Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo86
HPV infection is considered the most common sexually transmitted virus today. The persistence of HPV is the main cause for the development of precursor lesions and cervical cancer. There are environmental and non-environmental factors that contribute to the persistence of the virus. Studies indicate a possible relationship between the vaginal microbiota (environmental factor) and the risk of high-grade cervical squamous intraepithelial lesions and cervical cancer. This study evaluates the association between the type of vaginal microbiota and the occurrence of high-grade squamous intraepithelial lesions of the cervix.
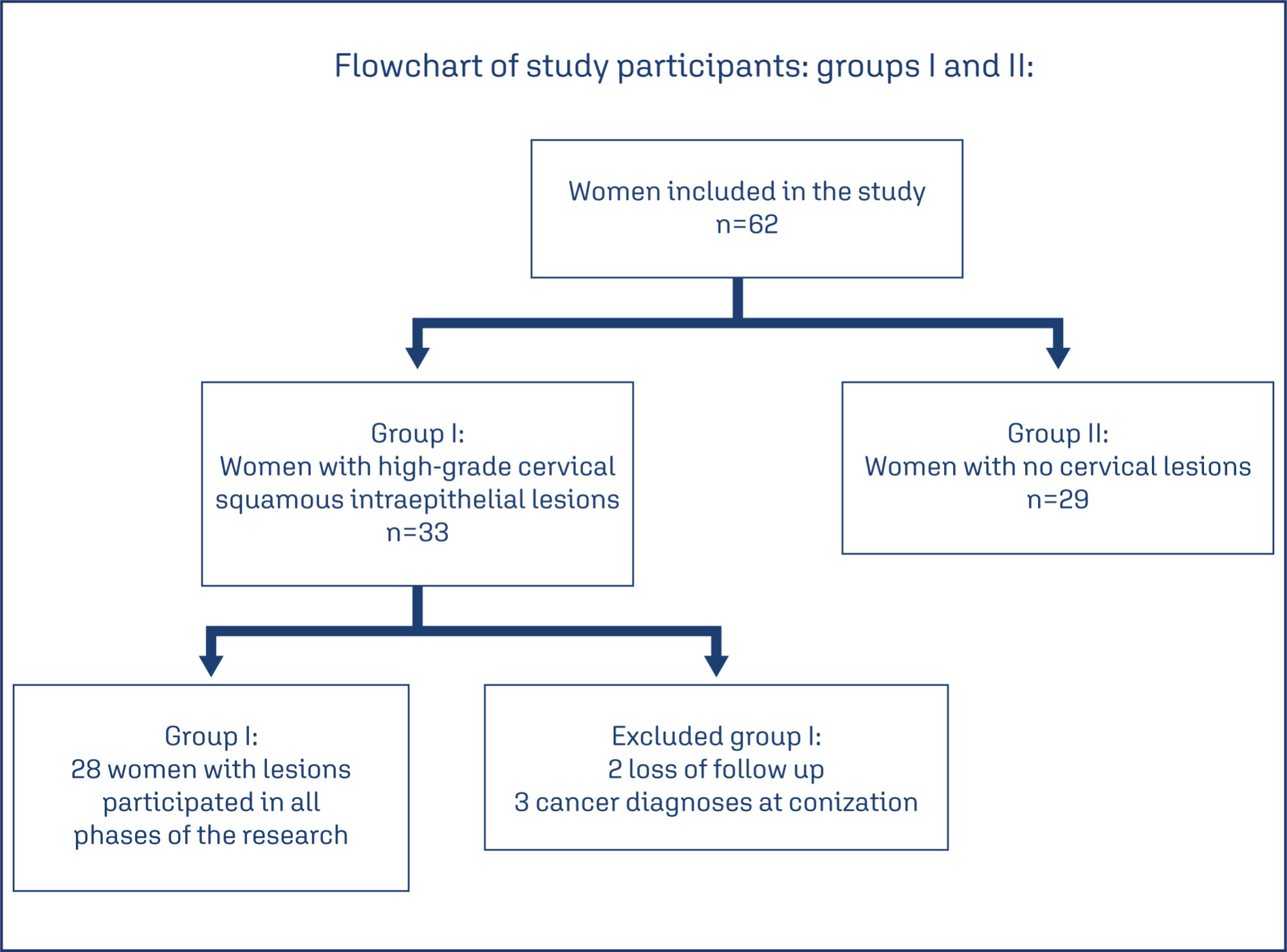
Observational, longitudinal, prospective, and analytical studies carried out between 2019 and 2021, which evaluated the vaginal microbiota of patients diagnosed with high-grade cervical squamous intraepithelial lesion before and after treatment in two collections with an interval of 6 months, using scrapings and vaginal swabs.
In Group I (with lesions) 28 women participated and 29 in Group II (without lesions). According to Nugent, in the initial collection of Group I, 16 women (57%) had lactobacillary microbiota, eight (28%) intermediate, and four (14%) coccus. In Group II, twenty-one (75%) were lactobacillary, one (3%) was intermediate, and seven (24%) werecoccus. With p=0.03.
According to Nugent's criteria, there was an association between the type of vaginal microbiota and the occurrence of high-grade cervical squamous intraepithelial lesions of the cervix. The same was not observed in the Donders classification. Studies with a larger sample are needed to confirm our results.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):689-698
The present study aims to establish a risk profile for high-grade cervical lesions and cervical cancer (CIN2 + ) in women undergoing colposcopy at the Hospital do Câncer de Barretos, through the analysis of Human Papillomavirus (HPV) infection, cervical cytology, and patient's age.
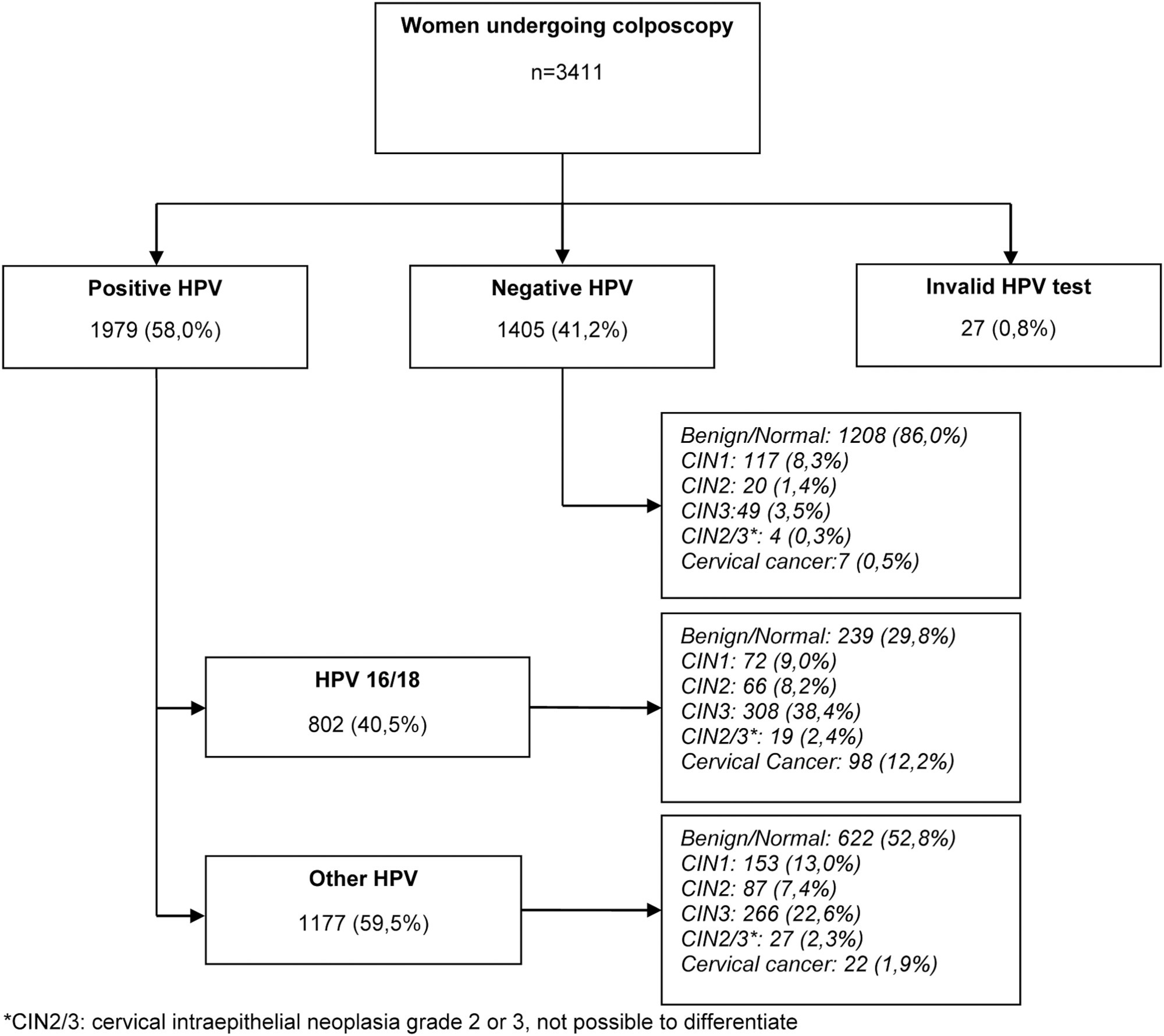
Retrospective cross-sectional study based on a computerized database of women aged ≥ 18 years old who underwent colposcopy at the Prevention Department of the Hospital do Câncer de Barretos from 2017 to 2019.
A total of 3,411 women were included, 58.0% were positive for high-risk-HPV test, with a higher prevalence of CIN2+ for HPV16 (30.3%) and other HPV (45.0%). Cytological findings that suggest invasive cervical cancer (squamous cells or adenocarcinoma), regardless of the status of HPV test, showed 100% diagnosis of CIN2 + , while atypias that suggest high-grade lesions, HSIL and ASC-H, positive for HPV test, showed in 86 and 55.2%, respectively, diagnosis of CIN2 + . ASC-H cytological results among women aged > 40 years old and negative HPV were mainly associated with benign findings. We observed that ≤ CIN1 has a higher prevalence among older women with negative HPV, while for high-grade lesions there is an increase among young women HPV16- and/or 18-positive. In cancer diagnosis, we observed a predominance of HPV 16/18 regardless of the age group.
The highest risks of precursor lesions and cervical cancer were found among women with positive HPV 16/18 tests and severe cytological atypia in population screening tests. In addition, cytological findings of ASC-H HPV negative in women > 40 years old usually represent benign findings in histological investigation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):21-30
To evaluate the rates of precancerous lesions, colposcopy referral, and positive predictive value (PPV) by age groups of a population-based screening with DNA-HPV testing.
The present demonstration study compared 16,384 HPV tests performed in the first 30 months of the program with 19,992 women tested in the cytology screening. The colposcopy referral rate and PPV for CIN2+ and CIN3+ by age group and screening program were compared. The statistical analysis used the chi-squared test and odds ratio (OR) with 95% confidence interval (95%CI).
The HPV tests were 3.26% positive for HPV16-HPV18 and 9.92% positive for 12 other HPVs with a 3.7 times higher colposcopy referral rate than the cytology program, which had 1.68% abnormalities. Human Papillomavirus testing detected 103 CIN2, 89 CIN3, and one AIS, compared with 24 CIN2 and 54 CIN3 detected by cytology (p < 0.0001). The age group between 25 and 29 years old screened by HPV testing had 2.4 to 3.0 times more positivity, 13.0% colposcopy referral, twice more than women aged 30 to 39 years old (7.7%; p < 0.0001), and detected 20 CIN3 and 3 early-stage cancer versus 9 CIN3 and no cancer by cytology screening (CIN3 OR= 2.10; 95%CI: 0.91 -5.25; p = 0.043). The PPV of colposcopy for CIN2+ ranged from 29.5 to 41.0% in the HPV testing program.
There was a significant increase in detections of cervix precancerous lesions in a short period of screening with HPV testing. In women < 30 years old, the HPV testing exhibited more positivity, high colposcopy referral rate, similar colposcopy PPV to older women, and more detection of HSIL and early-stage cervical cancer.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):211-217
To reveal the changes in the quality of life reported by women with Human papillomavirus (HPV)-induced lesions.
This is a cross-sectional, descriptive-exploratory study of a qualitative approach performed from June to August 2016. Semi-structured face-to-face interviews based on five questions on the concept of quality of life were used. The data were submitted to thematic analysis. All ethical aspects have been contemplated.
A total of 20 women aged between 25 and 59 years old were interviewed. From the analysis of the data, the following thematic units emerged: physical and emotional changes, especially complaints of pruritus, discharge and pain, worry, fear, shame and sadness; changes in sexual and affective relationships with decreased libido, dyspareunia and interruption of sexual activity; changes in social relationships resulting in absenteeism at work.
Human papillomavirus infection impairs the quality of life of women as it significantly affects sexual, affective, physical, emotional, and everyday habits. Therefore, HPV infection can lead to exponential changes in the quality of life of women, which can be mitigated by the availability of sources of support such as family, friends and the multi-professional team, helping to improve knowledge and cope with HPV.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):540-546
To determine the frequency of sexually transmitted infections (STIs) in asymptomatic women and the association of STIs with cervical intraepithelial neoplasia (CIN).
A cross-sectional studywas performed, enrollingwomen examined in a general gynecology clinic and in a colposcopy referral center fromOctober 2014 to October 2015. The colposcopy groupconsisted of 71women, and the general gynecologygroupconsisted of 55 women. Cervical samples were collected for cervical cytology and a multiplex realtime polymerase chain reaction (PCR) was developed to detect human papillomavirus (HPV) and the STIs caused by the following microorganisms: Chlamydia trachomatis, Mycoplasma hominis, Mycoplasma genitalium, Ureaplasma urealyticum, and Neisseria gonorrhoeae. A multivariate analysis was performed by logistic regression, considering the significance level of 0.05.
The general frequency of STIs was: 46.8% (HPV); 27.8% (C. trachomatis); 28.6% (M. genitalium); 0.8% (M. hominis); 4.8% (U. urealyticum); and 4.8% (N. gonorrhoeae). The significant risk factors for CIN were: HPV infection (odds ratio [OR] = 2.53; p = 0.024); C. trachomatis (OR = 3.04; p = 0.009); M. genitalium (OR = 2.37; p = 0.04); and HPV and C. trachomatis coinfection (OR = 3.11; p = 0.023). After the multivariate analysis, a significant associationwas found betweenHPVand CIN(OR = 2.48; 95% confidence interval [95%CI]: 1.04-5.92; p = 0.04); and between C. trachomatis and CIN (OR = 2.69; 95%CI: 1.11-6.53; p = 0.028).
The frequency of STIs was high in asymptomatic patients. Infections by HPV and C. trachomatis were independently associated with the presence of CIN. The high frequency of STIs in asymptomatic women suggests the need for routine screening of these infections.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):231-238
To evaluate the incidence and factors associated with cervical intraepithelial neoplasia (CIN) and cervical infection by human papillomavirus (HPV) among HIV-positive and HIV-negative women.
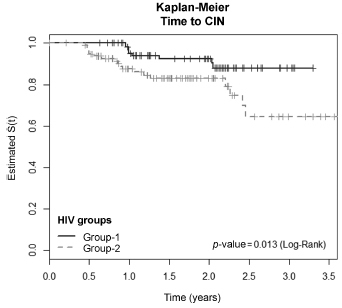
A cohort of 103 HIV positive and 113 HIV negative women were monitored between October 2008 and February 2012, for at least one year. Procedures included cervical cytology, DNA/HPV detection by polymerase chain reaction, colposcopy with biopsy if necessary, followed by an interview for exposure characteristics data. CIN was based on the histopathological results.
The incidence of CIN was of 8.8 and 4.6 cases/100 women-years in HIVpositive and HIV-negative women, respectively. HIV-positive women presented a hazard ratio (HR) of 2.8 for CIN and developed lesions earlier (0.86 year) than HIVnegative women (2 years) (p = 0.01). The risk of developing CIN decreased with age (HR = 0.9) and marital status (HR = 0.4). HPV patients presented a higher incidence of CIN when compared HIV-positive and HIV-negative women (p = 0.01). The incidence of HPV cervical infection was 18.1 and 11.4 cases/100 women-years in HIV-positive and HIV-negative women, respectively. Those HIV-positive presented earlier HPV infection (p = 0.002). The risk of developing HPV infection decreased with age and was higher among HIV-positive women. HPV 16 was the most common type in HIV-positive women, and also the type most closely associated with CIN in HIV-negative women.
HIV-positive women had a greater incidence of HPV and CIN, and in a shorter time interval. More rigorous and timely clinical control is required for this group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):178-185
DOI 10.1590/SO100-720320150005184
To conduct a comparative study between two groups of women (HIV positive and negative) analyzing: the prevalence of cervical intraepithelial neoplasia (CIN) and cervical HPV infection; viral risk and relationship with development of CIN; and sociodemographic and behavioral parameters that influence cervical HPV infection and the development of CIN.
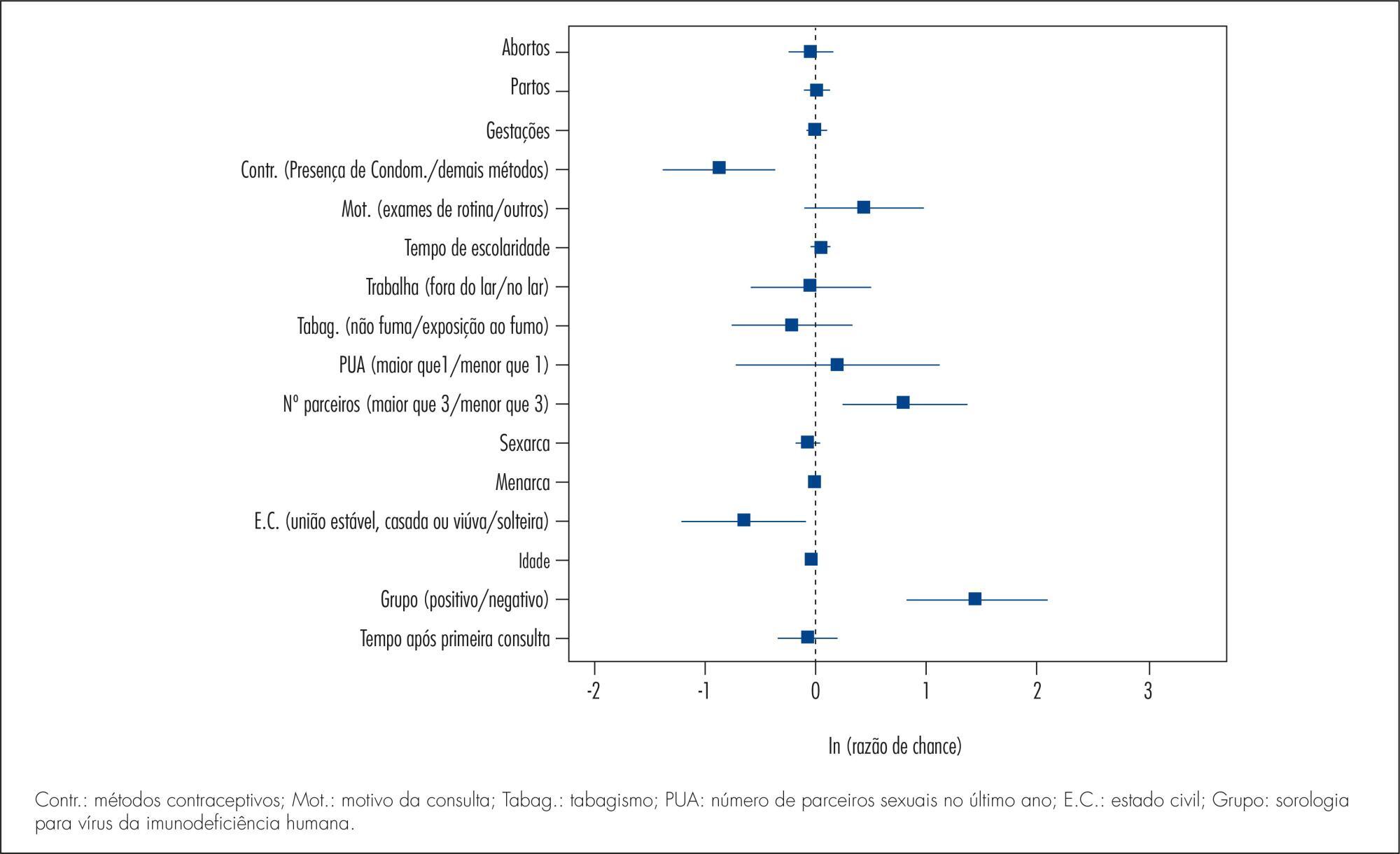
A cross-sectional study in which 202 HIV-positive women and 164 HIV-negative women were analyzed to assess the prevalence of CIN and 171 HIV-positive women and 160 HIV-negative women were analyzed to assess the prevalence of cervical HPV infection. The following procedures were performed on the occasion of each medical visit: collection of cervical samples for cytology and polymerase chain reaction (PCR) to detect HPV DNA; colposcopy; standardized questionnaire to collect demographic and behavioral data; and biopsy of all colposcopic changes. Histopathology was the gold standard for the diagnosis of CIN.
The prevalence of CIN was 2.4 and 15.3% (p<0.001) and the prevalence of cervical HPV infection was 37.1 and 55.5% (p=0.002), respectively, among HIV-negative and -positive women. HIV-positive women had a higher risk of HPV infection (35.7 and 23.6%) (p=0.02). HPV 16 was the most prevalent virus type, occurring in 11.3 and 10.2% of HIV-positive and negative women and was also more prevalent among women presenting CIN in both groups. Factors associated fwith the development of CIN were: HIV infection (HT=4.64; 95%CI 2.23-9.65), age (HT=0.95; 95%CI 0.93-0.98 for each year of life) and marital status(HT=0.49; 95%CI 0.30-0.80). Associated factors for HPV infection were: HIV presence (HT=2.72; 95%CI 1.77-4.17), greater number of sexual partners (HT=1.87; 95%CI 1.23-2.84), age (HT=0.97; 95%CI 0.95-0.99 for each year of life) and marital status (HT=0.65; 95%CI 0.42-1.0 for stable union/widows).
The prevalence of CIN and cervical HPV infection was higher in HIV-positive women, who also presented a higher risk of HPV infections and multiple viral types. Type 16 was predominant in both groups and in women with CIN. Older women and women with stable union/widows were less likely to acquire cervical HPV infection and CIN.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(5):226-232
DOI 10.1590/S0100-72032013000500007
PURPOSE: To determine the HPV prevalence and genotypes and to identify factors associated with infection in pregnant and non-pregnant women with positive or negative HIV-1, treated in Gynecology and Obstetrics Ambulatories and in Health Primary Units, in Rio Grande, Rio Grande do Sul State, Brazil. METHODS: Cervical cells samples from 302 patients were analyzed for HPV presence and genotypes were determined by nested and sequencing polymerase chain reaction. We calculated prevalence ratios associated with the studied variables by Fisher's exact or χ² tests, and Poisson's regression. Women with insufficient material were excluded from the study. RESULTS: HPV was detected in 55 of the 302 women included in the study (18.2%); of these, 31 were pregnant, showing a significant association for HPV (p=0.04) when compared to non-pregnant ones. Risk factors for the infection were: patients aged <20 years-old (p=0.04), early initiation of sexual life (p=0.04), absence of cytological test (p=0.01), diagnosis of altered cytology (p=0.001), and counting <349 cells/mm³ (p=0.05). However, multi-parity was found to be a protective factor for the infection (p=0.01). Multivariate analysis showed that age <20 years-old (PR=2.8; 95%CI 1.0 - 7.7, p=0.04) and an altered cytological result (PR=11.1; 95%CI 3.0 - 4.1, p=0.001) were significantly associated with infection. HPV genotype was determined in 47 samples (85.4%) presenting one genotype per infection: eight HPV 16 and 58; six HPV 6; four HPV 18 and 33; three HPV 53 and 82; two HPV 83 and 61; one HPV 31, 35, 45, 64, 68, 71 and 85. CONCLUSIONS: The prevalence of HPV detection was 18.2%, the most frequent genotypes were 16 and 58, and sociodemographic and gynecological factors were associated with viral infection.