Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo9
To analyze the amount of muscle and the presence of sarcopenia in postmenopausal women using different methods, verifying the agreement between them as to skeletal muscle mass (SMM).
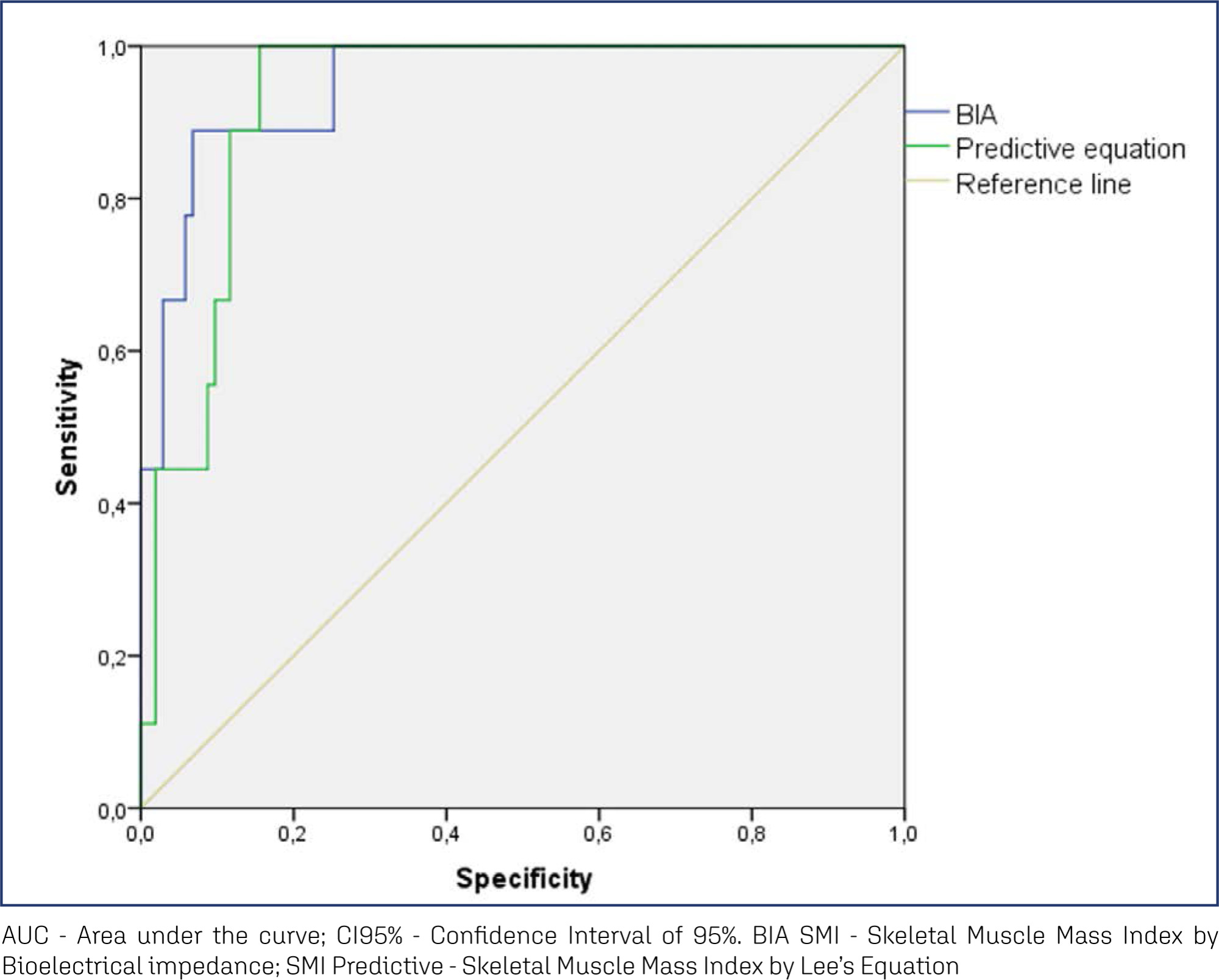
This cross-sectional observational study was conducted with postmenopausal women aged ≥ 50 years. SMM was obtained from a predictive equation, Bioelectrical Impedance (BIA), and Dual Energy X-Ray Absorptiometry (DXA). The skeletal muscle mass index (SMI) and the appendicular skeletal muscle mass index (ASMI) were calculated. The cut-off point of SMI was determined for the population itself. The agreement between the SMI obtained using the different methods was verified. Sarcopenia was diagnosed according to the criteria proposed by the European Working Group on Sarcopenia in Older People 2 (EWGSOP2). The significance level adopted for all tests was 5.0%.
A total of 112 women were evaluated, with an average age of 66.1 ± 5.65 years. Among them, 51.8% were sufficiently active and 43.8% were overweight and obese. The SMI cut-offs were 6.46 kg/m2 for the predictive equation and 7.66 kg/m2 for BIA, with high sensitivity and specificity. There was an excellent agreement in the identification of SMM by the predictive equation (0.89 [0.824-0.917], p < 0.001) and BIA (0.92 [0.883-0.945], p < 0.001), in reference to DXA. The prevalence of sarcopenia was 0.9%, 1.8%, and 2.7% according to BIA, DXA, and the predictive equation, respectively.
The predictive equation showed the expected agreement in estimating skeletal muscle mass in postmenopausal women, offering a viable and accurate alternative.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):586-592
To determine if there is a correlation between body mass index (BMI) and climacteric symptoms in postmenopausal women.
The study sample was composed of 109 postmenopausal women with a mean age of 57 ± 8 years, mean body mass index (BMI) of 30 ± 6 kg/m2, and 8 ± 8 years after menopause. For the assessment of the climacteric symptoms, the Blatt-Kupperman Index (BKI), the Menopause Rating Scale (MRS), and the Cervantes Scale (CS) were used. Data analysis was performed through the Chi-squared test, analysis of variance (ANOVA) with the Bonferroni post hoc test, and multiple linear regression. The level of significance adopted was of p < 0.05. The statistical analyses were performed using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, United States) software, version 26.0.
The multiple linear regression showed a positive association (p<0.01) between BMI values and menopause symptoms when adjusted for age and time after menopause in the 3 questionnaires used (BKI: B = 0.432; CS: B = 304; and MRS: B = 302). Regarding symptom scores, the obese women had higher mean scores (p<0.05) when compared to eutrophic women (BKI = 28 ± 10 and 20 ± 10; and MRS = 20 ± 10 and 13±7, respectively). In the Chi-squared analysis, 28% of obese women had severe symptoms and 46% had moderate symptoms, while only 1% and 46% of eutrophic women had these same symptoms.
There is an association between BMI and climacteric symptoms, and overweight or obese women have more intense and moderate symptoms than eutrophic women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):834-839
It has been suggested that excess body weight could represent a risk factor for infertility outcomes. The present study aimed to evaluate the association of overweight and anovulation among infertile women with regular menstrual cycles.
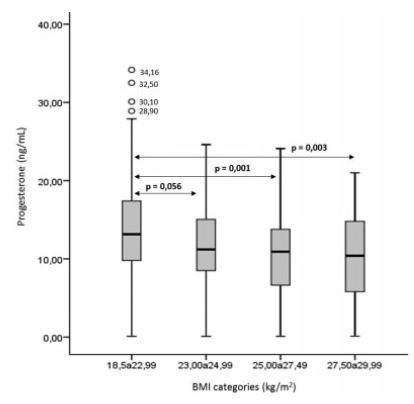
We conducted a retrospective case-control study with consistently anovulatory patients undergoing assisted reproduction treatment. The patients were stratified into normal weight (body mass index [BMI]: 18.5-24.9kg/m2) and overweight (BMI: 25.0- 29.9kg/m2).Those with polycystic ovary syndrome or obesity were excluded. The groups were matched for age, duration of infertility, prolactin, follicle stimulating hormone (FSH), thydroid stimulating hormone (TSH), luteinizing hormone (LH), and estradiol levels.
Overweight was significantly associated with anovulation, when using the World Health Organization (WHO) criteria for anovulation: progesterone levels>5.65 ng/ml and ultrasonography evidence of follicle collapse (odds ratio [OR]: 2.69; 95% confidence interval [CI95%]: 1.04-6.98).
Body mass index above the normal range jeopardizes ovulation among non-obese infertile women with regular menstrual cycles.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):107-112
To evaluate the obstetric and sociodemographic characteristics of gestational diabetic women who maintained hyperglycemia in the postpartum period (6-12 weeks postpartum).
This is a longitudinal cohort study with women who have had gestational diabetes and/or macrosomic children between March 1st, 2016 and March 1st, 2017. Between 6 and 12 weeks after birth, women who had gestational diabetes collected fasting glycemia, glucose tolerance test, and glycated hemoglobin results. The data were collected from medical records and during an interview in the first postpartum consultation. A statistical analysis was performed using frequency, percentage, Chi- Squared test, Fisher exact test, Mann-Whitney test, and multivariate Poisson regression. The significance level adopted for the statistical tests was 5%.
One hundred and twenty-two women were included. Most of the women were younger than 35 years old (70.5%), white, multiparous, and with no history of gestational diabetes. Thirteen percent of the participants developed persistent hyperglycemia. A univariate analysis showed that maternal age above 35 years, being overweight, having grade 1 obesity and weight gain under 5 kg was related to the persistence of hyperglycemia in the postpartum period.
Maternal age above 35 years, obesity and overweight, and the diagnosis of gestational diabetes in the first trimester of pregnancy are associated with hyperglycemia during the postpartum period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(12):578-584
DOI 10.1590/SO100-720320150005445
To estimate the future pregnancy success rate in women with a history of recurrent pregnancy loss.
A retrospective cohort study including 103 women seen at a clinic for recurrent pregnancy loss (loss group) between January 2006 and December 2010 and a control group including 204 pregnant women seen at a low-risk prenatal care unit between May 2007 and April 2008. Both groups were seen in the university teaching hospital the Maternidade Climério de Oliveira, Salvador, Bahia, Brazil. Reproductive success rate was defined as an alive-birth, independent of gestational age at birth and survival after the neonatal period. Continuous variables Means and standard deviations (SD) were compared using Student's t-test and nominal variables proportions by Pearson χ2test.
Out of 90 who conceived, 83 (91.2%) had reproductive success rate. There were more full-term pregnancies in the control than in the loss group (174/187; 92.1 versus 51/90; 56.7%; p<0.01). The prenatal visits number was satisfactory for 76 (85.4%) women in the loss group and 125 (61.3%) in the control (p<0.01). In this, the beginning of prenatal care was earlier (13.3; 4.2 versus 19.6; 6.9 weeks). During pregnancy, the loss group women increased the weight more than those in the control group (58.1 versus 46.6%; p=0.04). Although cervix cerclage was performed in 32/90 women in the loss group, the pregnancy duration mean was smaller (34.8 weeks; SD=5.6 versus 39.3 weeks; SD=1.6; p<0.01) than in the control group. Due to gestational complications, cesarean delivery predominated in the loss group (55/83; 64.7 versus 73/183; 39.5%; p<0.01).
A very good reproductive success rate can be attributed to greater availability of healthcare services to receive pregnant women, through prenatal visits (scheduled or not), cervical cerclage performed on time, and available hospital care for the mother and newborn.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(8):359-365
DOI 10.1590/SO100-720320150005415
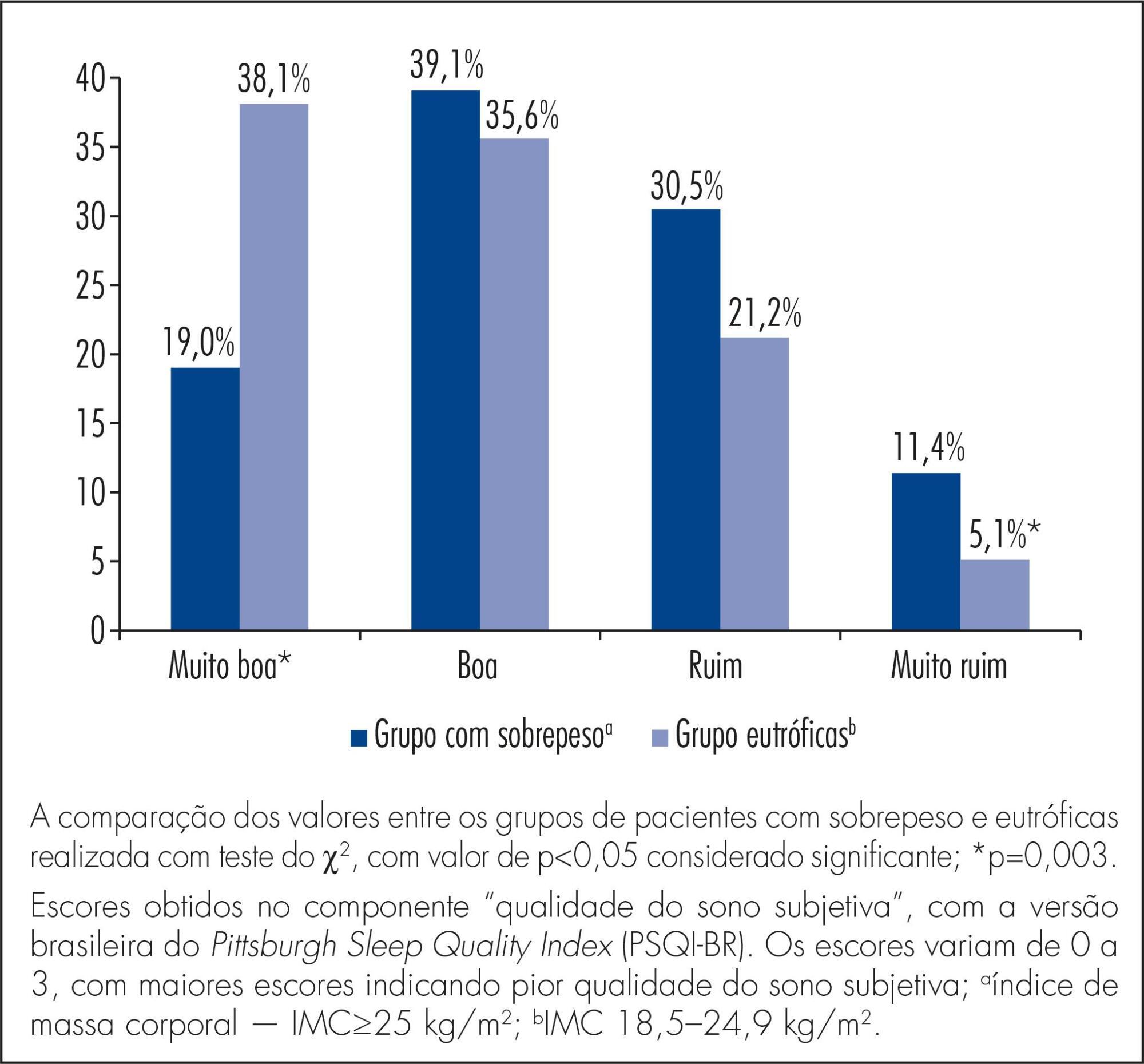
To compare sleep quality of overweight versus normal weight women in the second and third trimesters of pregnancy.
A cross-sectional study involving 223 women with 14 or more weeks of pregnancy, 105 of them overweight (pre-pregnancy body mass index - BMI - ≥25.0 kg/m2) and 118 of normal weight (BMI 18.5-24.9 kg/m2), attending the prenatal care clinic. The Brazilian version of the Pittsburgh Sleep Quality Index (PSQI-BR) questionnaire was used to evaluate sleep quality. The Student t-test and the chi-square test were used to compare differences between groups and a p value <0.05 was considered statistically significant.
Most of the participants (67.7%) were poor sleepers (total score >5); this proportion was significantly higher among overweight (80/105) versus normal weight (67/118) women (76.2 versus 56.8%, p=0,004). During the second trimester, this difference did not reach statistical significance (72.5 versus 53.7%, respectively, p=0.06) but mean total PSQI-BR scores were significantly higher among overweight participants (7.0±3.8 versus 5.5±3.2, p=0.02). In the 2nd trimester, overweight women also had higher scores for sleep latency (1.4±1.0 versus 1.0±0.9, p=0.02) and subjective sleep quality (1.3±0.8 versus 0.8±0.8, p=0.02). In the third trimester, the proportion of women with poor sleep quality was significantly higher in the overweight group, but did not reach statistical significance (79.6 versus 60.8%, p=0.06). During this period, total mean scores were similar for women with and without excess weight (9.4±4.2 versus 8.3±4.6, p=0.2). However, overweight women had higher mean scores for sleep disturbance (2.3±0.7 versus 2.0±0.8, p=0.04).
Overweight women had a poorer sleep quality than normal weight women in the second and third trimesters of pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):514-518
DOI 10.1590/S0100-720320140005007
To describe the epidemiologic and obstetric characteristics of women with recurrent miscarriages.
A descriptive and analytical study whose inclusion criterion was every woman that was attended at the clinic for recurrent miscarriage (loss group), between January 2006 and December 2010. Patients that did not live in Salvador, Bahia, Brazil, and those who were not reached by telephone or whose number was not included in the medical record were not included. The Control Group consisted of 204 pregnant women seen at the low-risk prenatal care unit between May 2007 and April 2008. Women who did not accept to be interviewed and those with obstetric risk were excluded from the Control Group. The analyzed variables were: age, education, occupation, marital status, alcohol consumption, body mass index, obstetric history and the gestational age when the losses occurred. The SPSS 18.0 program was used for statistical analysis. Means and standard deviations of continuous variables were compared using the Student's t-test and the frequencies of the nominal variables were compared by the χ2 test.
The mean age of women in the loss group was higher than in the Control Group (32.3±6.3 versus 26.5±6.4 years old, p<0.01). Consumption of alcoholic beverages predominated in the loss group (36.9 versus 22.1%, p=0.01), as well as marital status (93.2 versus 66.7% were married or living in a stable union, p<0.01). The pre-pregnancy body mass index was higher in the loss group (26.9 versus 23.5%, p<0.01). Regarding obstetric history, 103 women with recurrent miscarriage reported 334 pregnancies. Fifty-six of them had 2 or more miscarriages in the first quarter and in 31 of them, 2 or more pregnancies progressed to late abortions/extremely preterm infants.
Some risk factors were identified in women with recurrent losses, such as more advanced age and higher body mass index. These observations agree with more recent proposals regarding recurrent losses that consider the inclusion of losses in various gestational ages.