Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(7):309-316
DOI 10.1590/S0100-72032013000700005
PURPOSE: To determine perinatal outcomes and factors associated with fetal brain sparing effect diagnosed by Doppler flow velocimetry in patients with arterial hypertension. METHODS: We performed a cross-sectional retrospective study including 129 pregnant women with arterial hypertension and submitted to Doppler flow velocimetry, within fifteen days before delivery. Women with multiple pregnancies, fetal malformations, genital bleeding, placenta praevia, premature rupture of membranes, smoking, illicit drug use and chronic diseases were excluded. We analyzed the biological, socio-demographic and obstetric characteristics, as well the perinatal outcomes. To determine the association between variables, we used the χ² test, Fisher's exact test and Student's t-test. Multiple logistic regression analysis was performed to determine the factors associated with fetal centralization. RESULTS: Pre-eclampsia was the most frequent hypertensive disorder (53.5%) and fetal brain sparing effect was observed in 24.0% of fetuses. The prenatal factors associated with fetal brain sparing were the persistence of bilateral protodiastolic notches in uterine arteries (OR 3.6; 95%CI 1.4 - 9.4; p=0.009) and intrauterine growth restriction (IUGR) (OR 3.3; 95%CI 1.2 - 9.3; p=0.02). The perinatal outcomes associated with fetal brain sparing were gestational age <32 weeks, small for gestational age (SGA) infants, birth weight <2,500 g and perinatal death. There was no association with other maternal or neonatal variables. CONCLUSIONS: The main factors associated with fetal brain sparing were persistence of uterine arteries notches, IUGR, and increased frequency of adverse perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(4):157-163
DOI 10.1590/S0100-72032011000400002
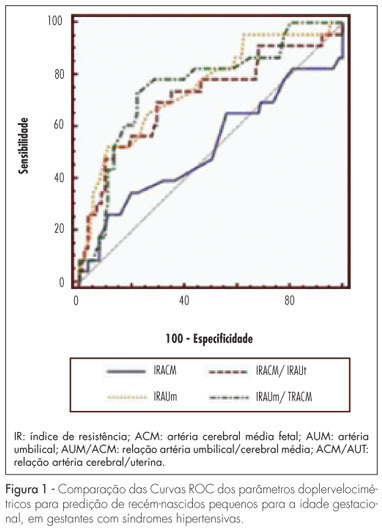
PURPOSE: to determine the best Doppler flow velocimetry index to predict small infants for gestational age (SGAI), in pregnant women with hypertensive syndromes. METHODS: a cross-sectional study was conducted enrolling 129 women with high blood pressure, submitted to dopplervelocimetry up to 15 days before delivery. Women with multiple fetuses, fetal malformations, genital bleeding, placental abruption, premature rupture of fetal membranes, smoking, use of illicit drugs, and chronic diseases were excluded. A receiver operating characteristic (ROC) curve for each Doppler variable was constructed to diagnose SGAI and the sensitivity (Se), specificity (Sp), positive (PLR) and negative (NLR) likelihood ratio were calculated. RESULTS: the area under the ROC curve for the middle cerebral artery resistance index was 52% (p=0.79) with Se, Sp, PLR, and NLR of 25.0, 89.1, 2.3 and 0.84% for a resistance index lower than 0.70, respectively. While the area under the ROC curve for the resistance index of the umbilical artery was 74% (p=0.0001), with Se=50.0%, Sp=90.0%, PLR=5.0 and NLR=0.56, for a resistance index higher or equal to 0.70. The area under the ROC curve for the resistance index umbilical artery/middle cerebral artery ratio was 75% (p=0.0001). When it was higher than 0.86, the Se, Sp, PLR and NLR were 70.8, 80.0, 3.4 and 0.36%, respectively. For the resistance index of the middle cerebral artery/uterine artery ratio, the area under the ROC curve was 71% (p=0.0001). We found a Se=52.2%, Sp=85.9%, PLR=3.7 and NLR=0.56, when the ratio was lower than 1.05. When we compared the area under the ROC curve of the four dopplervelocimetry indexes, we observed that only the resistance index umbilical artery/middle cerebral artery, resistance index middle cerebral artery/uterine artery and resistance index umbilical artery ratios seem to be useful for the prediction of SGA. CONCLUSION: in patients with high blood pressure during pregnancy, all dopplervelocimetry parameters, except the middle cerebral artery resistance index, can be used to predict SGAI. The umbilical artery/middle cerebral artery ratio seems to be the most recommended one.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(10):510-515
DOI 10.1590/S0100-72032010001000007
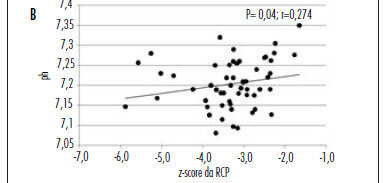
PURPOSE: to evaluate the hypothesis that the fetal cerebroplacental ratio (CPR) is related to acidemia at birth in pregnancies complicated by placental insufficiency detected before 34 weeks of gestation. METHODS: this is a prospective cohort study of 55 patients between 26 and 34 weeks of gestation with a diagnosis of placental insufficiency characterized by abnormal umbilical artery Doppler (pulsatility index>95p). Fetal assessment was performed for each patient by dopplervelocimetry of the umbilical artery, middle cerebral artery and ductus venosus, and by the fetal biophysical profile. CPR was calculated using the ratio between middle cerebral artery pulsatility index and umbilical artery pulsatility index, and the z-score was obtained (number of standard deviations of the mean value at each gestational age). Acidemia at birth was characterized when pH<7.2. RESULTS: of 55 patients, 29 (52.7%) presented acidemia at birth. In the group of fetal acidemia, when compared with the group with pH>7.2, a significant association was observed with CPR values (median 0.47 versus 0.58; p=0.009), pulsatility index of the umbilical artery (median 2.45 versus 1.93; p=0.003), ductus venosus pulsatility index for veins (PIV) (median 1.08 versus 0.85; p=0.034) and suspected or abnormal fetal biophysical profile (37 versus 8%; p=0.031). CPR analysis by z-score showed a negative tendency, but was not statistically significant (p=0.080). Significant correlations were found between pH at birth and CPR (r=0.45; p<0.01), z-score of CPR (r=0.27; p<0.05) and ductus venosus PIV (r=-0.35 p<0.01). CONCLUSION: CPR is associated with the presence of acidemia at birth in pregnancies with placental insufficiency detected before 34 weeks of gestation and this parameter could potentially represent a factor for assessing the severity of fetal involvement.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(1):11-18
DOI 10.1590/S0100-72032010000100003
PURPOSE: to describe adverse perinatal outcomes in patients with fetal blood flow centralization, using the relationship between the pulsatility indexes of the middle cerebral and umbilical arteries (MCAPI/UAPI), and between the resistance indexes of the middle cerebral and umbilical arteries (MCARI/UARI), as well as to compare both diagnostic indexes. METHODS: 151 pregnant women with diagnosis of blood flow centralization, attended to at the maternity hospital of Universidade Estadual de Campinas, whose delivery occurred up to 15 days after the ultrasonographic diagnosis, were included. It was considered as adverse perinatal outcomes: Apgar index lower than 7 at the fifth minute, permanence in neonatal ICU, small fetus for the gestational age, severe fetal suffering, perinatal death, hypoglycemia, polycythemia, necrotizing enterocolitis, brain hemorrhage, lung hemorrhage, anemia, septicemia, hyaline membrane disease, convulsive syndromes, hyperreflexia syndrome and kidney insufficiency. Rates of the perinatal adverse outcomes (PAO) for the brain-placentary ratios have been compared, using Fisher's exact or Pearson's χ2 tests, at 5% significance level. Adverse perinatal outcomes according to the gestational age have been evaluated using the Cochrane-Armitage test for trend. RESULTS: the adverse perinatal outcomes for the group with the two indexes altered were: 62.5% of the newborns needed to be placed in an ICU, 75.2% were small for the gestational age (SGA), 35.3% were under severe fetal suffering, 84.4% had hypoglycemia, 8.3% polycythemia, 4.2% necrotizing enterocolitis, and 2.1% brain hemorrhage. There has been significant association between the MCAPI/UAPI and MCARI/UARI ratios along the gestational age, and the need for neonatal intensive care, small fetuses for the gestational age, septicemia, necrotizing enterocolitis, kidney insufficiency, hyaline membrane disease, and anemia. There has been no significant difference between the two indexes of adverse perinatal outcome.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(2):82-88
DOI 10.1590/S0100-72032009000200006
PURPOSE: to evaluate the effect of magnesium sulphate on the pulsatility index (PI) of the uterine, umbilical and fetal middle cerebral arteries, according to the persistency or not of the bilateral protodiastolic notch of the uterine arteries in severe pre-eclampsia. METHODS: a cohort study including 40 pregnant women with severe pre-eclampsia, 23 of them presenting bilateral protodiastolic notch, and 17, unilateral/absent notch. The patients were submitted to Doppler velocimetry before and 20 minutes after the intravenous administration of 6 g of magnesium sulphate. The examination was carried out with the patient in semi-Fowler position, the sonograms being obtained during fetal inactivity, in apnea and absent uterine contraction periods. All the exams were performed by two researchers, the average being considered as the final result. Wilcoxon's test was used to compare the PI, before and after magnesium sulphate in both groups. The difference between the two measurements (before and after magnesium sulphate) was compared between the groups (bilateral incision and unilateral/absent incision) using the Mann-Whitney test. RESULTS: there was a significant increase in the maternal heart rate (MHR) and decrease in the maternal blood pressure, and in the PI medians of the two uterine arteries and in the fetal middle cerebral artery, after magnesium sulphate in both groups. There was a significant decrease in the PI of the left uterine artery and in the umbilical artery, only in the protodiastolic unilateral/absent notch group. Nevertheless, it was not found any significant difference regarding the PI of the right uterine artery, or the cerebral/umbilical relationship, before and after magnesium sulphate in each group. No difference between the groups was found, before and after magnesium sulphate, for any of the studied outcomes. CONCLUSIONS: after the intravenous administration of 6 g of magnesium sulphate to patients with severe pre-eclampsia, a decrease in blood pressure and in the PI of the uterine, umbilical and fetal middle cerebral arteries occurs, besides the increase in the MHR, not influenced by the presence of bilateral protodiastolic notch in the uterine arteries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(6):437-442
DOI 10.1590/S0100-72032003000600009
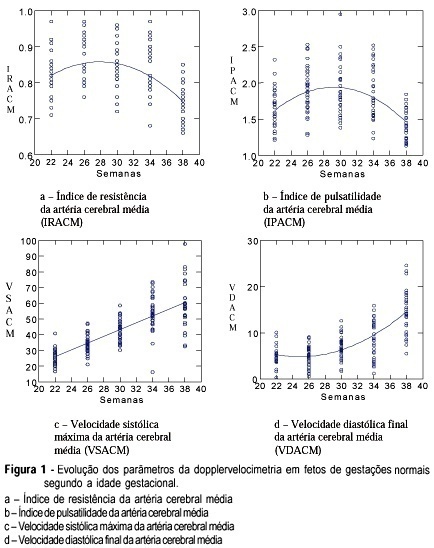
PURPOSE: to study the evolution of the resistance and pulsatility indices, maximum velocity, final diastolic velocity and time of acceleration of the middle cerebral artery of fetuses between 22 and 38 weeks of gestation. METHODS: a prospective and longitudinal observational study was conducted on 33 fetuses of normal pregnant women evaluated between 22 and 38 weeks of pregnancy. The gestational age was determined on the basis of the date of the last menstruation and/or by ultrasound examination during the first trimester. Doppler ultrasound examination was performed by a single observer using an Image Point 1800 (Hewlett Packard) apparatus equipped with a multiple frequency transducer. For the acquisition of the Doppler tracing of the middle cerebral artery, the sample indicator was calibrated for a sample volume of 1 mm³ and placed on the anterior middle cerebral artery as close as possible to the skullcap. The insonation angle was kept between 5º and 19º and the filter was adjusted to a frequency of 50-100 Hz. The newborn infants were evaluated in order to confirm that the fetuses were vigorous and adequate for gestational age. RESULTS: the results obtained for the resistance and pulsatility indices revealed a 2nd-degree equation, representing a parabola whose values for the resistance index were 0.81 during the 22nd week and 0.75 during the 38th week. The pulsatility index was 1.59 during the 22nd week and 1.45 during the 38th week. Maximum systolic velocity increased progressively along pregnancy, with values of 26.3 cm/s during the 22nd week and 57.7 cm/s during the 38th week. Final diastolic velocity increased progressively from the 26th week (5.21 cm/s) to term (14.6 cm/s). Acceleration time increased significantly only between 26 and 30 weeks, with values of 0.04 s during the 26th week and 0.05 s during the 30th week. CONCLUSION: it was concluded that the evolution of the resistance and pulsatility indices and of maximum systolic velocity were similar to those of most studies described in the literature. Acceleration time presented few modifications during the evaluated gestational weeks.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(2):113-120
DOI 10.1590/S0100-72032002000200007
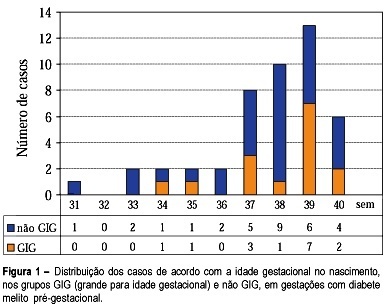
Purpose: to study fetal surveillance examinations in pregnancies complicated by pregestational diabetes mellitus, and to correlate them with large for gestational age (LGA) newborns. Methods: Between March 1999 and June 2001, 46 singleton pregnancies with pregestational diabetes mellitus without fetal anomalies were followed prospectively. From the 28th gestational week on, the following examinations were performed weekly: fetal biophysical profile, amniotic fluid index (AFI), and dopplervelocimetry of umbilical and middle cerebral arteries. The newborns with birthweight above the 90th percentile according to local standard values were characterized as LGA infants. Fisher's exact test and Student's t test were used for statistical analysis. Results: The mean gestational age at delivery was 37.6 weeks and 15 (32.6%) newborns were LGA. LGA fetuses showed significant increase in the AFI mean performed in the 32nd (16.5 cm, p=0.02), 33rd (16.7 cm, p=0.03), 34th (17.0 cm, p=0.02), 35th (17.9 cm, p=0.000), 36th (15.8 cm, p=0.03) and 37th (17.5 cm, p=0.003) weeks. Non-LGA fetuses presented the following mean AFI values: 13.5cm (32nd week), 13.1cm (33th week), 13.4 (34th week), 12.8 (35th week), 12.5 (36th week) and 12.8cm (37th week). AFI values equal to or above 18.0 cm were associated with the occurrence of LGA infants, when detected at the following gestational ages: 34th (60%, p=0.03), 35th (71.4%, p=0.01), 36th (80%, p=0.02) and 37th (66.7%, p=0.04) week. Non-LGA infants presented the following proportion of AFI values equal to or above 18.0 cm: 40.0% (34th week), 28.6% (35th week), 20.0% (36th week), and 33.3% (37th week). Conclusions: abnormal increase in AFI, mainly with values equal to or above 18.0 cm, is related to LGA infants at delivery. The maternal treatment should be adjusted to achieve the best result for maternal-fetal control, according to the AFI values during pregnancy.