-risk cervical HPV infection was associated with highrisk anal HPV infection (OR, 4.95; 95% CI, 1.34-18.3; p=0.012). There was no statistical difference concerning abnormal anal cytology or anoscopy between the groups, and no anal intraepithelial lesion was found in either group.
Conclusion
Immunocompetent women with HPV-associated genital lesions and high-risk cervical HPV were more likely to have high-risk anal HPV.
-
Original Article
Antibiotic Susceptibility Patterns and Prevalence of Streptococcus Agalactiae Rectovaginal Colonization Among Pregnant Women in Iran
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):454-459
09-25-2020
Summary
Original ArticleAntibiotic Susceptibility Patterns and Prevalence of Streptococcus Agalactiae Rectovaginal Colonization Among Pregnant Women in Iran
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):454-459
09-25-2020Views122Abstract
Objective
Streptococcus agalactiae is an important pathogen in neonates and pregnant women. Neonatal invasive infections due to S. agalactiae are life-threatening and preventive strategies for this challenge of human have become a concern. The aim of the present study was to determine the prevalence of rectovaginal colonization, related risk factors and antibiotic resistance pattern of S. agalactiae among pregnant women in Iran.
Methods
The present study was performed on 240 pregnant women. Vaginal and rectal swabs were obtained from all of the women and then were transferred to the laboratory. The isolation and identification of S. agalactiae was performed by standard microbiological tests and polymerase chain reaction (PCR) assay. The antimicrobial susceptibility patterns of the isolates were determined by the Kirby-Bauer disk diffusion. Polymerase chain reaction was used to detect ermB and mefA genes in erythromycin-nonsusceptible isolates.
Results
Out of 240 pregnant women, 16 cases (6.7%) were colonized by S. agalactiae. There is no significant association between demographic-obstetric factors and maternal S. agalactiae colonization in the pregnant women. Linezolid, vancomycin and ampicillin were the most effective antibiotics against S. agalactiae. The ermB gene was present in 6 (35.29%) S. agalactiae isolates. However, the mefA gene was not detected in any of the isolates.
Conclusion
Given the relatively significant prevalence of S. agalactiae colonization in the pregnant women in the present study and the risk of serious neonatal infections, the screening of pregnant mothers for the bacteria seems necessary. Our findings highlight the importance of appropriate antibiotic prophylaxis during pregnancy for the prevention of early onset S. agalactiae-neonatal infection and comorbidity.
Key-words antibiotic resistancePolymerase chain reactionPregnant womenRisk factorsStreptococcus agalactiaeSee more -
Original Articles
Sexually Transmitted Infections Detected by Multiplex Real Time PCR in Asymptomatic Women and Association with Cervical Intraepithelial Neoplasia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):540-546
09-01-2018
Summary
Original ArticlesSexually Transmitted Infections Detected by Multiplex Real Time PCR in Asymptomatic Women and Association with Cervical Intraepithelial Neoplasia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):540-546
09-01-2018Views187Abstract
Objective
To determine the frequency of sexually transmitted infections (STIs) in asymptomatic women and the association of STIs with cervical intraepithelial neoplasia (CIN).
Methods
A cross-sectional studywas performed, enrollingwomen examined in a general gynecology clinic and in a colposcopy referral center fromOctober 2014 to October 2015. The colposcopy groupconsisted of 71women, and the general gynecologygroupconsisted of 55 women. Cervical samples were collected for cervical cytology and a multiplex realtime polymerase chain reaction (PCR) was developed to detect human papillomavirus (HPV) and the STIs caused by the following microorganisms: Chlamydia trachomatis, Mycoplasma hominis, Mycoplasma genitalium, Ureaplasma urealyticum, and Neisseria gonorrhoeae. A multivariate analysis was performed by logistic regression, considering the significance level of 0.05.
Results
The general frequency of STIs was: 46.8% (HPV); 27.8% (C. trachomatis); 28.6% (M. genitalium); 0.8% (M. hominis); 4.8% (U. urealyticum); and 4.8% (N. gonorrhoeae). The significant risk factors for CIN were: HPV infection (odds ratio [OR] = 2.53; p = 0.024); C. trachomatis (OR = 3.04; p = 0.009); M. genitalium (OR = 2.37; p = 0.04); and HPV and C. trachomatis coinfection (OR = 3.11; p = 0.023). After the multivariate analysis, a significant associationwas found betweenHPVand CIN(OR = 2.48; 95% confidence interval [95%CI]: 1.04-5.92; p = 0.04); and between C. trachomatis and CIN (OR = 2.69; 95%CI: 1.11-6.53; p = 0.028).
Conclusion
The frequency of STIs was high in asymptomatic patients. Infections by HPV and C. trachomatis were independently associated with the presence of CIN. The high frequency of STIs in asymptomatic women suggests the need for routine screening of these infections.
Key-words Cervical intraepithelial neoplasiaChlamydiaPapillomavirus infectionsPolymerase chain reactionSexually transmitted diseasesSee more -
Original Article
Detection of High-Risk Human Papillomavirus in Cervix Sample in an 11.3-year Follow-Up after Vaccination against HPV 16/18
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):408-414
08-01-2017
Summary
Original ArticleDetection of High-Risk Human Papillomavirus in Cervix Sample in an 11.3-year Follow-Up after Vaccination against HPV 16/18
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):408-414
08-01-2017Views163Abstract
Purpose
the aim of this study was to evaluate the pattern of human papillomavirus (HPV) detection in an 11.3-year post-vaccination period in a cohort of adolescent and young women vaccinated or not against HPV 16/18.
Methods
a subset of 91 women from a single center participating in a randomized clinical trial (2001-2010, NCT00689741/00120848/00518336) with HPV 16/18 AS04- adjuvanted vaccine was evaluated. All women received three doses of the HPV vaccine (n = 48) or a placebo (n = 43), and cervical samples were collected at 6-month intervals. Only in this center, one additional evaluation was performed in 2012. Up to 1,492 cervical samples were tested for HPV-DNA and genotyped with polymerase chain reaction (PCR). The vaccine group characteristics were compared by Chi-square or Fisher exact or Mann-Whitney test. The high-risk (HR)-HPV 6-month-persistent infection rate was calculated. The cumulative infection by HPV group was evaluated by the Kaplan-Meier method and the log-rank test.
Results
the cumulative infection with any type of HPV in an 11.3-year period was 67% in the HPV vaccine group and 72% in the placebo group (p = 0.408). The longitudinal analysis showed an increase of 4% per year at risk for detection of HR-HPV (non-HPV 16/ 18) over time (p = 0.015), unrelated to vaccination. The cumulative infection with HPV 16/18 was 4% for the HPV vaccine group and 29% for the placebo group (p = 0.003). There were 43 episodes of HR-HPV 6-month persistent infection, unrelated to vaccination.
Conclusions
this study showed themaintenance of viral detection rate accumulating HR-HPV (non-HPV-16-18) positive tests during a long period post-vaccination, regardless of prior vaccination. This signalizes that the high number of HPV-positive testsmay be maintained after vaccination.
Key-words Cervix uteriHPV DNA testsHuman papillomavirushuman papillomavirus vaccine 16 and 18 L1 VLPpapillomavirus vaccinesPolymerase chain reactionSee more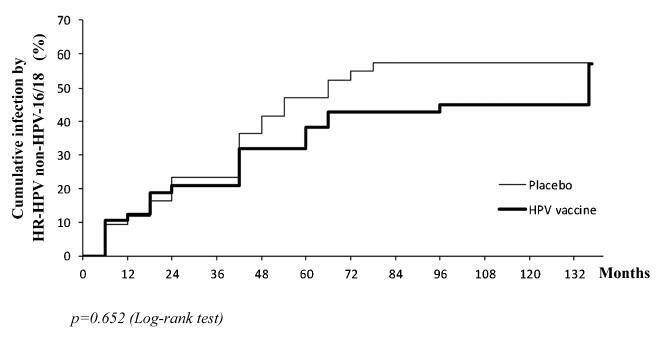
-
Original Article
Incidence of Cervical Human Papillomavirus and Cervical Intraepithelial Neoplasia in Women with Positive and Negative HIV Status
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):231-238
05-01-2016
Summary
Original ArticleIncidence of Cervical Human Papillomavirus and Cervical Intraepithelial Neoplasia in Women with Positive and Negative HIV Status
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):231-238
05-01-2016Views167Abstract
Objectives
To evaluate the incidence and factors associated with cervical intraepithelial neoplasia (CIN) and cervical infection by human papillomavirus (HPV) among HIV-positive and HIV-negative women.
Methods
A cohort of 103 HIV positive and 113 HIV negative women were monitored between October 2008 and February 2012, for at least one year. Procedures included cervical cytology, DNA/HPV detection by polymerase chain reaction, colposcopy with biopsy if necessary, followed by an interview for exposure characteristics data. CIN was based on the histopathological results.
Results
The incidence of CIN was of 8.8 and 4.6 cases/100 women-years in HIVpositive and HIV-negative women, respectively. HIV-positive women presented a hazard ratio (HR) of 2.8 for CIN and developed lesions earlier (0.86 year) than HIVnegative women (2 years) (p = 0.01). The risk of developing CIN decreased with age (HR = 0.9) and marital status (HR = 0.4). HPV patients presented a higher incidence of CIN when compared HIV-positive and HIV-negative women (p = 0.01). The incidence of HPV cervical infection was 18.1 and 11.4 cases/100 women-years in HIV-positive and HIV-negative women, respectively. Those HIV-positive presented earlier HPV infection (p = 0.002). The risk of developing HPV infection decreased with age and was higher among HIV-positive women. HPV 16 was the most common type in HIV-positive women, and also the type most closely associated with CIN in HIV-negative women.
Conclusions
HIV-positive women had a greater incidence of HPV and CIN, and in a shorter time interval. More rigorous and timely clinical control is required for this group.
Key-words Cervical intraepithelial neoplasiaHIV infectionsHPV DNA probesPapillomavirus infectionsPolymerase chain reactionSee more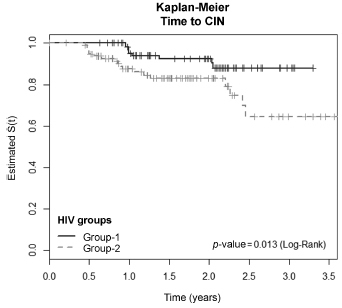
-
Artigos Originais
Prevalence of cervical infection by human papillomavirus and cervical intraepithelial neoplasia in HIV-positive and negative women
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):178-185
04-01-2015
Summary
Artigos OriginaisPrevalence of cervical infection by human papillomavirus and cervical intraepithelial neoplasia in HIV-positive and negative women
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):178-185
04-01-2015DOI 10.1590/SO100-720320150005184
Views107See morePURPOSE:
To conduct a comparative study between two groups of women (HIV positive and negative) analyzing: the prevalence of cervical intraepithelial neoplasia (CIN) and cervical HPV infection; viral risk and relationship with development of CIN; and sociodemographic and behavioral parameters that influence cervical HPV infection and the development of CIN.
METHODS:
A cross-sectional study in which 202 HIV-positive women and 164 HIV-negative women were analyzed to assess the prevalence of CIN and 171 HIV-positive women and 160 HIV-negative women were analyzed to assess the prevalence of cervical HPV infection. The following procedures were performed on the occasion of each medical visit: collection of cervical samples for cytology and polymerase chain reaction (PCR) to detect HPV DNA; colposcopy; standardized questionnaire to collect demographic and behavioral data; and biopsy of all colposcopic changes. Histopathology was the gold standard for the diagnosis of CIN.
RESULTS:
The prevalence of CIN was 2.4 and 15.3% (p<0.001) and the prevalence of cervical HPV infection was 37.1 and 55.5% (p=0.002), respectively, among HIV-negative and -positive women. HIV-positive women had a higher risk of HPV infection (35.7 and 23.6%) (p=0.02). HPV 16 was the most prevalent virus type, occurring in 11.3 and 10.2% of HIV-positive and negative women and was also more prevalent among women presenting CIN in both groups. Factors associated fwith the development of CIN were: HIV infection (HT=4.64; 95%CI 2.23-9.65), age (HT=0.95; 95%CI 0.93-0.98 for each year of life) and marital status(HT=0.49; 95%CI 0.30-0.80). Associated factors for HPV infection were: HIV presence (HT=2.72; 95%CI 1.77-4.17), greater number of sexual partners (HT=1.87; 95%CI 1.23-2.84), age (HT=0.97; 95%CI 0.95-0.99 for each year of life) and marital status (HT=0.65; 95%CI 0.42-1.0 for stable union/widows).
CONCLUSION:
The prevalence of CIN and cervical HPV infection was higher in HIV-positive women, who also presented a higher risk of HPV infections and multiple viral types. Type 16 was predominant in both groups and in women with CIN. Older women and women with stable union/widows were less likely to acquire cervical HPV infection and CIN.
-
Artigos Originais
Prevalence of Chlamydia trachomatis and risk factors associated with infection detected in endocervical sample
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):379-383
10-10-2013
Summary
Artigos OriginaisPrevalence of Chlamydia trachomatis and risk factors associated with infection detected in endocervical sample
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):379-383
10-10-2013DOI 10.1590/S0100-72032013000800008
Views59PURPOSE: It was to determine the prevalence of Chlamydia trachomatis and the risk factors associated with infection in endocervical specimens from women seen in outpatient Obstetrics and Gynecology. METHODS: Samples of endocervical secretion of 200 women treated at the University Hospital of the Federal University of Rio Grande were analyzed for the presence of C. trachomatis by polymerase chain reaction (PCR) using primers that amplify CT05/CT06 281 base pairs of the main outer membrane protein of C. trachomatis. All participants completed a pre-coded and self-report questionnaire. Data were analyzed with the SPSS 17.0 software; for multivariate analysis it was used Poisson regression. RESULTS: Of the 200 women who were included in the study, the prevalence of infection with C. trachomatis was 11% (22 patients) and these 55 (27.5%) were positive for HPV. Risk factors associated with infection by C. trachomatis were: 8 years or less of schooling (p<0.001), family income below the poverty level (p=0.005), first intercourse at age 15 or less (p=0.04) and being a carrier of the virus HIV (p<0.001). After multivariate analysis, only the variables of schooling or less than eight years (PR 6.0; 95%CI 1.26 - 29.0; p=0.02) and presence of HIV (RP 14.1; 95%CI 3.4 - 57.5; p<0.001) remained statistically significant. CONCLUSIONS: The prevalence of C. trachomatis in endocervical specimens by PCR was 11%. The factors associated with a higher infection by C. trachomatis were lower education and being HIV positive.
Key-words Chlamydia infectionsPolymerase chain reactionPrevalenceQuestionnairesRisk factorsSexually transmitted diseasesSee more -
Artigos Originais
Risk factors and prevalence of HPV infection in patients from Basic Health Units of an University Hospital in southern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(5):226-232
07-05-2013
Summary
Artigos OriginaisRisk factors and prevalence of HPV infection in patients from Basic Health Units of an University Hospital in southern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(5):226-232
07-05-2013DOI 10.1590/S0100-72032013000500007
Views138PURPOSE: To determine the HPV prevalence and genotypes and to identify factors associated with infection in pregnant and non-pregnant women with positive or negative HIV-1, treated in Gynecology and Obstetrics Ambulatories and in Health Primary Units, in Rio Grande, Rio Grande do Sul State, Brazil. METHODS: Cervical cells samples from 302 patients were analyzed for HPV presence and genotypes were determined by nested and sequencing polymerase chain reaction. We calculated prevalence ratios associated with the studied variables by Fisher's exact or χ² tests, and Poisson's regression. Women with insufficient material were excluded from the study. RESULTS: HPV was detected in 55 of the 302 women included in the study (18.2%); of these, 31 were pregnant, showing a significant association for HPV (p=0.04) when compared to non-pregnant ones. Risk factors for the infection were: patients aged <20 years-old (p=0.04), early initiation of sexual life (p=0.04), absence of cytological test (p=0.01), diagnosis of altered cytology (p=0.001), and counting <349 cells/mm³ (p=0.05). However, multi-parity was found to be a protective factor for the infection (p=0.01). Multivariate analysis showed that age <20 years-old (PR=2.8; 95%CI 1.0 - 7.7, p=0.04) and an altered cytological result (PR=11.1; 95%CI 3.0 - 4.1, p=0.001) were significantly associated with infection. HPV genotype was determined in 47 samples (85.4%) presenting one genotype per infection: eight HPV 16 and 58; six HPV 6; four HPV 18 and 33; three HPV 53 and 82; two HPV 83 and 61; one HPV 31, 35, 45, 64, 68, 71 and 85. CONCLUSIONS: The prevalence of HPV detection was 18.2%, the most frequent genotypes were 16 and 58, and sociodemographic and gynecological factors were associated with viral infection.
Key-words BrazilHealth centersHospitals, universityPapillomavirus infectionsPolymerase chain reactionPregnant womenPrevalenceRisk factorsSee more


