Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):384-389
The main objective of this study was to examine the diagnostic performance of the first-trimester combined test for aneuploidies in unselected pregnancies from Rio de Janeiro and compare it with the examples available in the literature.
We investigated 3,639 patients submitted to aneuploidy screening from February 2009 to September 2015. The examination is composed of the Fetal Medicine Foundation risk evaluation based on nuchal translucency evaluation, mother’s age, presence of risk factors, presence of the nasal bone and Doppler of the ductus venous in addition to biochemical analysis of pregnancy-associated plasma protein A (PAPP-A) and beta-human chorionic gonadotropin (β-hCG) markers. The cut-off point for high risk for aneuploidies was defined as greater than 1:100, with intermediate risk defined between 1:100 and 1:1,000, and low risk defined as less than 1:1,000. The variable aneuploidy was considered as a result not only of trisomy of chromosome 21 but also trisomy of chromosomes 13 and 18.
Excluding the losses, the results of 2,748 patients were analyzed. The firsttrimester combined test achieved 71.4% sensitivity with a 7.4% false-positive (FP) rate, specificity of 92.6%, positive predictive value (PPV) of 6.91% and negative predictive value (NPV) of 99.76%, when the cut-off point considered was greater than 1:1,000. Through a receiving operating characteristics (ROC) curve, the cut-off point that maximized the sensitivity and specificity for the diagnosis of aneuploidies was defined as 1:1,860. When we adjusted the false-positive (FP) rate to 5%, the detection rate for this analysis is 72.7%, with a cut-off point of 1:610.
The combined test of aneuploidy screening showed a detection rate inferior to those described in the literature for a higher FP rate.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(6):274-280
DOI 10.1590/S0100-72032013000600007
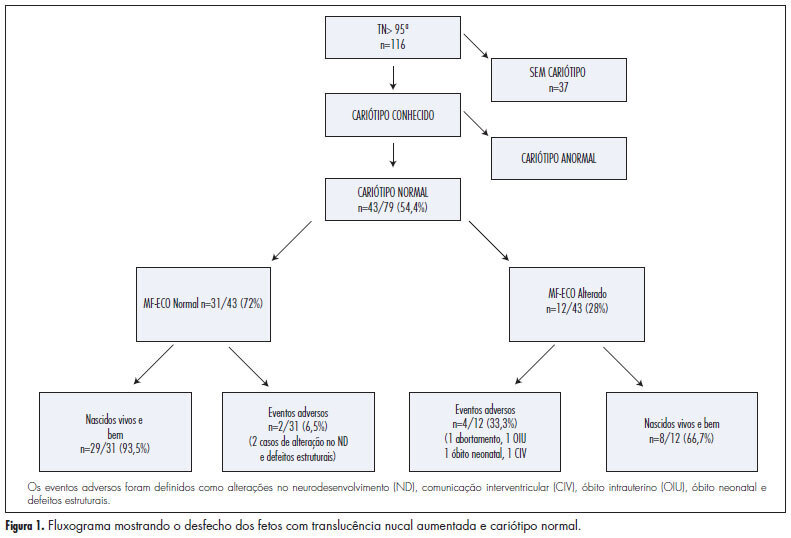
PURPOSE: To analyze the perinatal and pediatric outcome of fetuses that showed nuchal translucency (NT) above the 95th percentile (P95) and a normal karyotype in order to obtain data allowing better maternal prenatal counseling. METHODS: fetuses from a tertiary obstetric service with an NT above P95 and a normal karyotype were analyzed between 2005 and 2011. We analyzed gestational ultrasound follow-up, fetal and postnatal echocardiography (ECHO), weight, length and Apgar score at birth, and neuropsychomotor development by the Ages and Stages Questionnaire (ASQ) up to July 2012. RESULTS: During this period, there were 116 cases of nuchal translucency above the 95th percentile, and the fetal karyotype was determined in 79 of them (68%). Forty-three analyses were normal (54.4%) and 36 were altered (45.6%). Among the fetuses with a normal karyotype, one was miscarried at 15 weeks of gestation with Cantrel pentalogy and one died at 24 weeks with several structural abnormalities. There was one neonatal death of unknown cause and two cases of intraventricular communication (IVC) detected by fetal ECHO. Postnatal echocardiography revealed the persistence of IVC in one case and one case of atrial septal defect (ASD) and patent ductus arteriosus (PDA). Of the 40 surviving children, only 1 showed delayed speech development and another presented autism. The remaining cases resulted in normal neurodevelopment. CONCLUSION: During the monitoring of fetuses with increased NT and a normal karyotype, parents can be best advised that when a 2nd trimester morphological-echocardiography ultrasound study is normal, the probability of the child being born alive and well is high (93.5%).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(6):288-294
DOI 10.1590/S0100-72032011000600005
PURPOSE: to evaluate the performance of the combined first trimester screening for chromosomal abnormalities in a group of the Brazilian population. METHODS: a retrospective study including pregnant women with single fetuses referred to a fetal medicine center to perform the first trimester screening that combines maternal age, nuchal translucency measurement and two maternal serum biochemical markers: free B-hCG and PAPP-A. To evaluate the performance of the test, the detection rate, specificity, negative and positive predicted values and false-positive rates were calculated, considering as high risk the cut-off value above 1 in 300. RESULTS: we studied 456 patients submitted to the test. Advanced maternal age above 35 years was observed in 36.2% of cases. The incidence of chromosomal abnormalities in the study population was 2.2%. Twenty-one patients (4.6%) presented a high risk (above 1:300) by the combined test. Using this cut-off level, the detection rate of the test was 70% for all chromosomal abnormalities and 83.3% for trisomy 21, for a false-positive rate of 3.1%. CONCLUSIONS: the combined first trimester screening was effective to detect chromosomal abnormalities, mainly for trisomy 21, with low false-positive rates. The combined test contributed to decreasing the indication of an invasive test if we compare to maternal age alone as a risk factor.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(1):49-57
DOI 10.1590/S0100-72032011000100008
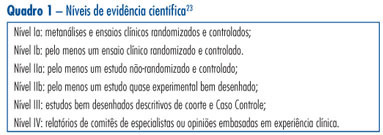
This is a traditional (narrative) review with the objective of highlighting the contribution of obstetric ultrasonography (US) between the 11th and 14th week of pregnancy, commonly called first trimester anomaly scan. In addition to being used for the screening of chromosomal anomalies, US can be employed during this period to confirm or determine gestational age, evaluate fetal anatomy, diagnose malformations, screen major structural abnormalities and genetic syndromes, define the prognosis of pregnancy, diagnose and characterize multiple pregnancies, and screen preeclampsia and intrauterine growth restriction. The most important studies about this subject published between 1990 and 2010 in the Cochrane and PubMed libraries were included. The selected studies can be classified with scientific levels I to III.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):647-653
DOI 10.1590/S0100-72032007001200008
Screening for major chromosomal abnormalities can be provided in the first trimester of pregnancy. Screening by a combination of fetal nuchal translucency and maternal serum free human chorionic gonadotropin and pregnancy-associated plasma protein-A can identify 90% of fetuses with trisomy 21 and other major chromosomal abnormalities for a false-positive rate of 5%. This is superior to the 30% detection rate achieved by maternal age and 65% by second-trimester maternal serum biochemistry. A further improvement in the effectiveness of first-trimester screening is likely to be achieved by a risk-orientated two-stage approach. In this approach, the patients are subdivided into a high-risk group, requiring invasive testing; a low-risk group, which can be reassured that an abnormality is unlikely, and an intermediate-risk group (risk of 1 in 101 to 1 in 1000), in which further assessment is performed by first-trimester ultrasound examination (for presence/absence of the nasal bone or presence/absence of tricuspid regurgitation or normal/abnormal Doppler velocity waveform in the ductus venosus), and chorionic villus sampling is performed if their adjusted risk becomes 1 in 100 or more. Those performing first-trimester scans should be appropriately trained and their results subjected to external quality assurance. This process was well established by the Fetal Medical Foundation several years ago and is widely accepted internationally.
