Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):728-735
The role of breast milk in the physical and mental health of infants and in the prevention of infant death is widely known. The benefits of breastfeeding for mothers and infants have been proven, but several factors can affect breastfeeding. Childbirth is one of the most influential factors. The present study aimed to investigate the effect of the type of delivery (natural childbirth and cesarean section) on breastfeeding based on the latch, audible swallowing, type of nipple, comfort, hold (LATCH) scoring system.
The present cross-sectional observational study was performed using the census method among women who referred to Afzalipour Hospital for delivery in May 2020; the breastfeeding pattern was completed by observation and the in-case information, by LATCH checklist. Data were analyzed using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, United States) software, version 19.0, analysis of variance (ANOVA), and the Chi-squared statistical test.
Out of a total of 254 deliveries (127 natural childbirths and 127 cesarean deliveries), there was no statistically significant difference between the 2 study groups in terms of age, maternal employment status, and infant weight, but there was a statistically significant relationship between the type of delivery, the maternal level of schooling, and the appearance, pulse, grimace, activity, and respiration (Apgar) score in the first minute. The mean score of breastfeeding patterns among the natural childbirth group (9.33) was higher than that of the cesarean section group (7.21).
The type of delivery affects the mother’s performance during breastfeeding, and mothers submitted to cesarean sections need more support and help in breastfeeding.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):91-96
To analyze the factors associated with the prevalence of exclusive breastfeeding (EBF) for up to six months in mother/infant binomials cared for at a usual-risk maternity hospital.
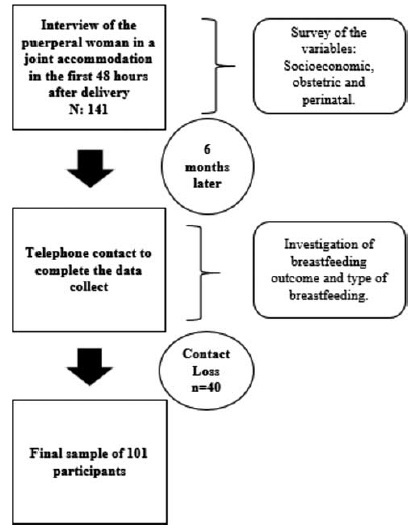
The present is a descriptive, longitudinal, prospective, quantitative study. Socioeconomic, obstetric and perinatal variables from 101 mother/infant binomials in a Public Maternity Hospital in the city of Curitiba, state of Paraná, Brazil, were investigated during hospitalization after delivery and 6 months after birth. For the statistical analysis, the Chi-squared test was used. The variables that showed values of p < 0.25 for the Chi-squared test were also submitted to an odds ratio (OR) analysis.
The prevalence (42.6%) of EBF was observed. Most women (93.1%) had had more than 6 prenatal consultations, and the variables maternity leave and support to breastfeeding were associated with EBF. Support to breastfeeding by professionals and family members increased 4-fold the chance of maintenance of EBF (OR = 0.232; 95% confidence intercal [95%CI]: 0.079 to 0.679; p = 0.008). Cracked nipples were the biggest obstacle to breastfeeding, and low milk production was the main responsible factor for weaning.
The encouragement of breastfeeding and the mother’s stay for a longer period with the child contributed to the maintenance of EBF until the sixth month of life of the infant.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):465-470
To describe and evaluate the use of a simple, low-cost, and reproducible simulator for teaching the repair of obstetric anal sphincter injuries (OASIS).
Twenty resident doctors in obstetrics and gynecology and four obstetricians participated in the simulation. A fourth-degree tear model was created using lowcost materials (condom simulating the rectal mucosa, cotton tissue simulating the internal anal sphincter, and bovine meat simulating the external anal sphincter). The simulator was initially assembled with the aid of anatomical photos to study the anatomy and meaning of each component of the model. The laceration was created and repaired, using end-to-end or overlapping application techniques.
The model cost less than R$ 10.00 and was assembled without difficulty, which improved the knowledge of the participants of anatomy and physiology. The sutures of the layers (rectal mucosa, internal sphincter, and external sphincter) were performed in keeping with the surgical technique. All participants were satisfied with the simulation and felt it improved their knowledge and skills. Between 3 and 6 months after the training, 7 participants witnessed severe lacerations in their practice and reported that the simulation was useful for surgical correction.
The use of a simulator for repair training in OASIS is affordable (low-cost and easy to perform). The simulation seems to improve the knowledge and surgical skills necessary to repair severe lacerations. Further systematized studies should be performed for evaluation.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(3):156-162
Venous thromboembolism events are important causes of maternal death during pregnancyandthepostpartumperiodworldwide.Are view of the literature with the objective of evaluating venous thromboembolism events in the puerperium according to the route of delivery was performed through a bibliographic survey in the Medline, LILACS and Scielo databases. We observed that patients submitted to cesarean sections present a significantlyhigher riskofdeveloping venousthromboembolismwhencomparedwiththose who undergo spontaneous vaginal delivery. The pathophysiological bases for this difference were explored and described in this review, as well as the indications of prophylaxis and treatment. Doctors and health professionals must be continuously vigilant regarding this condition, since it is associated with high morbidity and mortality.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):325-332
Systematic reviews that evaluate the perineal cryotherapy to reduce pain in the vaginal postpartum are inconclusive.
To evaluate clinical effectiveness of cryotherapy in the management of humanized postpartum perineal pain and vaginal edema.
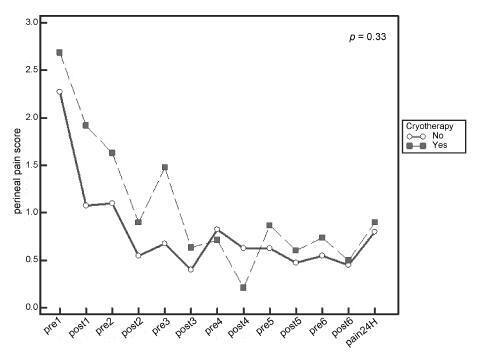
A double-bind randomized controlled clinical trial (UTN number: U1111- 1131-8433) was conducted in a hospital in Northeastern, Brazil.Women were included following humanized childbirth. All had vaginal deliveries of a single, full-term pregnancy with cephalic presentation. Exclusion criteria included previous perineal lesion, episiotomy during the current delivery, instrumental delivery, uterine curettage and postpartum hemorrhage. In the experimental group, an ice pack was applied six times on the perineum for 20 minutes, reducing the temperature between 10 and 15° C, then 60 minutes without exposure to cold. In the non-cryotherapy, a water bag unable to reduce the temperature to this extent was used, compliance with the same application protocol of the first group. Perineal temperature wasmonitored at zero, 10 and 20 minutes for application in both groups. Evaluations were made immediately before and after the applications and 24 hours after delivery spontaneous, to determine the association between variables.
A total of 80 women were included in the study, 40 in each group. There was no significant difference in scores of perineal pain and edema between the groups with or without cryotherapy until 24 hours after childbirth. There was no difference between groups when accomplished repeated measures analysis over the 24 hours after delivery, considering the median perineal pain (p = 0.3) and edema (p = 0.9). Perineal cryotherapy did not influence the amount of analgesics used (p = 0.07) and no adverse effect was registered.
The use of cryotherapy following normal vaginal delivery within the concept of humanized minimally interventionist childbirth had no effect on perineal pain and edema, since it was already substantially lower, nor the need for pain medicaments.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):548-554
DOI 10.1590/So100-720320140005038
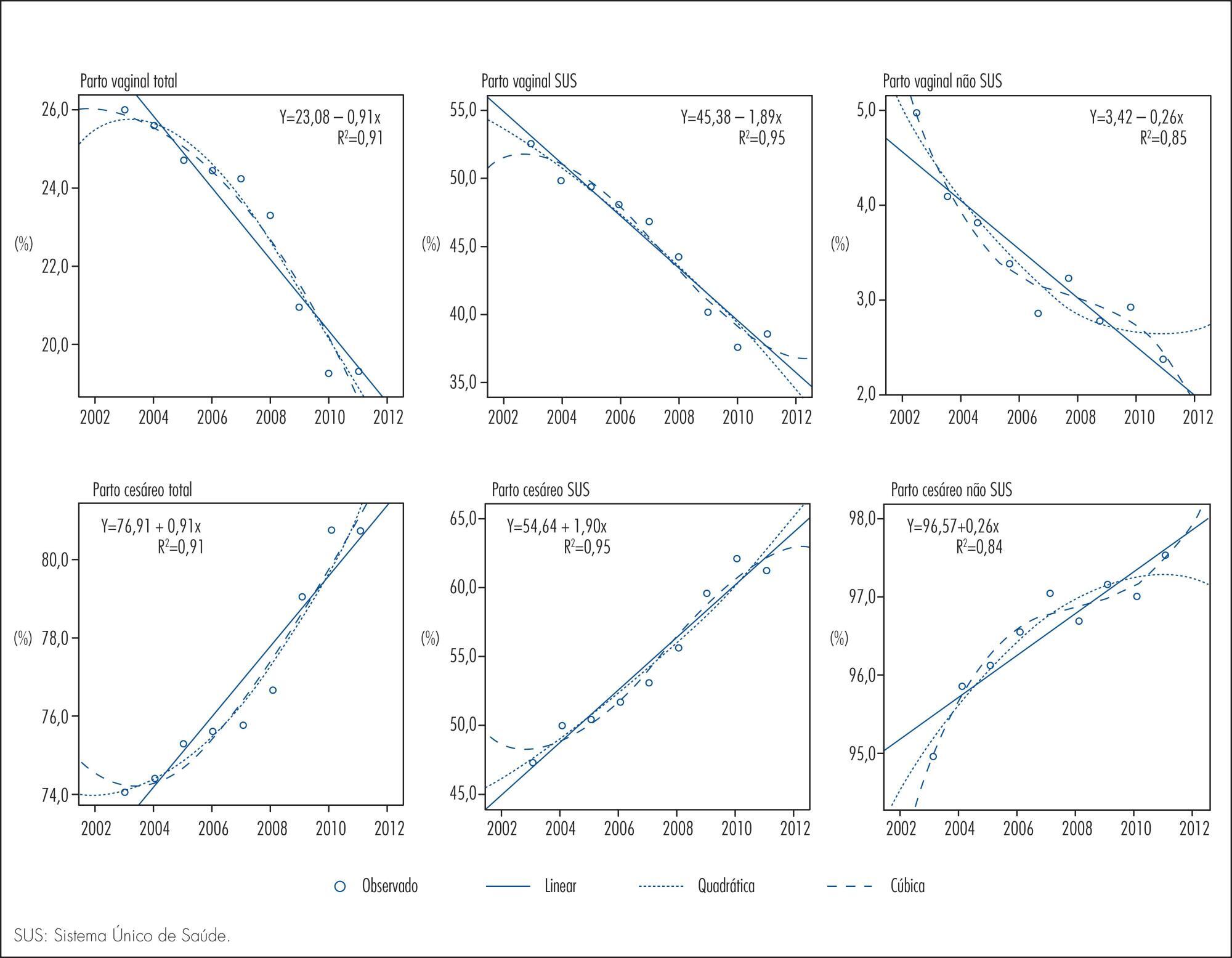
To analyze the time trend of the rates of cesarean and vaginal delivery according to the source of financing.
This was an ecological study of the time series analysis of cesarean and vaginal delivery rates according to the financing source, carried out in Maringá, Paraná State, Brazil, from 2002 to 2012. Information available at the System of Information on Live Births and at the System of Hospital Information of the Brazilian Unified Health System (SUS) was used for data collection. Moving averages were calculated for all mode of delivery rates in order to smooth random fluctuations in the series, dispersion diagrams were designed between the coefficients and years of the study, and polynomial regression models were estimated from the functional relation observed, with the level of significance set at p<0.05.
Throughout the 11 years of the study there were 48,210 births, 77.1% by cesarean delivery and only 22.9% by vaginal delivery. A total of 22,366 procedures were financed by SUS, 54.6% of them being cesareans. Trend analysis was significant for all the regression models, demonstrating an ascending trend for cesarean delivery and a descending trend for vaginal delivery for both types of financing. The non-SUS cesarean rates always exceeded 90.0% and were more frequent than the SUS cesarean rates, even with a 36.0% increase of the latter during the study period.
Based on trend analysis, cesarean deliveries will continue to increase in both health financing sources unless new actions and strategies of reduction are implemented, involving the sociocultural, demographic and obstetric characteristics of women, the training and activity of professionals in the area of obstetrics and an adequate structure of health services for providing vaginal delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(3):117-122
DOI 10.1590/S0100-72032013000300005
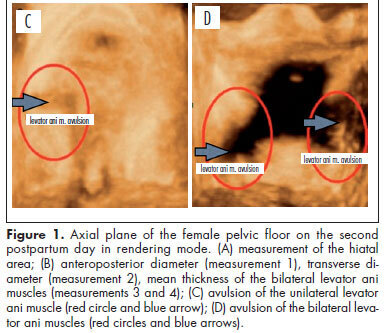
PURPOSE: To evaluate changes to the pelvic floor of primiparous women with different delivery modes, using three-dimensional ultrasound. METHODS: A prospective cross-sectional study on 35 primiparae divided into groups according to the delivery mode: elective cesarean delivery (n=10), vaginal delivery (n=16), and forceps delivery (n=9). Three-dimensional ultrasound on the pelvic floor was performed on the second postpartum day with the patient in a resting position. A convex volumetric transducer (RAB4-8L) was used, in contact with the large labia, with the patient in the gynecological position. Biometric measurements of the urogenital hiatus were taken in the axial plane on images in the rendering mode, in order to assess the area, anteroposterior and transverse diameters, average thickness, and avulsion of the levator ani muscle. Differences between groups were evaluated by determining the mean differences and their respective 95% confidence intervals. The proportions of levator ani muscle avulsion were compared between elective cesarean section and vaginal birth using Fisher's exact test. RESULTS: The mean areas of the urogenital hiatus in the cases of vaginal and forceps deliveries were 17.0 and 20.1 cm², respectively, versus 12.4 cm² in the Control Group (elective cesarean). Avulsion of the levator ani muscle was observed in women who underwent vaginal delivery (3/25), however there was no statistically significant difference between cesarean section and vaginal delivery groups (p=0.5). CONCLUSION: Transperineal three-dimensional ultrasound was useful for assessing the pelvic floor of primiparous women, by allowing pelvic morphological changes to be differentiated according to the delivery mode.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):361-366
DOI 10.1590/S0100-72032011001100007
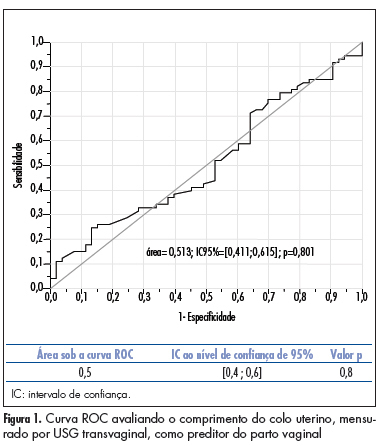
PURPOSE: to compare the accuracy of transvaginal ultrasonographic measurement of the uterine cervix with Bishop’s score for the prediction of vaginal delivery after labor induction, with 25 mcg of misoprostol. METHODS: a prospective study for the validation of a diagnostic test was conducted on 126 pregnant women with indication for labor induction. The patients were evaluated by Bishop’s score and transvaginal ultrasonography for cervical measurement. They also undergone obstetric transabdominal ultrasound to evaluate static and fetal weight, as well as the amniotic fluid index, and basal cardiotocography for the evaluation of fetal vitality. Labor was induced with vaginal and sublingual misoprostol, one of the tablets containing 25 mcg of the drug and the other only placebo. The tablets were administered every six hours, with a maximum number of eight. Frequency tables were obtained, and measures of central tendency and dispersion were calculated. ROC curves were constructed for the evaluation of Bishop’s score and ultrasonographic measurement of the uterine cervix for the prediction of vaginal delivery. RESULTS: the area under the ROC curve was 0.5 (p=0.8) for the ultrasonographic measurement of the uterine cervix, and 0.6 (p=0.02) for Bishop’s score (cut point ³4). Bishop’s score had a sensitivity of 56.2% and specificity of 67.9% for prediction of vaginal delivery, with a positive likelihood ratio of 1.75 and a negative one of 0.65. CONCLUSIONS: ultrasonographic measurement of the uterine cervix was not a good predictor of evolution to vaginal delivery among patients with misoprostol-induced labor. Bishop’s score was a better predictor of vaginal delivery under these circumstances.