-
Original Article05-01-2018
A Long-term Estrogen Deficiency in Ovariectomized Mice is Associated with Disturbances in Fatty Acid Oxidation and Oxidative Stress
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):251-259
Abstract
Original ArticleA Long-term Estrogen Deficiency in Ovariectomized Mice is Associated with Disturbances in Fatty Acid Oxidation and Oxidative Stress
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):251-259
Views245See moreAbstract
Objective
The aim of this work was to evaluate the changes caused by estrogen deficiency in lipid metabolism.
Methods
This study encompassed direct measurements of plasma biochemical analyses, liver lipid contents, and assessments of the mitochondrial β-oxidation capacity as well as an evaluation of the liver redox status in an animal model of estrogen deficiency.
Results
When compared with control mice, the livers of ovariectomized (OVX) mice presented considerable accretions in their lipid contents, which were accompanied by increased levels of lipid peroxidation in liver homogenates andmitochondria from OVX groups and decreased reduced glutathione (GSH) contents. In isolated mitochondria, estrogen deficiency inhibited mitochondrial β-oxidation of fatty acids irrespective of their chain length. The liver mitochondrial and peroxisomal H2O2 generations in OVX mice were increased. Additionally, the activities of all antioxidant enzymes assessed were decreased.
Conclusion
These data provide one potential explanation for the increased susceptibility to metabolic diseases observed after menopause.
-
Original Article04-01-2018
Effectiveness of Metformin in the Prevention of Gestational Diabetes Mellitus in Obese Pregnant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):180-187
Abstract
Original ArticleEffectiveness of Metformin in the Prevention of Gestational Diabetes Mellitus in Obese Pregnant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):180-187
Views281See moreAbstract
Objective
To assess the effectiveness of metformin in the incidence of gestational diabetes mellitus (GDM) in obese pregnant women attending a public maternity hospital in Joinville, Santa Catarina, Brazil.
Methods
Randomized clinical trial including obese pregnant women with a body mass index (BMI) ≥ 30 kg/m2, divided into two groups (control and metformin). Both groups received guidance regarding diet and physical exercise. The participants were assessed at two moments, the first at enrollment (gestational age ≤ 20) and the second at gestational weeks 24-28. The outcomes assessed were BMI and gestational diabetes mellitus (GDM) diagnosis. The data distribution was assessed with the Friedman test. For all the analytical models, the p-values were considered significant when lower than 0.05. The absolute risk reduction was also estimated.
Results
Overall, 164 pregnant women were assessed and further divided into 82 participants per group. No significant difference was observed in BMI variation between the control and metformin groups (0.9 ± 1.2 versus 1.0 ± 0.9, respectively, p = 0.63). Gestational diabetes mellitus was diagnosed in 15.9% (n = 13) of the patients allocated to the metformin group and 19.5% (n = 16) of those in the control group (p = 0.683). The absolute risk reduction was 3.6 (95% confidence interval 8.0- 15.32) in the group treated with metformin, which was not significant.
Conclusion
Metformin was not effective in reducing BMI and preventing GDM in obese pregnant women.
-
Original Article01-01-2018
Body Mass Index Changes during Pregnancy and Perinatal Outcomes – A Cross-Sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):11-19
Abstract
Original ArticleBody Mass Index Changes during Pregnancy and Perinatal Outcomes – A Cross-Sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):11-19
Views222See moreAbstract
Objective
To evaluate the relation between changes the body mass index (BMI) percentile, reflected in the Atalah curve, and perinatal outcomes.
Methods
A cross-sectional study with 1,279 women was performed. Data regarding gestational weight, sociodemographic characteristics and perinatal outcomes were collected through medical charts, prenatal card and interviews in the postpartum period. Women could be classified according to the Atalah curve in the following categories: low weight, adequateweight, overweight, and obese. The BMIwas calculated at the first and at the last prenatal care visits, and these values were compared.
Results
An increase in the BMI category according to the Atalah classification occurred in 19.9% of pregnant women, and an increase of 3.4, 5.8 and 6.4 points of BMI were found for women respectively classified in the adequate weight, overweight and obese categories at the first prenatal visit. Women with high school education presented a lower chance of increasing their BMI (odds ratio [OR] 0:47 [0.24- 0.95]). Women who evolved with an increase in the the Atalah classification were associated with cesarean section (OR 1.97-2.28), fetalmacrosomia (OR 4.13-12.54) and large for gestational age newborn (OR 2.88-9.83).
Conclusion
Pregnant women who gained enough weight to move up in their BMI classification according to the Atalah curve had a higher chance of cesarean section and macrosomia. Women classified as obese, according to the Atalah curve, at the first prenatal visit had a high chance of cesarean section and delivering a large for gestational age newborn.
-
Short Communication12-01-2017
Nutritional Counseling Promotes Changes in the Dietary Habits of Overweight and Obese Adolescents with Polycystic Ovary Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(12):692-696
Abstract
Short CommunicationNutritional Counseling Promotes Changes in the Dietary Habits of Overweight and Obese Adolescents with Polycystic Ovary Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(12):692-696
Views208See moreAbstract
Objective
To evaluate the effects of nutritional counseling on the dietary habits and anthropometric parameters of overweight and obese adolescentswith polycystic ovary syndrome (PCOS).
Methods
This was a prospective, longitudinal and auto-controlled study. Thirty adolescents aged 13-19 years-old, diagnosed with PCOS received nutritional counseling and were followed-up for 6 months. After the follow-up period, the results were evaluated through body weight, body mass index (BMI) and waist circumference (WC).
Results
Sixty-percent of the adolescents adhered to the nutritional counseling and, of these, 50% lost weight. Adolescents who lost weight changed their dietary habits by adopting hypocaloric diets and eating more meals per day, as per nutritional counseling. The waist circumference (WC) decreased significantly, although the body weight decreased non-significantly after adoption of a hypocaloric diet.
Conclusion
Although there was no significant weight loss, there was a considerable reduction in theWCassociated with hypocaloric diets and with eating a greater number of meals per day.
-
Original Article07-01-2017
Effect of Obesity on Gestational and Perinatal Outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):330-336
Abstract
Original ArticleEffect of Obesity on Gestational and Perinatal Outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):330-336
Views145See moreAbstract
Purpose
To assess the impact of pre-pregnancy obesity (body mass index [BMI] ≥30 kg/m2) on the gestational and perinatal outcomes.
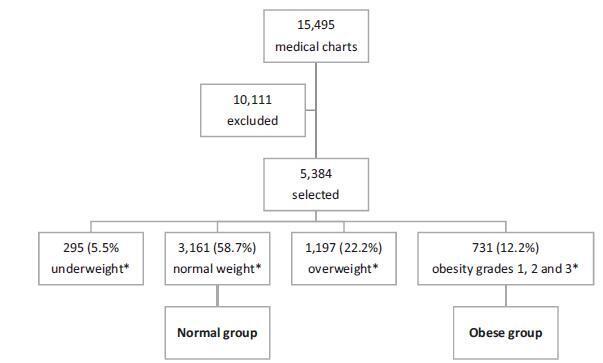
Methods
Retrospective cohort study of 731 pregnant women with a BMI ≥30 kg/m2 at the first prenatal care visit, comparing them with 3,161 women with a BMI between 18.5 kg/m2 and 24.9 kg/m2. Maternal and neonatal variables were assessed. Statistical analyses reporting the demographic features of the pregnant women (obese and normal) were performed with descriptive statistics followed by two-sided independent Student’s t tests for the continuous variables, and the chi-squared (χ2) test, or Fisher’s exact test, for the categorical variables. We performed a multiple linear regression analysis of newborn body weight based on the mother’s BMI, adjusted by maternal age, hyperglycemic disorders, hypertensive disorders, and cesarean deliveries to analyze the relationships among these variables. All analyses were performed with the R (R Foundation for Statistical Computing, Vienna, Austria) for Windows software, version 3.1.0. A value of p < 0.05 was considered statistically significant.
Results
Obesity was associated with older age [OR 9.8 (7.8-12.2); p < 0.01], hyperglycemic disorders [OR 6.5 (4.8-8.9); p < 0.01], hypertensive disorders [OR 7.6 (6.1-9.5); p < 0.01], caesarean deliveries [OR 2.5 (2.1-3.0); p < 0.01], fetal macrosomia [OR 2.9 (2.3-3.6); p < 0.01] and umbilical cord pH [OR 2.1 (1.4-2.9); p < 0.01). Conversely, no association was observed with the duration of labor, bleeding during labor, Apgar scores at 1 and 5 minutes after birth, gestational age, stillbirth and early neonatal mortality, congenital malformations, and maternal and fetal injury.
Conclusion
We observed that pre-pregnancy obesity was associated with maternal age, hyperglycemic disorders, hypertension syndrome, cesarean deliveries, fetal macrosomia, and fetal acidosis.
-
Original Article08-01-2015
Sleep quality in overweight pregnant women
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(8):359-365
Abstract
Original ArticleSleep quality in overweight pregnant women
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(8):359-365
DOI 10.1590/SO100-720320150005415
Views129PURPOSE:
To compare sleep quality of overweight versus normal weight women in the second and third trimesters of pregnancy.
METHODS:
A cross-sectional study involving 223 women with 14 or more weeks of pregnancy, 105 of them overweight (pre-pregnancy body mass index - BMI - ≥25.0 kg/m2) and 118 of normal weight (BMI 18.5-24.9 kg/m2), attending the prenatal care clinic. The Brazilian version of the Pittsburgh Sleep Quality Index (PSQI-BR) questionnaire was used to evaluate sleep quality. The Student t-test and the chi-square test were used to compare differences between groups and a p value <0.05 was considered statistically significant.
RESULTS:
Most of the participants (67.7%) were poor sleepers (total score >5); this proportion was significantly higher among overweight (80/105) versus normal weight (67/118) women (76.2 versus 56.8%, p=0,004). During the second trimester, this difference did not reach statistical significance (72.5 versus 53.7%, respectively, p=0.06) but mean total PSQI-BR scores were significantly higher among overweight participants (7.0±3.8 versus 5.5±3.2, p=0.02). In the 2nd trimester, overweight women also had higher scores for sleep latency (1.4±1.0 versus 1.0±0.9, p=0.02) and subjective sleep quality (1.3±0.8 versus 0.8±0.8, p=0.02). In the third trimester, the proportion of women with poor sleep quality was significantly higher in the overweight group, but did not reach statistical significance (79.6 versus 60.8%, p=0.06). During this period, total mean scores were similar for women with and without excess weight (9.4±4.2 versus 8.3±4.6, p=0.2). However, overweight women had higher mean scores for sleep disturbance (2.3±0.7 versus 2.0±0.8, p=0.04).
CONCLUSION:
Overweight women had a poorer sleep quality than normal weight women in the second and third trimesters of pregnancy.
Key-words ObesityOverweightPregnancy trimester, secondPregnancy trimester, thirdSleepSleep initiation and maintenance disordersSee more -
Original Article07-01-2015
Blockade of AT1 receptor of Angiotensin II reduces the number of antral follicles in female rats with obesity induced by cafeteria diet
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(7):302-307
Abstract
Original ArticleBlockade of AT1 receptor of Angiotensin II reduces the number of antral follicles in female rats with obesity induced by cafeteria diet
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(7):302-307
DOI 10.1590/S0100-720320150005352
Views93See morePURPOSE:
To evaluate the follicular development of female Wistar rats with obesity induced by the cafeteria diet, submitted to the administration of losartan (LOS), an antagonist of the AT1 receptor of Angiotensin II.
METHODS:
At weaning (21 days of age), female Wistar rats were randomly divided, into two groups: control (CTL) that received standard chow and cafeteria (CAF) that received a cafeteria diet, a highly palatable and highly caloric diet. At 70 days of age, at the beginning of the reproductive age, animals of the CAF group were subdivided into two groups (n=15/group): CAF, that received water, and CAF+LOS, that received LOS for 30 days. The CTL group also received water by gavage. At 100 days of age, the animals were euthanized and body weight (BW) as well as the retroperitoneal, perigonadal and subcutaneous fat weights were analyzed. The right ovaries were isolated for counting the number of primary, secondary, antral and mature follicles. Plasma levels of FSH, LH, prolactin and progesterone hormones were analyzed. The results were expressed as mean±standard error of the mean. Data were analyzed statistically by one-way ANOVA followed by the Newman-Keuls post-test (p<0.05).
RESULTS:
BW and fat weight, as well as the number of antral follicles, were higher in the CAF group compared to the CTL group. However, FSH and LH levels were lower in CAF animals compared to CTL animals. LOS administration attenuated the reduction of FSH and LH levels. Progesterone and PRL levels were similar among groups.
CONCLUSION:
LOS could improve follicular development in obese females and could be used as an adjunctive drug in the treatment of infertility associated with obesity.


