Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo10
03-18-2025
Preterm birth remains a significant contributor to neonatal morbidity and mortality. The use of cervical pessaries as an intervention for preventing preterm delivery in women with a short cervix has been a subject of interest. We evaluated the effectiveness of cervical pessary compared to standard care in preventing preterm delivery in women with a short cervix.
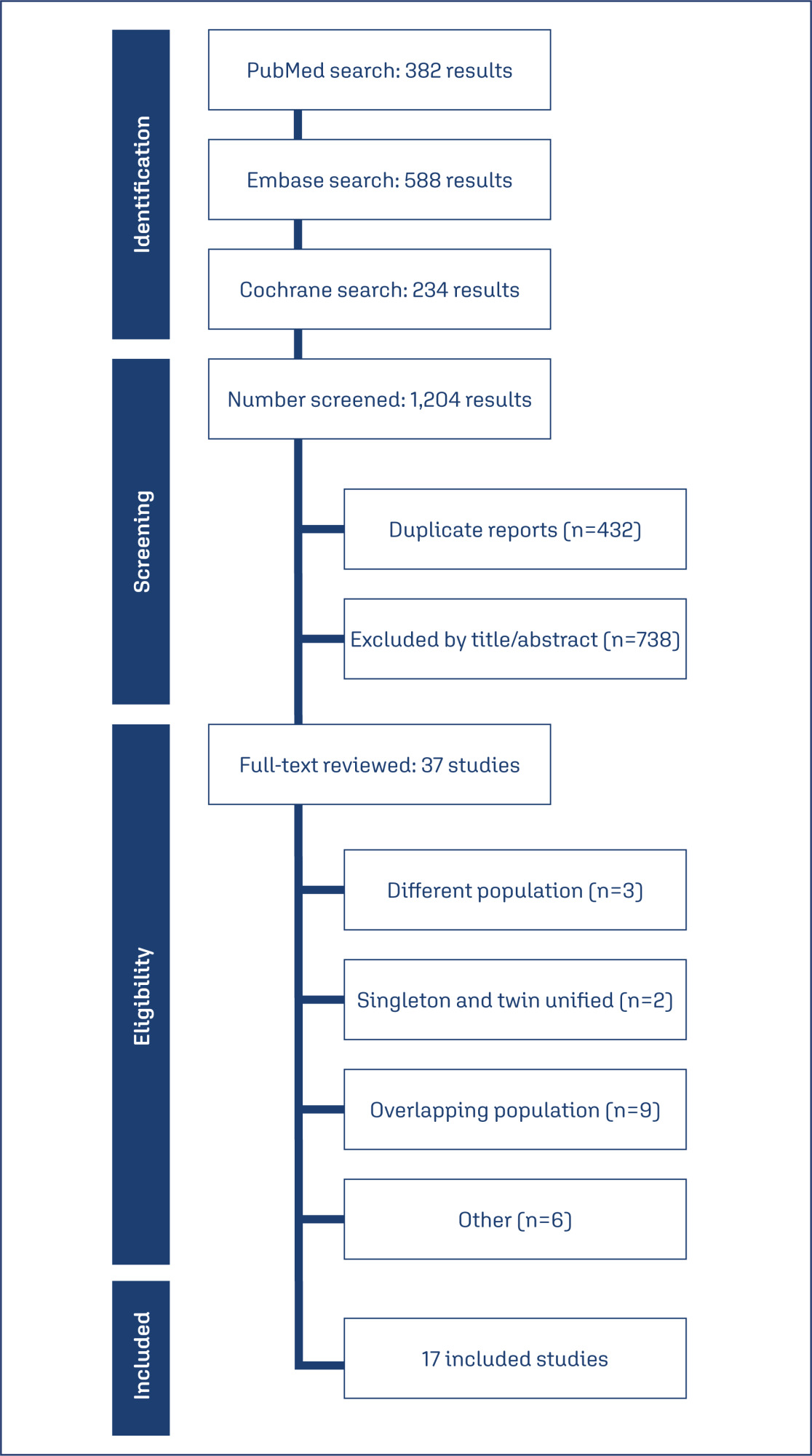
Databases were systematically searched in PubMed, Cochrane, and Embase databases in December 2023.
Randomized clinical trials with the outcomes of interest were included.
We computed risk ratios for binary endpoints, with 95% confidence intervals. Heterogeneity was assessed using I2 statistics. Data were analyzed using R software (version 4.3.0). The primary outcomes of interest were preterm delivery before 37 weeks, and preterm delivery before 34 weeks.
Seventeen studies with 5,704 patients were included. The use of cervical pessary was associated with a decreased risk of preterm delivery before 37 (RR 0.88; 95% CI 0.81-0.96) and 34 weeks (RR 0.79; 95% CI 0.63-0.99) of gestation in twin pregnancies as compared to standard care without progesterone. There were no significant differences in preterm delivery in singleton pregnancy, neonatal outcomes, preterm premature rupture of the membranes or chorioamnionitis.
The use of cervical pessary was associated with a significant reduction in preterm delivery at 34 and 37 weeks of gestation in twin pregnancies among patients with a short cervix compared to no treatment. No significant difference was found in singleton pregnancies or maternal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo39i
09-06-2024
This study aims to create a new screening for preterm birth < 34 weeks after gestation with a cervical length (CL) ≤ 30 mm, based on clinical, demographic, and sonographic characteristics.
This is a post hoc analysis of a randomized clinical trial (RCT), which included pregnancies, in middle-gestation, screened with transvaginal ultrasound. After observing inclusion criteria, the patient was invited to compare pessary plus progesterone (PP) versus progesterone only (P) (1:1). The objective was to determine which variables were associated with severe preterm birth using logistic regression (LR). The area under the curve (AUC), sensitivity, specificity, and positive predictive value (PPV) and negative predictive value (NPV) were calculated for both groups after applying LR, with a false positive rate (FPR) set at 10%.
The RCT included 936 patients, 475 in PP and 461 in P. The LR selected: ethnics white, absence of previous curettage, previous preterm birth, singleton gestation, precocious identification of short cervix, CL < 14.7 mm, CL in curve > 21.0 mm. The AUC (CI95%), sensitivity, specificity, PPV, and PNV, with 10% of FPR, were respectively 0.978 (0.961-0.995), 83.4%, 98.1%, 83.4% and 98.1% for PP < 34 weeks; and 0.765 (0.665-0.864), 38.7%, 92.1%, 26.1% and 95.4%, for P < 28 weeks.
Logistic regression can be effective to screen preterm birth < 34 weeks in patients in the PP Group and all pregnancies with CL ≤ 30 mm.