Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(10):297-304
DOI 10.1590/S0100-72032011001000005
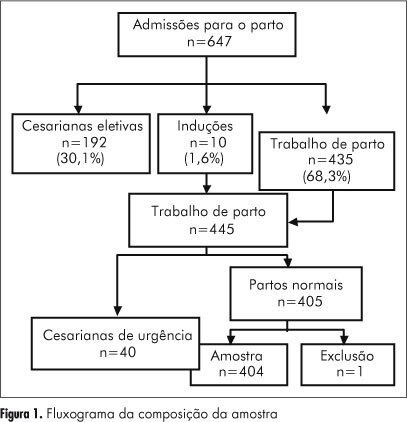
PURPOSE: To evaluate the quality of health care assistance during childbirth in the hospitals of Goiânia, in Brazil. METHODS: Thirteen hospitals were appraised from April to December 2007, and a random sample of 404 normal births was studied. Data were obtained from interviews with mothers after delivery and by consulting their medical records. The quality of assistance at birth was evaluated by using the Bologna score and by comparing the procedures used in those hospitals to standard recommended practices. RESULTS: The Bologna score presented an average value of 1.04 (95%CI=0.9-1.1). The elective caesarian rate was 30%, the emergency caesarian rate was 10%, and the rate of induced childbirth was 1.6% The percentage of childbirths attended by health care professionals was 100%, but pediatricians in the delivery room were present only in 30% of the time. During labor, half of the women had no evaluation of the uterine dynamics and 29% had no auscultation fetal monitoring. The partogram was used for only 28.5% of the women, whereas the use of oxytocin was 45.8%. CONCLUSIONS: The results indicate a poor quality of childbirth care with low values of the Bologna score, high elective and emergency caesarians rates, a high number of unnecessary and potentially harmful interventions, and an insufficient frequency of beneficial interventions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(11):671-679
DOI 10.1590/S0100-72032006001100007
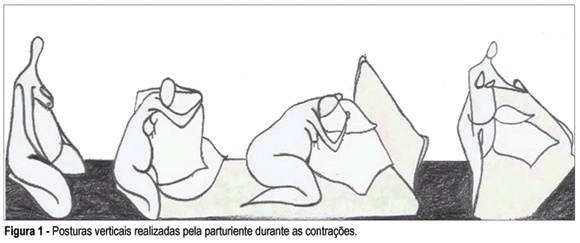
PURPOSE: to investigate the influence of the maternal mobility during the active phase of labor. METHODS: a prospective clinical trial was conducted through comparative analysis among a treatment group (n=50) and a control group (n=50), in the Obstetric Center of the Hospital Universitário da Universidade de São Paulo (USP). The inclusion criteria were: primigravidae with a single fetus on cephalic presentation, with 37 to 42 weeks of pregnancy, with two uterine contractions every ten minutes and with cervical dilatation until 4 cm, besides the agreement to sign the free and informed consent term. The evolution of labor for cesarean section was the exclusion criteria. The patients were assisted during the active phase of labor by the physiotherapist and encouraged for staying in vertical position and movement, according to each dilatation stage and fetus head progression. The control group had obstetric support without the presence of the physiotherapist; it was selected retrospectively, according to the same inclusion and exclusion criteria. RESULTS: 58 primigravidae between 15 and 37 years old were accompanied; 50 of them (86.2%) evolved to vaginal birth and eight (13.7%) evolved to cesarean section and were excluded. Among the patients who were accompanied, the mean of active phase was five hours and 16 minutes, while in the control group it was eight hours and 28 minutes (p<0.001). This difference was maintained in relation to the amniotic sac either whole or ragged. As for the cervix uterine evanescence, the treatment group showed a smaller period of active phase in association to a thin uterine cervix (p<0.001). In the treatment group, none of the patients used analgesics during the active phase, against 62% of the control group (p<0.001). In this group, all the patients used some kind of anesthesia for delivery; in the treatment group, among those who used anesthesia, 76% did it while the dilatation was 9 or 10 cm and 12% did not use any kind of anesthesia (p<0.05). The average weight of the newborns and the apgar did not show significant difference rates between the two groups. CONCLUSIONS: the good performance of maternal mobility has positive influences on the labor process: it increases the tolerance to pain, avoids the use of drugs during labor, improves the evolution of dilatation and reduces the duration of the active phase.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(9):523-529
DOI 10.1590/S0100-72032006000900004
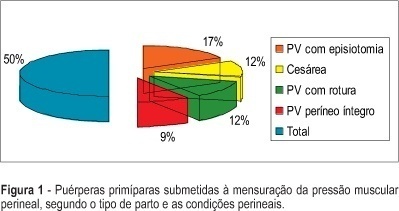
PURPOSE: to determine the values of perineal muscular force (PMF) in the lying and seated positions and to identify the values of PMF between first pregnancy, according to type and the characteristics of the vaginal delivery and cesarean section. METHODS: study of the transversal type, performed in a maternity of Brazilian Public the Health System (SUS) in the city of São Paulo. The sample consisted of 95 primiparae at term. Evaluation occurred between the 40th and 45 th, day with an interview, physical examination and measurement of PMF using a perineometer of the Kegel type. The measurement was carried out in the lying and seated positions, muscular status (at rest and in maximum contraction), and the average of three measures for each position and muscular state were considered. RESULTS: 76.8% (73) of the women had vaginal delivery and 23.2% (22) cesarean section. After vaginal delivery, intact perineum in 18.9%, (18), perineal rupture in 24.2% (23), and episiotomy in 33.7% (32) were observed. Obtained values of the PMF were: lying position muscular rest 18. 9 mmHg, lying position maximum contraction: 30,7 mmHg, seated position muscular rest: 34.5 mmHg, seated positions maximum muscular contraction: 46.5 mmHg. CONCLUSION: there was association between the type and the characteristics of the delivery and PMF.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(4):244-250
DOI 10.1590/S0100-72032006000400007
Osteogenesis imperfecta is a connective tissue disorder due to quantitative and qualitative anomalies in type 1 collagen, genetically transmitted by a dominant or recessive autosomal gene, leading to bone fragility. We report a case of a 19-year-old G1 PO patient referred to our institution following a screening ultrasound that demonstrated short limb fetal extremities. A level 3 scan was performed which evidenced an irregular cranial shape and compression of the cephalic pole with moderate transducer pressure. Limb shortening, decreased echoes and fractures of long bones were found on our scan evaluation. A vaginal delivery occurred at 35 weeks of gestation. The male newborn, weighing 1.990 grams had 6 and 8 in Apgar scores. The neonate was clearly abnormal, presenting irregular cranial shape, with poor ossification on X-ray, blue sclera, fractures and limb deformities. Postnatal evaluation was satisfactory and the neonate was discharged in good conditions. Prenatal diagnosis is important for an adequate pregnancy follow-up. Postnatal outcome was not related to vaginal delivery, as there were no recent fractures in the newborn.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(11):677-682
DOI 10.1590/S0100-72032005001100008
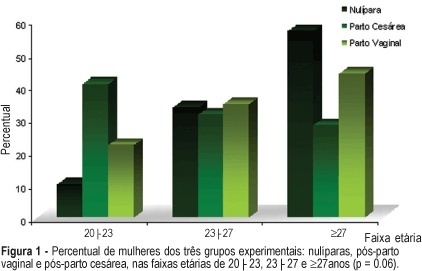
PURPOSE: to evaluate the influence of the delivery route on pelvic floor (PF) muscle strength. METHODS: a cross-sectional study was conducted to evaluate PF muscle strength by the pelvic floor strength evaluation (PFSE) test and perineometer in primiparous patients aged 20 to 30 years 4 to 6 months after delivery. The categorization was: zero lack of muscle contraction; one - weak contraction; two - moderate contraction not sustained for 6 s and three - normal contraction sustained for 6 s. A total of 94 patients were divided into there groups based on prior delivery route. They were: 32 patients with vaginal delivery with singleton cephalic presentation; 32 patients with cesarean delivery, and 30 nulliparous patients as a control group. The independent variable was delivery route and the dependent one was the muscle strength of the PF. Comparison between contraction levels was performed by Kruskal-Wallis and Dunn multiple comparison tests and the influence of delivery method was tested by chi2. Confidence interval of 95% was obtained for relative risk (RR) of Pf muscle strength changes and kappa statistics. RESULTS: the 1st and 3rd quartiles of delivery route regarding PF muscle strength were lower (p=0.01) for vaginal delivery (2.0;1-2) and intermediate for cesarean section (2.0;2-3) compared to the nulliparous (3.0;2-3) by the PFSE test and perineometer. RR of the altered examination was increased after vaginal delivery (RR=2.58; CI 95%: 1.32-5.04, p=0.002); (RR=2.31; CI 95%: 1.24-4.32, p=0.005), and after cesarean section (RR=1.56; CI 95%: 0.94-2.57, p= 0.12); (RR=1.38; CI 95%: 0.85-2.23, p=0.29) by AFA and perineometer, respectively. CONCLUSIONS: vaginal delivery decreased PF muscle strength when compared with cesarean delivery and control groups.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):189-196
DOI 10.1590/S0100-72032005000400005
PURPOSE: to create a predictive model for cesarean section at the "Professor Monteiro de Morais Maternity" after evaluation of antepartum risk factors of the pregnant women who delivered from September 1, 1999 to August 31, 2000, and then, to verify the efficacy of indication for cesarean section. METHODS: a longitudinal, case control study with 3.626 pregnant women was performed to identify the antepartum risk factors for cesarean section in the period from September 1, 1999 to August 31, 2000. Thereafter an ideal model able to quantify the risk for cesarean section for each patient in the presence of one or more risk factor was created. Then, the model was applied to the patients of the study in order to verify the efficacy of indication for cesarean section. RESULTS: the baseline risk for cesarean section was 15.2%. The concordance between the percentage estimated through logistic model and cesarean delivery was 86.6%. CONCLUSIONS: the logistic model was able to identify the baseline risk for cesarean section and to quantify the increase in risk for cesarean section in each patient when risk factors were introduced in the model. The model can be considered efficient and able to predict cesarean section because the agreemant between the prediction and the correct indication was 86.6%, and 53.6% of the patients who had vaginal delivery did not have any risk factor for cesarean section.