Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):503-508
DOI 10.1590/S0100-720320140005081
To evaluate variations in the body mass index in patients undergoing adjuvant chemotherapy for breast cancer, and to associate these changes with patient's age and adjuvant chemotherapy regimen.
We performed a retrospective cohort study in order to correlate any variation in the body mass index before and after adjuvant chemotherapy with patient's age and adjuvant chemotherapy regimen. Patients who received any form of prior hormone therapy, such as tamoxifen or aromatase inhibitors, were excluded. We selected data for 196 patients with stage I to III breast cancer who were treated by radical or conservative surgery and received adjuvant chemotherapy at the Cancer Institute of the State of São Paulo, Brazil.
Before adjuvant chemotherapy, 67.8% of patients were classified as overweight or obese according to their body mass indices. Around 66.3% (95% CI 59.7–73.0) of the patients exhibited an increase in the body mass index after adjuvant chemotherapy. The average age of all patients was 56.3±11.3 years. Participants whose body mass index increased were younger than those with no increase (54.7±11.1 versus 59.3±11.2 years; p=0.007). Patients were treated with the following adjuvant chemotherapy regimens: doxorubicin, cyclophosphamide, and paclitaxel (AC-T, 129 patients, 65.8%); 5-fluoracil, doxorubicin, and cyclophosphamide (36 patients, 18.4%); cyclophosphamide, methotrexate, and 5-fluoracil (16 patients, 8.2%); docetaxel and cyclophosphamide (7 patients, 3.6%); and other regimen (8 patients, 4.1%). The AC-T regimen showed a statistically significant association with increase in the body mass index (p<0.001 by ANOVA).
Most patients with breast cancer showed an increase in the body mass index after adjuvant chemotherapy, especially after the AC-T chemotherapy regimen.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):102-106
DOI 10.1590/S0100-72032012000300002
PURPOSE: To assess the prevalence of obstetric risk factors and their association with unfavorable outcomes for the mother and fetus. METHODS: A longitudinal, descriptive and analytical study was conducted on 204 pregnant women between May 2007 and December 2008. Clinical and laboratory assessments followed routine protocols. Risk factors included socio-demographic aspects; family, personal and obstetric history; high pre-gestational body mass index (BMI); excessive gestational weight gain and anemia. Adverse outcomes included pre-eclampsia (4.5%), gestational diabetes mellitus (3.4%), premature birth (4.4%), caesarian birth (40.1%), high birth weight (9.8%) and low birth weight (13.8%). RESULTS: The average age was 26±6.4 years; the mothers were predominantly non-white (84.8%), 51.8% had incomplete or complete secondary level schooling, 67.2% were in a stable marital relationship and 51.0% had a regular paid job; 63.7% were admitted to the prenatal clinic during the second trimester and 16.7% during the first, with 42.6% being primiparous. A past history of chronic hypertension was reported by 2.9%, pre-eclampsia by 9.8%, excessive gestational weight gain by 15.2% and former gestational diabetes mellitus by 1.0%. In the current pregnancy, elevated pre-gestational BMI was found in 34.6%; 45.5% presented with excessive gestational weight gain, 25.3% with anemia and 47.3% with dyslipidemia. Of the 17.5% of cases with altered blood glucose, gestational diabetes mellitus was confirmed in 3.4% and proteinuria occurred in 16.4% of all cases. Adverse maternal fetal outcomes included pre-eclampsia (4.5%), gestational diabetes mellitus (3.4%), premature birth (4.4%), caesarean birth (40.1%) and high and low birth weight (9.8% and 13.8%, respectively). Independent predictors of adverse maternal fetal outcomes were identified by Poisson multivariate regression analysis: pre-gestational BMI>25 kg/m² was a predictor for pre-eclampsia (RR=17.17; 95%CI 2.14-137.46) and caesarian operation (RR=1.79; 95%CI 1.13-2.85), previous caesarean was a predictor for present caesarean operation (RR=2.28; 95%CI 1.32-3.92) and anemia and high gestational weight gain were predictors for high birth weight (RR=3.38; 95%CI 1.41-8.14 and RR=4.68; 95%CI 1.56-14.01, respectively). CONCLUSION: Pre-gestational overweight/obesity, previous caesarean, excessive weight gain and anemia were major risk factors for pre-eclampsia, caesarean operations and high birth weight.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):348-353
DOI 10.1590/S0100-72032011001100005
PURPOSE: To describe the obstetric outcome of women with overweight/obesity treated at the prenatal care clinic of a public maternity hospital in Rio de Janeiro. METHODS: A descriptive cross-sectional study which investigated 433 women (³20 years-old, without any chronic diseases) and their newborns treated at public hospitals in Rio de Janeiro. Information was collected from medical records and through interviews. The characteristics of mothers and newborns evaluated were divided into maternal (social habits, anthropometric measurements and clinical, obstetric, and prenatal care) and newborn groups (birth conditions). Data regarding the categories of nutritional status were analyzed using the odds ratio (OR) and 95% confidence interval (CI). RESULTS: The prevalence of overweight/obesity in this sample was 24.5% (n=106). There was an association between inadequate weight gain and the prevalence of overweight/obesity (OR 2.7, 95%CI 1.5-4.9, p<0.05). Overweight/obese women had an increased risk for preeclampsia (OR 3.3, 95%CI 1.1--9.9, p=0.03). Regarding birth conditions, mean birth weight was 3291.3 g (±455.2), with rates of low birth weight of 4.7% (n=5) and rates of macrosomia of 2.8% (n=3). CONCLUSIONS: There was an alarming prevalence of inadequate nutritional status before and during pregnancy, which may be associated with increased risk of perinatal morbidity and mortality. This suggests the need for nutritional monitoring of these pregnant women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(8):380-384
DOI 10.1590/S0100-72032009000800002
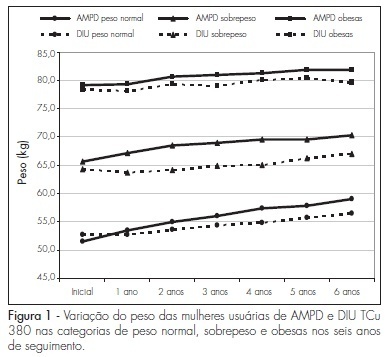
PURPOSE: to determine weight variation in women with different Body Mass Index (BMI) in use of trimestral injections of depot-medroxyprogesterone acetate (DMPA), and compare it to women users of a non-hormonal method. METHODS: retrospective study with the chart review of 226 DMPA users and 603 controls, users of DIU TCu380A. Women were distributed in categories, according to their initial BMI, as having normal weight (<25 kg/m²), overweight (25 to 29,9 kg/m²) and being obese (>30 kg/m²), and were followed-up for six years, with yearly measurements of weight and BMI. The statistic test ANOVA was used to measure the weight variation among the groups in each BMI category every year. RESULTS: the average age at the onset of the method employed was higher in the study group than in the controls, in all the BMI categories: 31.6±SD 7.1 X 27.4±SD 5.5 in the normal weight category (p<0.0001); 37.3±SD 6.8 X 29.2±SD 6.0 in the overweight category (p<0.0001); and 35.3±SD 6.4 X 29.7±SD 5.8 among obese women (p<0.0001). DMPA users showed weight increase as compared to the controls in the overweight category (p=0.0082); and the weight increase along the observation period was also higher among the DMPA users than among the controls, for the normal weight (p<0.0001) and overweight (p=0.0008) categories. In the obese group, there was no BMI variation between the groups, nor along the period during which they were using the method. CONCLUSIONS: there was no change in weight gain among DMPA users from the obese category. Prospective studies should be done with metabolic tests to establish the determining factors of weight gain in normal and overweight women.