-
Review Article04-30-2025
Letrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
Abstract
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
Views168Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Key-words ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeSee more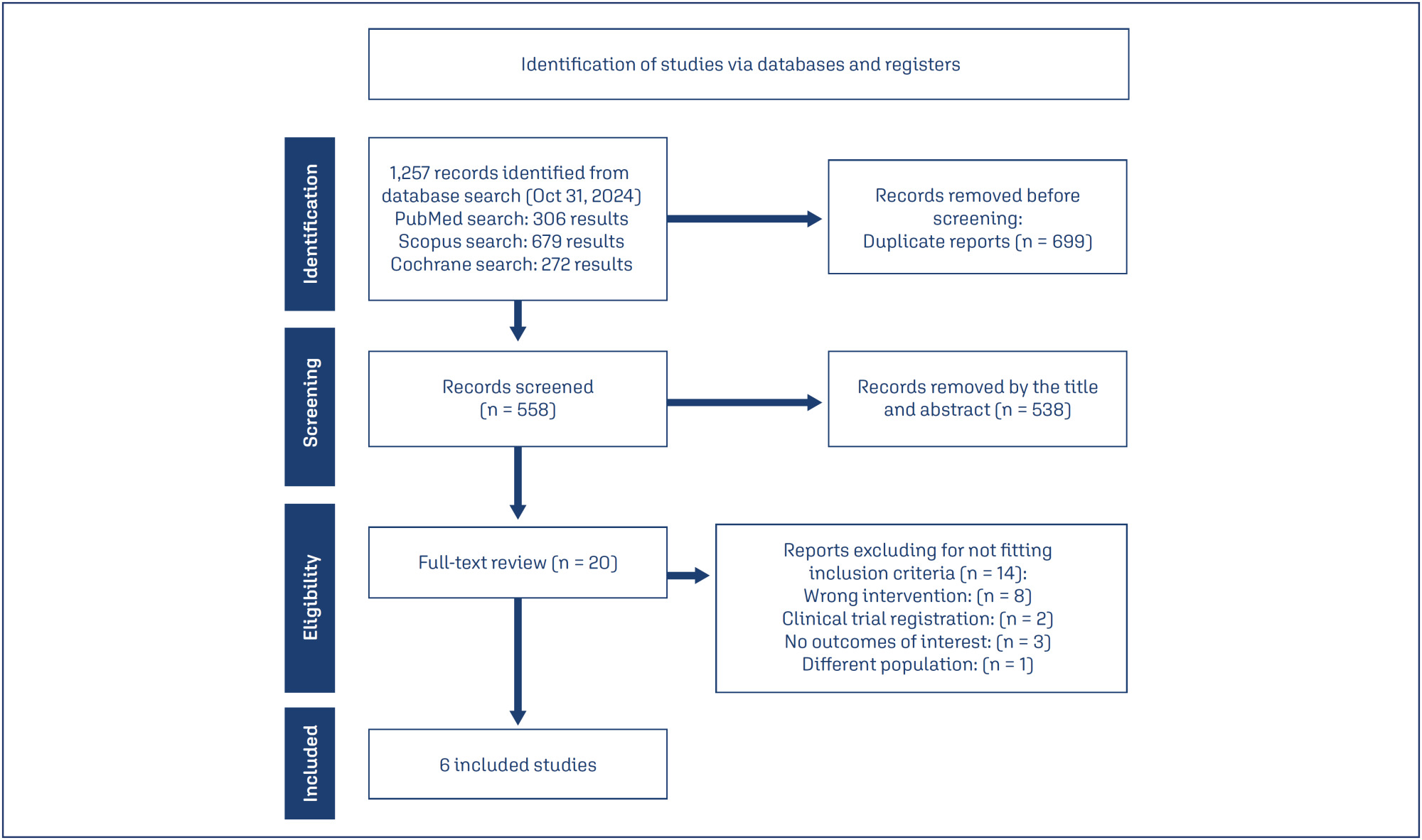
-
Review Article06-27-2024
Effects of vitamin D supplementation on oxidative stress biomarkers of Iranian women with polycystic ovary syndrome: a meta-analysis study
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo37
Abstract
Review ArticleEffects of vitamin D supplementation on oxidative stress biomarkers of Iranian women with polycystic ovary syndrome: a meta-analysis study
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo37
Views269Abstract
Objective
To identify the impact of redox imbalance on the clinical evolution of patients with polycystic ovary syndrome and carry out a qualitative and quantitative projection of the benefits of vitamin D supplementation.
Data sources
Combinations of the keywords polycystic ovary syndrome, vitamin D, oxidative stress, reactive oxygen species, antioxidant, and free radicals were used in PubMed, Cochrane Library, LILACS, EMBASE, and Web of Science databases. The last search was conducted on August 22, 2023.Selection of studies: Based on the inclusion and exclusion criteria, studies were selected considering a low risk of bias, published in the last 5 years in English, which investigated the effects of vitamin D supplementation in women with PCOS, focusing on oxidative stress markers. Of the 136 articles retrieved, 6 intervention studies (445 women) were included.
Data collection
The risk of bias in included studies was assessed using the Jadad scale, and analysis and visualization of continuous data were performed using Review Manager 5.4.1, summarized as standardized mean differences (SMD) with confidence intervals (CI) of 95%.
Data synthesis
Vitamin D effectively reduced malondialdehyde (P=0.002) and total testosterone (P=0.0004) levels and increased total antioxidant capacity levels (P=0.01). Although possible improvements in the modified Ferriman–Gallwey hirsutism score, levels of sex hormone-binding globulin, and free androgen index were identified and the results were not statistically significant.
Conclusion
Vitamin D is a promising alternative for the treatment of PCOS with a positive influence on the oxidative, metabolic, and endocrine disorders of this syndrome.
Key-words Antioxidant therapycholecalciferolHyperandrogenismOxidative stressPolycystic ovary syndromeSee more -
Review Article06-27-2022
Polycystic Ovary Syndrome in Adolescence: Challenges in Diagnosis and Management
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):425-433
Abstract
Review ArticlePolycystic Ovary Syndrome in Adolescence: Challenges in Diagnosis and Management
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):425-433
Views380See moreAbstract
Diagnosing polycystic ovary syndrome (PCOS) during adolescence is challenging since normal pubertal development overlap typical features of this syndrome. The authors aim to summarize the existing evidence concerning PCOS in adolescence, particularly its diagnostic criteria and therapeutic options. A search throughout medical databases such as PubMed and MedScape was performed. Diagnostic criteria include irregular menstrual cycles according to time postmenarche and evidence of clinical hyperandrogenism and/or biochemical hyperandrogenism, provided other causes have been excluded. Polycystic ovarianmorphology ought not to be used as a diagnostic criterion. Treatment should targetmanifestations and/or comorbidities, even in the absence of a definite diagnosis. Lifestyle interventions are the first-line treatment. Combined oral contraceptives, metformin or antiandrogens may also be considered as adjuvants. Screening for PCOS in adolescence is crucial as it allows an early intervention on the symptoms and comorbidities presented leading to better long-term reproductive and metabolic outcomes.
-
Original Article01-05-2020
Physical Performance Regarding Handgrip Strength in Women with Polycystic Ovary Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):811-819
Abstract
Original ArticlePhysical Performance Regarding Handgrip Strength in Women with Polycystic Ovary Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):811-819
Views236See moreAbstract
Objective
The present study aimed to investigate the physical performance of handgrip strength (HGS) in women with polycystic ovary syndrome (PCOS).
Methods
A case-control study that included 70 women with PCOS and 93 agematched healthy women aged between 18 and 47 years with body mass index (BMI) between 18 Kg/m2-39.9 Kg/m2. The serum levels of total testosterone, androstenedione, insulin, estradiol, thyroid-stimulating hormone (TSH), prolactin, sex hormonebinding globulin (SHBG), and 17-hydroxyprogesterone (17-OHP) were measured. The free androgen index (FAI) and the homeostatic model assessment of insulin resistance (HOMA-IR) were calculated. The body composition regions of interest (ROIs) were assessed by dual-energy X-ray absorptiometry (DXA), and the handgrip strength (HGS) was evaluated for both the dominant and the non-dominant hands with a manual Sammons Preston (Bolingbrook, IL, US) bulb dynamometer.
Results
Women with PCOS had high serum levels of total testosterone (p < 0.01), androstenedione (p = 0.03), and insulin (p < 0.01), as well as high FAI (p < 0.01) and HOMA-IR (p = 0.01) scores. Compared with the non-PCOS group, the PCOS group had greater total lean mass in the dominant hand (p < 0.03) and greater HGS in both the dominant and the non-dominant hands (p < 0.01). The HGS was correlated with lean mass (p < 0.01).
Conclusion
Women with PCOS have greater HGS. This may be associated with age and BMI, and it may be related to lean mass. In addition, the dominance effect on muscle mass may influence the physical performance regarding HGS in women with PCOS.
-
Original Article04-17-2020
Increased Sympathetic Cardiac Autonomic Modulation after Two Consecutive Tilt Tests in Women with Polycystic Ovary Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):81-89
Abstract
Original ArticleIncreased Sympathetic Cardiac Autonomic Modulation after Two Consecutive Tilt Tests in Women with Polycystic Ovary Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):81-89
Views196Abstract
Objective
The present study aimed to analyze cardiac autonomic modulation via spectral and symbolic analysis of heart rate variability (HRV) in women with polycystic ovary syndrome (PCOS) who were subjected to two consecutive tilt tests.
Methods
A total of 64 women were selected and divided into 2 groups: control (without PCOS), and PCOS. Concentrations of follicle-stimulating hormone, luteinizing hormone, prolactin, estradiol, homocysteine, sex hormone-binding globulin, thyroid stimulating hormone, fasting insulin, testosterone, androstenedione, and 17-hydroxyprogesterone levels, triglycerides, free androgen index (FAI), and homeostasis assessment model (HOMA-IR) were assessed. Cardiac autonomic modulation was evaluated by spectral and symbolic analyses during two consecutive tilt tests (two moments) and supine moments before, between and after (three moments) the tilt tests.
Results
Women with PCOS had higher fasting insulin, HOMA-IR indexes, testosterone and FAI. Additionally, we observed that the PCOS group had greater sympathetic autonomic cardiac modulation in supine 2, tilt 1, and supine 3 moments compared with controls.
Conclusion
Women with PCOS had higher autonomic sympathetic cardiac modulation even after a second tilt test. No adaptation to this provocative test was observed. Spectral analysis was more sensitive for identifying differences between groups than the symbolic analysis.
Key-words cardiac autonomic modulationHyperandrogenismPolycystic ovary syndromespectral analysissymbolic analysisSee more -
Original Article04-01-2018
Association between Insulin Resistance and Cardiovascular Risk Factors in Polycystic Ovary Syndrome Patients
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):188-195
Abstract
Original ArticleAssociation between Insulin Resistance and Cardiovascular Risk Factors in Polycystic Ovary Syndrome Patients
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):188-195
Views206Abstract
Objective
To analyze the association between the indirect methods of evaluating insulin resistance (IR) and blood pressure, anthropometric and biochemical parameters in a population of polycystic ovary syndrome (PCOS) patients.
Methods
Cross-sectional study performed at the Hospital Universitário de Brasília (HUB, in the Portuguese acronym) involving PCOS patients diagnosed from January 2011 to January 2013. Four indirect methods, namely, fasting blood insulin level, fasting glucose/insulin ratio (G/I), homeostatic model-assessment-insulin resistance (HOMA-IR), and the quantitative insulin sensitivity check index (QUICKI), were used to obtain the IR diagnosis. The data were analyzed using the test of proportions, the Chisquare test, and Fisher exact test, when indicated.
Results
Out of the 83 patients assessed, aged 28.79 ± 5.85, IR was found in 51.81- 66.2% of them using the G/I ratio and the QUICKI, respectively. The test of proportions did not show a significant difference between the methods analyzed. The proportion of IR diagnoses was statistically higher in obese women than in women with normal body mass index (BMI). We observed a statistically significant association between all the methods for diagnosing IR and BMI, waist circumference (WC) and lipid accumulation product (LAP). With regards to arterial hypertension (AH), we observed a significant association according to three methods, with the exception of the ratio G/I.
Conclusion
Insulin resistance prevalence varied according to the diagnostic method employed,with no statistical difference between them. The proportion of IR diagnoses was statistically higher in obese women than in women with normal BMI.We observed a significant association between IR andWC, BMI, LAP, as well as dyslipidemia and AH in a high proportion of patients.
Key-words Body mass indexInsulin resistancelipid accumulation productPolycystic ovary syndromeWaist circumferenceSee more


