-
Review Article
Characterization of Placental Infection by Zika Virus in Humans: A Review of the Literature
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):577-585
10-23-2020
Summary
Review ArticleCharacterization of Placental Infection by Zika Virus in Humans: A Review of the Literature
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):577-585
10-23-2020Views145See moreAbstract
Objective
The aim of the current review is to present a systematic evaluation of reported human placental findings in cases of zika virus (ZIKV) infection.
Data
sources We reviewed the EMBASE, PUBMED, and SCIELO databases until June 2019, without language restrictions. Selection of studies The search terms placenta AND zika virus were used. The inclusion criteria of the studies were studies that reported placental findings in humans. Experimental studies, reviews, notes or editorials were excluded. A total of 436 studies were retrieved; after duplicate exclusion, 243 articles had their titles screened, and 128 had their abstract read; of those, 32 were included in the final analysis (18 case reports, 10 case series, and 4 cohorts)
Data collection
We collected data concerning the author, year of publication, study design, number of participants, number of placental samples, onset of symptoms, perinatal outcomes, and main findings on histological analysis.
Data synthesis
The placental pathologic findings were described as mild and nonspecific, similar to those of other placental infections, including chronic placentitis, chronic villitis, increased Hofbauer cells, irregular fibrin deposits, increased mononuclear cells in the villus stroma, villous immaturity, edema, hypervascularization, stromal fibrosis, calcification, and focal necrosis of syncytiotrophoblasts.
Conclusion
Zika infection presents unspecific placental findings, similar to other infections in the toxoplasmosis, other agents, rubella, cytomegalovirus, and herpes (TORCH)group. Characterizing and standardizing placental findings after zika virus infection is key to understanding the mechanisms of congenital diseases.
-
Original Article
High Incidence of Herpes Simplex Virus-1 in Cord Blood and Placenta Infection of Women in Southern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):5-11
03-27-2020
Summary
Original ArticleHigh Incidence of Herpes Simplex Virus-1 in Cord Blood and Placenta Infection of Women in Southern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):5-11
03-27-2020Views157See moreAbstract
Objective
Estimate the prevalence of human herpesvirus type 1 HSV-1 DNA in placental samples, its incidence in umbilical cord blood of newborns and the associated risk factors.
Methods
Placental biopsies and umbilical cord blood were analyzed, totaling 480 samples, from asymptomatic parturients and their newborns at a University Hospital. Nested polymerase chain reaction (PCR) and gene sequencingwere used to identify the virus; odds ratio (OR) and relative risk (RR) were performed to compare risk factors associated with this condition.
Results
The prevalence of HSV-1 DNA in placental samples was 37.5%, and the incidence in cord blood was 27.5%. Hematogenous transplacental route was identified in 61.4% from HSV-1+ samples of umbilical cord blood paired with the placental tissue. No evidence of the virus was observed in the remaining 38.6% of placental tissues, suggesting an ascendant infection from the genital tract, without replication in the placental tissue, resulting in intra-amniotic infection and vertical transmission, seen by the virus in the cord blood. The lack of condom use increased the risk of finding HSV-1 in the placenta and umbilical cord blood.
Conclusion
The occurrence of HSV-1 DNA in the placenta and in cord blood found suggests vertical transmission from asymptomatic pregnant women to the fetus.
-
Original Articles
Placental Growth Measures in Relation to Birth Weight in a Latin American Population
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):373-380
08-01-2016
Summary
Original ArticlesPlacental Growth Measures in Relation to Birth Weight in a Latin American Population
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):373-380
08-01-2016Views152See moreAbstract
Introduction
The placenta, translates how the fetus experiences the maternal environment and is a principal influence on birth weight (BW).
Objective
To explore the relationship between placental growth measures (PGMs) and BW in a public maternity hospital.
Methods
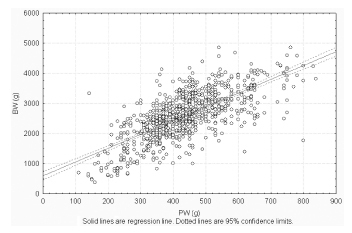
Observational retrospective study of 870 singleton live born infants at Hospital Maternidad Sardá, Universidad de Buenos Aires, Argentina, between January 2011 and August 2012 with complete data of PGMs. Details of history, clinical and obstetrical maternal data, labor and delivery and neonatal outcome data, including placental measures derived from the records, were evaluated. The following manual measurements of the placenta according to standard methods were performed: placental weight (PW, g), larger and smaller diameters (cm), eccentricity, width (cm), shape, area (cm2), BW/PW ratio (BPR) and PW/BW ratio (PBR), and efficiency. Associations between BW and PGMs were examined using multiple linear regression.
Results
Birth weight was correlated with placental weight (R2 =0.49, p < 0.001), whereas gestational age was moderately correlated with placental weight (R2 =0.64, p < 0.001). By gestational age, there was a positive trend for PW and BPR, but an inverse relationship with PBR (p < 0.001). Placental weight alone accounted for 49% of birth weight variability (p < 0,001), whereas all PGMs accounted for 52% (p < 0,001). Combined, PGMs, maternal characteristics (parity, pre-eclampsia, tobacco use), gestational age and gender explained 77.8% of BW variations (p < 0,001). Among preterm births, 59% of BW variances were accounted for by PGMs, compared with 44% at term. All placental measures except BPR were consistently higher in females than in males, which was also not significant. Indices of placental efficiency showed weakly clinical relevance.
Conclusions
Reliable measures of placental growth estimate 53.6% of BW variances and project this outcome to a greater degree in preterm births than at term. These findings would contribute to the understanding of the maternal-placental programming of chronic diseases.
-
Original Articles
Hofbauer cells morphology and density in placentas from normal and pathological gestations
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(9):407-412
11-06-2013
Summary
Original ArticlesHofbauer cells morphology and density in placentas from normal and pathological gestations
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(9):407-412
11-06-2013DOI 10.1590/S0100-72032013000900005
Views143See morePURPOSE: In placentas from uncomplicated pregnancies, Hofbauer cells either disappear or become scanty after the fourth to fifth month of gestation. Immunohistochemistry though, reveals that a high percentage of stromal cells belong to Hofbauer cells. The aim of this study was to investigate the changes in morphology and density of Hofbauer cells in placentas from normal and pathological pregnancies. METHODS: Seventy placentas were examined: 16 specimens from normal term pregnancies, 10 from first trimester's miscarriages, 26 from cases diagnosed with chromosomal abnormality of the fetus, and placental tissue specimens complicated with intrauterine growth restriction (eight) or gestational diabetes mellitus (10). A histological study of hematoxylin-eosin (HE) sections was performed and immunohistochemical study was performed using the markers: CD 68, Lysozyme, A1 Antichymotrypsine, CK-7, vimentin, and Ki-67. RESULTS: In normal term pregnancies, HE study revealed Hofbauer cells in 37.5% of cases while immunohistochemistry revealed in 87.5% of cases. In first trimester's miscarriages and in cases with prenatal diagnosis of fetal chromosomal abnormalities, both basic and immunohistochemical study were positive for Hofbauer cells. In pregnancies complicated with intrauterine growth restriction or gestational diabetes mellitus, a positive immunoreaction was observed in 100 and 70% of cases, respectively. CONCLUSIONS: Hofbauer cells are present in placental villi during pregnancy, but with progressively reducing density. The most specific marker for their detection seems to be A1 Antichymotrypsine. It is remarkable that no mitotic activity of Hofbauer cells was noticed in our study, as the marker of cellular multiplication Ki-67 was negative in all examined specimens.
-
Article
Correlation between placental thickness in the second and third trimester and fetal weight
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(7):317-322
09-27-2013
Summary
ArticleCorrelation between placental thickness in the second and third trimester and fetal weight
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(7):317-322
09-27-2013DOI 10.1590/S0100-72032013000700006
Views57See morePURPOSE: To investigate relationship between placental thickness during the second and third trimesters and placental and birth weights. METHODS: From January 2011 to June 2012, a total of 250 singleton pregnant women presented at our antenatal clinic were enrolled in this prospective study. All recruited women were assessed at the 1st trimester screening for baseline demographic and obstetric data. The placental thickness was measured trans-abdominally by placing the ultrasound transducer perpendicularly to the plane of the placenta, in the area of the cord insertion at second and third trimester. Pearson's correlation analysis was used to establish the degree of relationship between placental thickness and birth and placental weights. RESULTS: Of 250 recruited participants, 205 women were able to complete the study. The mean age of cases was 26.4±5.1. Values of mean birth and placental weights were 305.56±657.0 and 551.7±104.8 grams respectively. Ultrasonographic measures of placental thickness in second and third trimester and changes between them were 21.68±4.52, 36.26±6.46 and 14.67±5.67 mm respectively. There was a significant positive correlation between placental thickness and birth weight in the second and third trimesters (r=0.15, p=0.03; r=0.14, p=0.04 correspondingly). CONCLUSION: According to our study, birth weight has a positive relation with both second and third trimester placental thickness; however, placental thickness change could not predict low birth weight.
-
Artigos Originais
Influence of maternal and fetal intercurrences on the different degrees of chorioamnionitis
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):153-157
05-11-2012
Summary
Artigos OriginaisInfluence of maternal and fetal intercurrences on the different degrees of chorioamnionitis
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):153-157
05-11-2012DOI 10.1590/S0100-72032012000400003
Views61See morePURPOSE: To evaluate the influence of maternal complications, prematurity, fetal anthropometric parameters and conditions of the newborn on different degrees of chorioamnionitis. METHODS: We analyzed 90 placentas from deliveries performed at the General Hospital of Triângulo Mineiro Federal University with a diagnosis of inflammation in the anatomopathological exams. We reviewed the medical records to obtain relevant maternal and fetal information. The infections were classified as grade I - deciduitis; grade II - chorioamnionitis; grade III - chorioamnionitis and vasculitis; grade IV - neonatal sepsis and grade V - fetal death and pneumonitis. RESULTS: Among the pregnant women analyzed, 50.0% had no complications, 15.0% had ruptured membranes, 15.0% urinary tract infection, 7.5% hypertensive disorders, 7.5% transvaginal infection, 5.0% hematogenous infection, and 11.1% other complications. More than a half the neonates were males and 72.2% were born at term. Analysis of the degree of chorioamnionitis showed that 56.7% had grade I, 22.2% grade II, 4.4% grade III, 10.0% grade IV, and 6.7% grade V. Data were analyzed statistically by the Χ2 test for qualitative variables and by the Spearman test for correlation analysis. The higher grades of chorioamnionitis were observed in cases of maternal complications. We observed negative correlations between all parameters and the degree of fetal chorioamnionitis, which were significant regarding weight, length, thoracic circumference and Apgar score in the first and fifth minutes. CONCLUSIONS: The different patterns of chorioamnionitis were related to different maternal and fetal clinical features, affecting the life conditions of the newborn and the severity of morphological lesions found in stillbirths.
-
Relato de Caso
Placental vascular lesion as cause of IUGR and nonimmune fetal hydrops in twin pregnanc
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(12):421-425
01-23-2011
Summary
Relato de CasoPlacental vascular lesion as cause of IUGR and nonimmune fetal hydrops in twin pregnanc
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(12):421-425
01-23-2011DOI 10.1590/S0100-72032011001200008
Views132See morePlacenta vascular lesions are a group of distinct yet related entities that include chorangiomas and diffuse multifocal chorangiomatosis. Chorangioma is an expansive nodular lesion with an incidence of about 1%. Diffuse multifocal chorangiomatosis is rare (0.2%) and mostly seen in placentas before the 32nd gestational week. The authors present a case of a monochorionic/biamniotic twin pregnancy, in which, at the 26th gestational week, one fetus developed intrauterine growth restriction (IUGR), hydrops, and anemia associated with a tumor of the placenta with increased vascularization in the Doppler study. Pathological examination of the placenta diagnosed diffuse multifocal chorangiomatosis. This rare case report of diffuse multifocal chorangiomatosis with prenatal manifestations resembling those of a chorangioma proves that prenatal ultrasound detection of a placenta tumor, with increased vascularization at Doppler study, must raise other diagnostic possibilities beside chorangioma.
-
Artigos Originais
Laser ablation of placental vessels for treatment of severe twin-twin transfusion syndrome: experience from an university center in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(5):214-221
08-26-2010
Summary
Artigos OriginaisLaser ablation of placental vessels for treatment of severe twin-twin transfusion syndrome: experience from an university center in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(5):214-221
08-26-2010DOI 10.1590/S0100-72032010000500003
Views129See morePURPOSE: to describe the results of laser ablation of placental vessels for the treatment of severe twin-to-twin transfusion syndrome in an university center in Brazil. METHODS: retrospective observational study of patients treated at UNICAMP from 2007 to 2009. Laser ablation of placental vessels was performed in cases of severe twin-twin transfusion syndrome (Quintero stages II, III and IV) diagnosed before 26 complete weeks of gestation. The main variables evaluated in this series were gestational age at delivery, survival (discharge from the nursery) of at least one twin and neurological damage in survivors. Logistic regression was used to investigate the influence of cervical length, gestational age and stage of the disease (before the surgery) on the occurrence of delivery/abortion and fetal death after the intervention, and the influence on severe preterm birth and survival. RESULTS: in the whole series, at least one twin survived in 63.3% of cases (19/30). Among patients who did not have delivery/abortion after surgery, the survival of at least one twin was 82.6% (19/23). In this subgroup (n=23), mean gestational age in delivery was 31.9 weeks and neurological damage was identified in one neonate (1/31; 3.2%). Cervix length influenced the occurrence of delivery/abortion after surgery (p-value=0.008). Among seven patients (7/30; 23.3%) who carried this complication, five (5/7; 71.4%) had cervix length lower than 15 mm. Among the 23 patients who did not have delivery/abortion as a result of the surgery, the highest stages of the disease (III and IV) increased the risk of delivery prior to 32 complete weeks of gestation (p-value=0.025) and decreased the chance of survival of both twins (p-value=0.026). CONCLUSIONS: the results are similar to those available in the literature. In our series, the main factors associated with poorer results were short cervix (lower than 15 mm) and the highest stages of the disease (III and IV) at the time of the treatment.


