Home
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):706-723
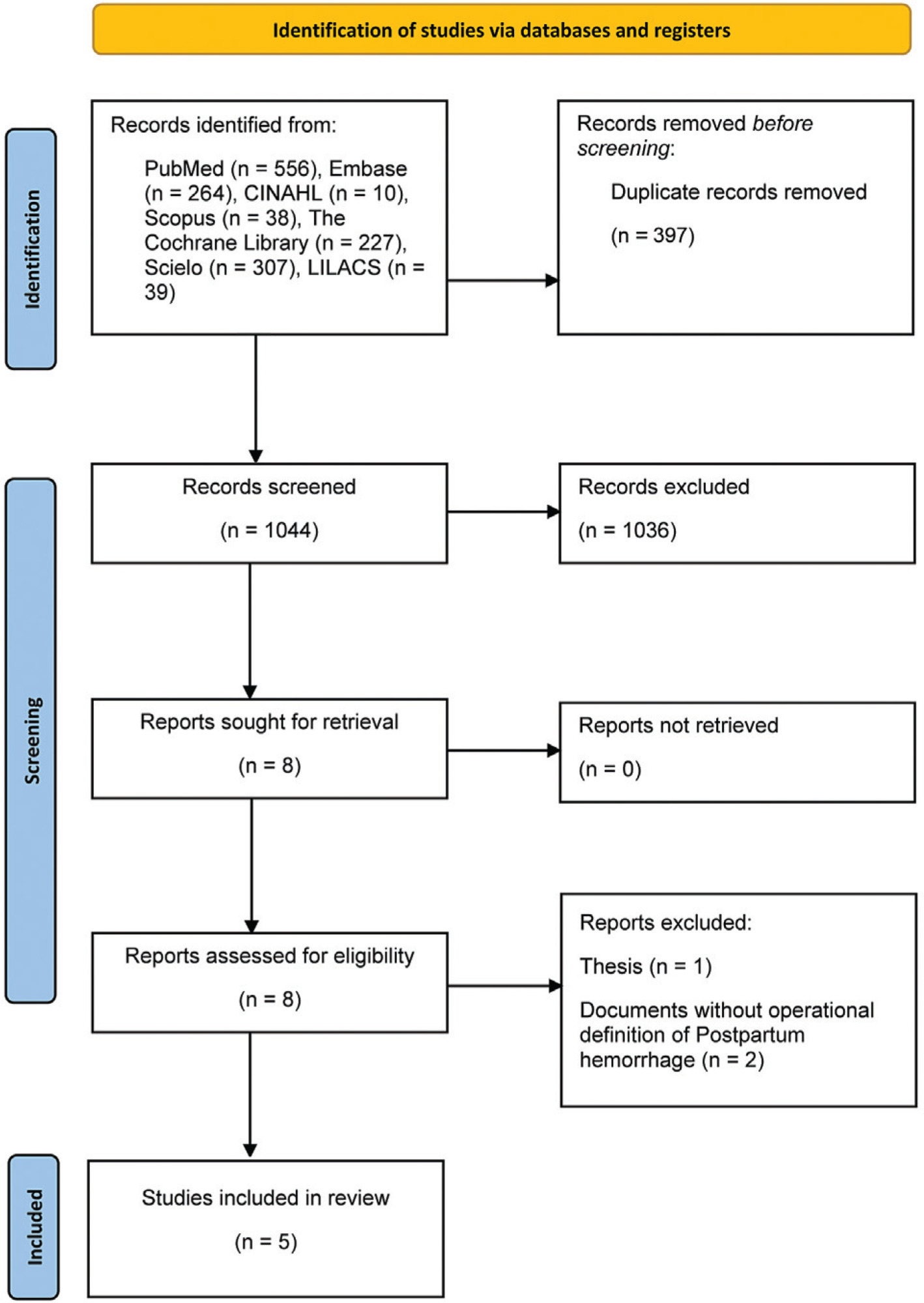
To determine the association between fetal macrosomia (FM) and postpartum hemorrhage (PPH) in Latin American and Caribbean (LAC) women.
Studies evaluating the association between FM and PPH (≥ 500 ml) and severe PPH (≥ 1,000 ml) until November 4, 2021, indexed in CINHAL, Scopus, Embase, Cochrane Library, MEDLINE, LILACS, and SciELO.
Inclusion criteria were cohort and case-control studies that provided the number of PPH and FM cases. Exclusion criteria were studies lacking information about the number of cases, with a population of women who were not from LAC; published in a language other than English, Spanish, or Portuguese, and with a different design.
Data extraction was performed independently by two authors, and discrepancies were resolved with a third author. Data regarding FM and PPH cases were retrieved.
Of the 1,044 articles evaluated, 5 studies were included, from 6 different countries: Argentina and Uruguay (multi-country), West Indies, Antigua and Barbuda, French Guyana, and Suriname. The pooled odds ratio (OR) for FM and PPH in the meta-analysis (five studies) was 2.10 (95% confidence interval [CI]: 1.79–2.47; I2: 0%), with estimates within this 95% CI in the sensitivity analysis. The combined OR for severe PPH (3 studies) was 1.61 (95% CI: 0.40–6.48; I2: 91.89%), showing high heterogeneity.
There was a positive association between FM and PPH in the LAC, increasing the risk of the presence of this event 2-fold. The high heterogeneity of the studies that measured severe PPH does not allow drawing conclusions about the estimates obtained.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):706-723
To determine the association between fetal macrosomia (FM) and postpartum hemorrhage (PPH) in Latin American and Caribbean (LAC) women.
Studies evaluating the association between FM and PPH (≥ 500 ml) and severe PPH (≥ 1,000 ml) until November 4, 2021, indexed in CINHAL, Scopus, Embase, Cochrane Library, MEDLINE, LILACS, and SciELO.
Inclusion criteria were cohort and case-control studies that provided the number of PPH and FM cases. Exclusion criteria were studies lacking information about the number of cases, with a population of women who were not from LAC; published in a language other than English, Spanish, or Portuguese, and with a different design.
Data extraction was performed independently by two authors, and discrepancies were resolved with a third author. Data regarding FM and PPH cases were retrieved.
Of the 1,044 articles evaluated, 5 studies were included, from 6 different countries: Argentina and Uruguay (multi-country), West Indies, Antigua and Barbuda, French Guyana, and Suriname. The pooled odds ratio (OR) for FM and PPH in the meta-analysis (five studies) was 2.10 (95% confidence interval [CI]: 1.79–2.47; I2: 0%), with estimates within this 95% CI in the sensitivity analysis. The combined OR for severe PPH (3 studies) was 1.61 (95% CI: 0.40–6.48; I2: 91.89%), showing high heterogeneity.
There was a positive association between FM and PPH in the LAC, increasing the risk of the presence of this event 2-fold. The high heterogeneity of the studies that measured severe PPH does not allow drawing conclusions about the estimates obtained.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(6):337-346
To compare the use of mirabegron with anticholinergics drugs for the treatment of overactive bladder (OB).
Systematic searches were conducted in EMBASE, PUBMED, Cochrane, and LILACS databases from inception to September 2021. We included RCTs, women with clinically proven OB symptoms, studies that compared mirabegron to antimuscarinic drugs, and that evaluated the efficacy, safety or adherence.
RevMan 5.4 was used to combine results across studies. We derived risk ratios (RRs) and mean differences with 95% CIs using a random-effects meta-analytic model. Cochrane Collaboration Tool and GRADE was applied for risk of bias and quality of the evidence.
We included 14 studies with a total of 10,774 patients. Fewer total adverse events was reported in mirabegron group than in antimuscarinics group [RR 0.93 (0.89–0.98)]. The risk of gastrointestinal tract disorders and dry mouth were lower with mirabegron [RR 0,58 (0.48–0.68); 9375 patients; RR 0.44 (0.35–0.56), 9375 patients, respectively]. No difference was reported between mirabegron and antimuscarinics drugs for efficacy. The adherence to treatment was 87.7% in both groups [RR 0.99 (0.98–1.00)].
Mirabegron and antimuscarinics have comparable efficacy and adherence rates; however, mirabegron showed fewer total and isolated adverse events.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(6):337-346
To compare the use of mirabegron with anticholinergics drugs for the treatment of overactive bladder (OB).
Systematic searches were conducted in EMBASE, PUBMED, Cochrane, and LILACS databases from inception to September 2021. We included RCTs, women with clinically proven OB symptoms, studies that compared mirabegron to antimuscarinic drugs, and that evaluated the efficacy, safety or adherence.
RevMan 5.4 was used to combine results across studies. We derived risk ratios (RRs) and mean differences with 95% CIs using a random-effects meta-analytic model. Cochrane Collaboration Tool and GRADE was applied for risk of bias and quality of the evidence.
We included 14 studies with a total of 10,774 patients. Fewer total adverse events was reported in mirabegron group than in antimuscarinics group [RR 0.93 (0.89–0.98)]. The risk of gastrointestinal tract disorders and dry mouth were lower with mirabegron [RR 0,58 (0.48–0.68); 9375 patients; RR 0.44 (0.35–0.56), 9375 patients, respectively]. No difference was reported between mirabegron and antimuscarinics drugs for efficacy. The adherence to treatment was 87.7% in both groups [RR 0.99 (0.98–1.00)].
Mirabegron and antimuscarinics have comparable efficacy and adherence rates; however, mirabegron showed fewer total and isolated adverse events.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(8):776-784
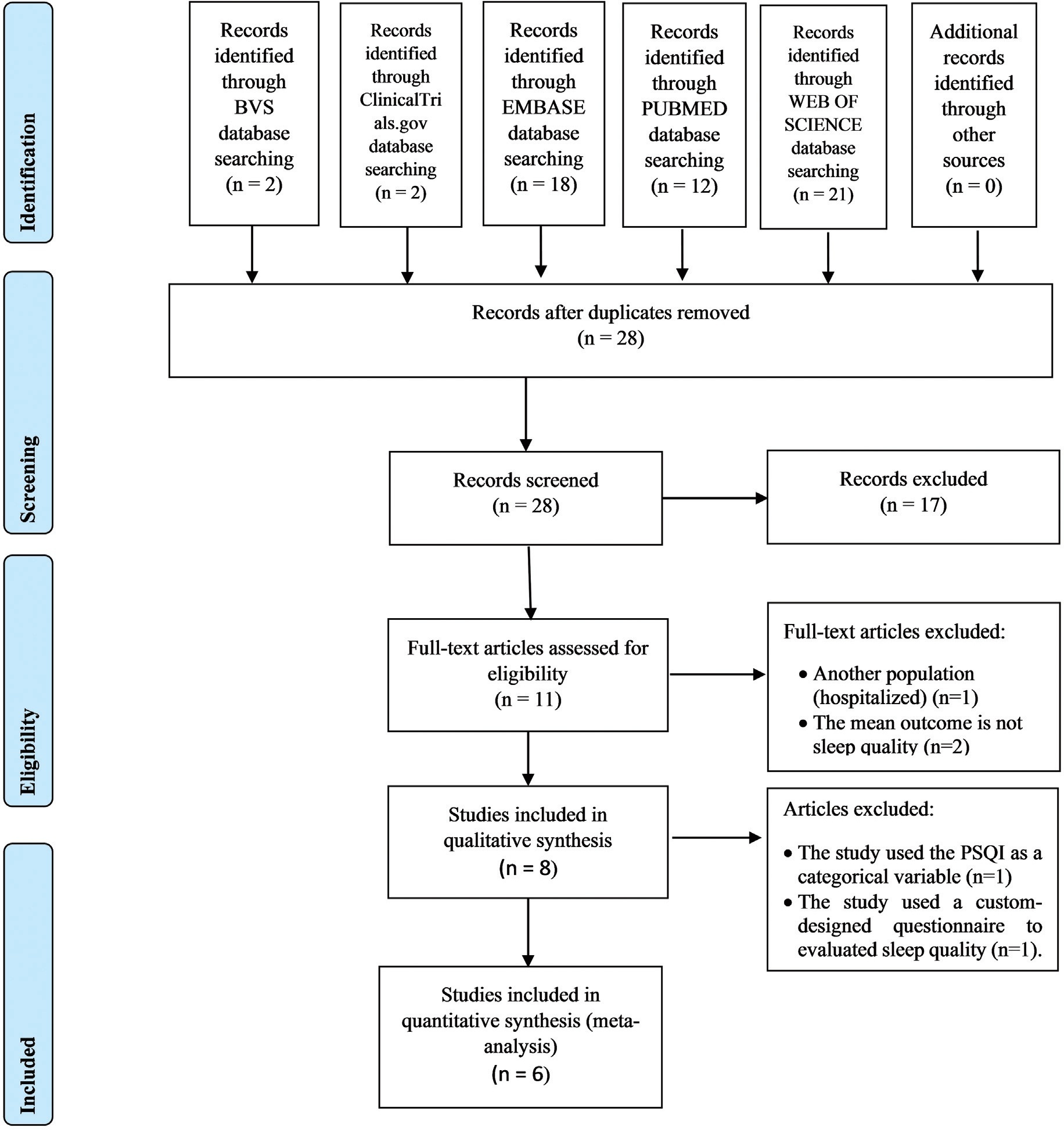
To investigate the effect of non-pharmacological interventions to improve sleep quality during pregnancy.
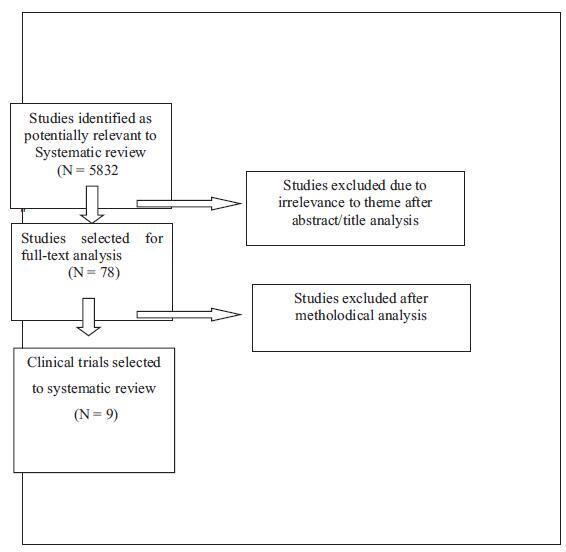
A search was made in the NCBI/PubMed, ClinicalTrials.gov, Embase, BVS, and Web of Science databases. There were no limitations regarding language, sample size, and type of non-pharmacological intervention. We have included prospective clinical trials between July 2014 and July 2019.
This study was registered in the Prospective International Registration of Systematic Reviews (PROSPERO) database was performed. Publication bias was also assessed with funnel plots. the primary outcome was the total score in the Pittsburgh Sleep Quality Index (PSQI) before and after intervention. Risk of bias and the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria were used for assessing methodological quality. From the 28 retrieved studies, we have selected 8 for qualitative analysis and 6 for meta-analysis.
Two independent reviewers performed the study selection. In the case of disagreement, a third senior reviewer was consulted. The study was initially assessed based on the title, followed by abstract. Lastly, the full text was assessed to be included.
A significant improvement on the sleep quality (PSQI score) was observed when all interventions were grouped (MD = -3.03, 95%CI -4.15 to -1.92, n= 623, i2= 84%, p< 0.001). Analysis by subgroup (music listening: MD = -1.96, 95% CI -3.27 to -0.65, n= 207, i2= 67%, p= 0.003 and other interventions: MD = -3.66, 95% CI -4.93 to -2.40, n= 416, i2 = 80%, p< 0.001) showed an improvement, with high heterogeneity. Risk of bias has shown performance and detection bias for almost studies, and GRADE evidence was very low for all analyzed variables.
Non-pharmacological interventions—listening to music, physical exercise, relaxation exercises, lettuce seed, sleep hygiene, and acupressure—are effective for improving sleep quality during pregnancy.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(8):776-784
To investigate the effect of non-pharmacological interventions to improve sleep quality during pregnancy.
A search was made in the NCBI/PubMed, ClinicalTrials.gov, Embase, BVS, and Web of Science databases. There were no limitations regarding language, sample size, and type of non-pharmacological intervention. We have included prospective clinical trials between July 2014 and July 2019.
This study was registered in the Prospective International Registration of Systematic Reviews (PROSPERO) database was performed. Publication bias was also assessed with funnel plots. the primary outcome was the total score in the Pittsburgh Sleep Quality Index (PSQI) before and after intervention. Risk of bias and the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria were used for assessing methodological quality. From the 28 retrieved studies, we have selected 8 for qualitative analysis and 6 for meta-analysis.
Two independent reviewers performed the study selection. In the case of disagreement, a third senior reviewer was consulted. The study was initially assessed based on the title, followed by abstract. Lastly, the full text was assessed to be included.
A significant improvement on the sleep quality (PSQI score) was observed when all interventions were grouped (MD = -3.03, 95%CI -4.15 to -1.92, n= 623, i2= 84%, p< 0.001). Analysis by subgroup (music listening: MD = -1.96, 95% CI -3.27 to -0.65, n= 207, i2= 67%, p= 0.003 and other interventions: MD = -3.66, 95% CI -4.93 to -2.40, n= 416, i2 = 80%, p< 0.001) showed an improvement, with high heterogeneity. Risk of bias has shown performance and detection bias for almost studies, and GRADE evidence was very low for all analyzed variables.
Non-pharmacological interventions—listening to music, physical exercise, relaxation exercises, lettuce seed, sleep hygiene, and acupressure—are effective for improving sleep quality during pregnancy.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):699-709
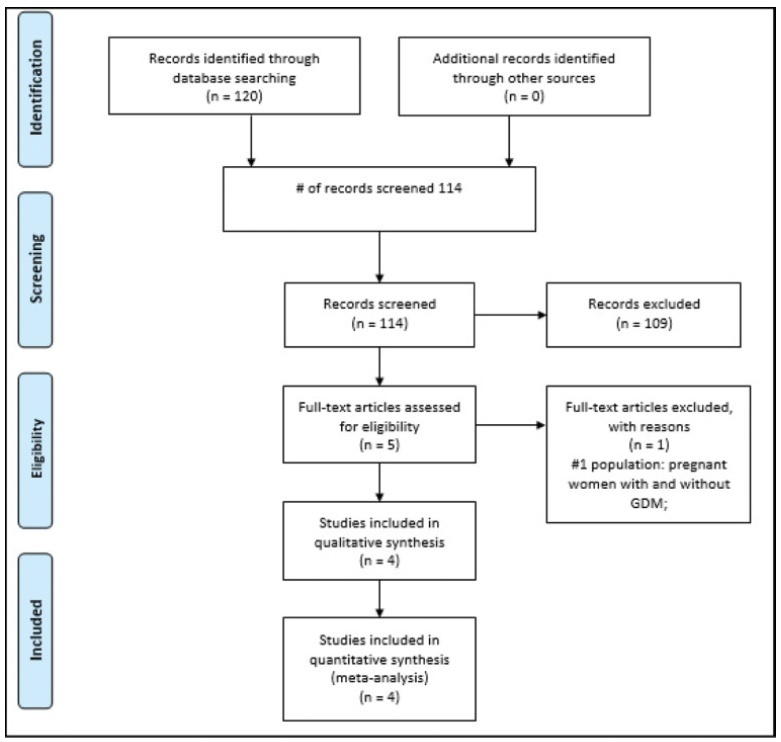
To evaluate the effects of vitamin D supplementation in the postpartum period of women with previous gestational diabetes mellitus (GDM).
Randomized clinical trials of pregnant women with GDM of any chronological, gestational age and parity, with no history of previous disease who received vitamin D supplementation in the prenatal and/or postpartum period and were evaluated in the postpartum period were included. The PubMed, EMBASE, Cochrane, and LILACS databases were consulted until July 2019. Serum vitamin D concentration (25- hydroxyvitamin D in nmol/L), fasting blood glucose, glycated hemoglobin, serum calcium concentration, homeostatic model assessment of insulin resistance (HOMAIR), quantitative insulin sensitivity check index (QUICKI), parathyroid hormone (PTH) and body mass index (BMI) were evaluated. Similar results in at least two trials were plotted using the RevMan 5; Cochrane Collaboration, Oxford, Reino Unido. The quality of the evidence was generated according to the classification, development, and evaluation of the classification of the recommendations.
Four studies were included in the present review (200 women). The findings indicate that there is no difference in the postpartum period in women diagnosed with previous GDM who received vitamin D supplementation in the prenatal and/or in the postpartum period, showing only that there was a significant increase in the concentration of vitamin D (relative risk [RR]: 1.85; 95% confidence interval [CI]: 1.02-2.68).
This increase in the concentration of vitamin D should be interpreted with caution, since the assessment of the quality of the evidence was very low. For the other analyzed outcomes, there was no significance between the intervention and control groups, and the outcomes, when analyzed in their strength of evidence, were considered very low and low in their evaluation.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):699-709
To evaluate the effects of vitamin D supplementation in the postpartum period of women with previous gestational diabetes mellitus (GDM).
Randomized clinical trials of pregnant women with GDM of any chronological, gestational age and parity, with no history of previous disease who received vitamin D supplementation in the prenatal and/or postpartum period and were evaluated in the postpartum period were included. The PubMed, EMBASE, Cochrane, and LILACS databases were consulted until July 2019. Serum vitamin D concentration (25- hydroxyvitamin D in nmol/L), fasting blood glucose, glycated hemoglobin, serum calcium concentration, homeostatic model assessment of insulin resistance (HOMAIR), quantitative insulin sensitivity check index (QUICKI), parathyroid hormone (PTH) and body mass index (BMI) were evaluated. Similar results in at least two trials were plotted using the RevMan 5; Cochrane Collaboration, Oxford, Reino Unido. The quality of the evidence was generated according to the classification, development, and evaluation of the classification of the recommendations.
Four studies were included in the present review (200 women). The findings indicate that there is no difference in the postpartum period in women diagnosed with previous GDM who received vitamin D supplementation in the prenatal and/or in the postpartum period, showing only that there was a significant increase in the concentration of vitamin D (relative risk [RR]: 1.85; 95% confidence interval [CI]: 1.02-2.68).
This increase in the concentration of vitamin D should be interpreted with caution, since the assessment of the quality of the evidence was very low. For the other analyzed outcomes, there was no significance between the intervention and control groups, and the outcomes, when analyzed in their strength of evidence, were considered very low and low in their evaluation.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):400-408
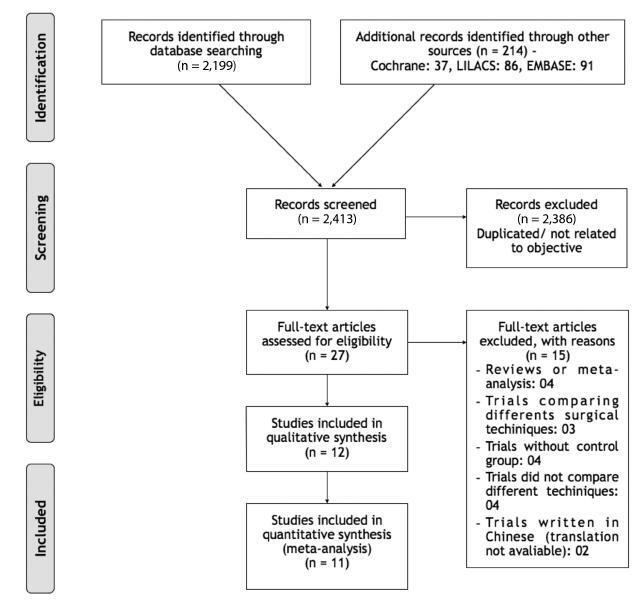
The objective of this review was to analyze the impact on ovarian reserve of the different hemostatic methods used during laparoscopic cystectomy.
The studies were identified by searching electronic databases (MEDLINE, Embase, Cochrane, LILACS) and scanning reference lists of articles.
We selected clinical trials that assessed the influence of hemostatic techniques on ovarian reserve in patients with ovarian cysts with benign sonographic appearance submitted to laparoscopic cystectomy by stripping technique. The included trials compared different laparoscopic hemostatic techniques: suture, bipolar electrocoagulation, ultrasonic energy and hemostatic sealants. The outcomes evaluated were level of serum anti-Mullerian hormone (AMH) and antral follicle count (AFC). The possibility of publication bias was evaluated by funnel plots.
Twelve trials involving 1,047 patients were evaluated. Laparoscopic suturewas superior to bipolar coagulationwhen evaluating serum AMHand AFC, in the 1st, 3rd, 6th and 12thmonth after surgery. In the comparison between bipolar and hemostatic sealants, the results favored the use of hemostatic agents. The use of ultrasonic energy was not superior to the use of bipolar energy.
We recommend suture for hemostasis during laparoscopic cystectomy.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):400-408
The objective of this review was to analyze the impact on ovarian reserve of the different hemostatic methods used during laparoscopic cystectomy.
The studies were identified by searching electronic databases (MEDLINE, Embase, Cochrane, LILACS) and scanning reference lists of articles.
We selected clinical trials that assessed the influence of hemostatic techniques on ovarian reserve in patients with ovarian cysts with benign sonographic appearance submitted to laparoscopic cystectomy by stripping technique. The included trials compared different laparoscopic hemostatic techniques: suture, bipolar electrocoagulation, ultrasonic energy and hemostatic sealants. The outcomes evaluated were level of serum anti-Mullerian hormone (AMH) and antral follicle count (AFC). The possibility of publication bias was evaluated by funnel plots.
Twelve trials involving 1,047 patients were evaluated. Laparoscopic suturewas superior to bipolar coagulationwhen evaluating serum AMHand AFC, in the 1st, 3rd, 6th and 12thmonth after surgery. In the comparison between bipolar and hemostatic sealants, the results favored the use of hemostatic agents. The use of ultrasonic energy was not superior to the use of bipolar energy.
We recommend suture for hemostasis during laparoscopic cystectomy.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):333-347
To investigate the relationship between maternal exposure to alcohol and low birthweight (LBW).
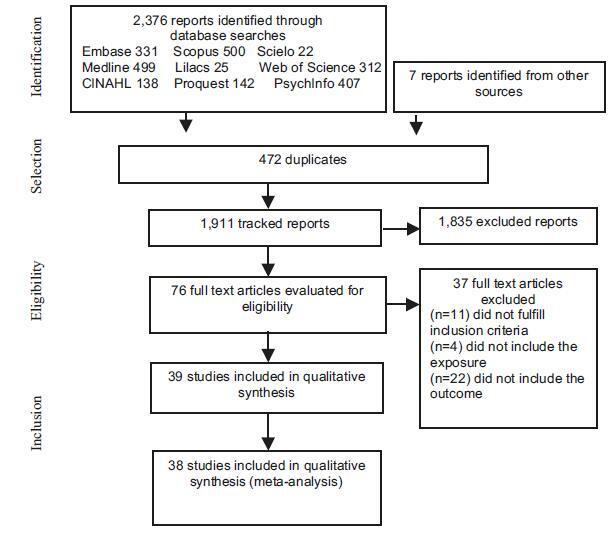
The literature search was performed in January 2017 using the following electronic databases: Medline, Embase, LILACS, SciELO, Web of Science, Scopus, CINHAL, Proquest, and PsychInfo. The search strategy used the following terms: alcohol drinking, binge drinking, alcohol-related disorders, alcoholism, alcohol addiction/ use/abuse/consumption, light/moderate/social/low drinking, low birthweight, case-control studies, retrospective studies, and cohort studies. No restrictions regarding language or publication date were considered. The literature search yielded 2,383 articles, and after screening and eligibility assessment, 39 articles were included in the systematic review, and 38 studies were included in the meta-analysis.
Maternal alcohol consumption was associated with LBWamong retrospective cohort studies (relative risk [RR] = 1.37; 95%CI [confidence interval]:1.10-1.77; I2 = 98.4%; p < 0.01). Prospective cohort studies (RR = 1.11; 95%CI: 0.98-1.25; I2 = 81.5%; p < 0.01), and case-control studies (odds ration [OR] = 1.16; 95%CI: 0.68-1.97; I2 = 61.2%; p = 0.05) showed no association between alcohol and LBW.No publication bias was identified, and the meta-regression showed that the sample size influenced the high heterogeneity among retrospective cohort studies. The subgroup analysis showed differences in association between groups when compared by sample size, type of adjustment, or crude measures and publication year.
We have not found an association between alcohol consumption during gestation and LBW in the analysis in all of the subgroups. In addition, we have found a high heterogeneity between the primary studies, which is related to methodological differences in the conduction of these studies.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):333-347
To investigate the relationship between maternal exposure to alcohol and low birthweight (LBW).
The literature search was performed in January 2017 using the following electronic databases: Medline, Embase, LILACS, SciELO, Web of Science, Scopus, CINHAL, Proquest, and PsychInfo. The search strategy used the following terms: alcohol drinking, binge drinking, alcohol-related disorders, alcoholism, alcohol addiction/ use/abuse/consumption, light/moderate/social/low drinking, low birthweight, case-control studies, retrospective studies, and cohort studies. No restrictions regarding language or publication date were considered. The literature search yielded 2,383 articles, and after screening and eligibility assessment, 39 articles were included in the systematic review, and 38 studies were included in the meta-analysis.
Maternal alcohol consumption was associated with LBWamong retrospective cohort studies (relative risk [RR] = 1.37; 95%CI [confidence interval]:1.10-1.77; I2 = 98.4%; p < 0.01). Prospective cohort studies (RR = 1.11; 95%CI: 0.98-1.25; I2 = 81.5%; p < 0.01), and case-control studies (odds ration [OR] = 1.16; 95%CI: 0.68-1.97; I2 = 61.2%; p = 0.05) showed no association between alcohol and LBW.No publication bias was identified, and the meta-regression showed that the sample size influenced the high heterogeneity among retrospective cohort studies. The subgroup analysis showed differences in association between groups when compared by sample size, type of adjustment, or crude measures and publication year.
We have not found an association between alcohol consumption during gestation and LBW in the analysis in all of the subgroups. In addition, we have found a high heterogeneity between the primary studies, which is related to methodological differences in the conduction of these studies.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(2):116-123
To evaluate if performing anti-incontinence procedures during surgical anterior and/or apical prolapse correction in women with asymptomatic urinary incontinence (UI) may prevent stress urinary incontinence (SUI) postoperatively.
We have performed a systematic review of articles published in the PubMed, Cochrane Library, and Lilacs databases until March 31, 2016. Two reviewers performed the data collection and analysis, independently. All of the selected studiesweremethodologically analyzed. The results are presented as relative risk (RR), with a 95% confidence interval (CI).
After performing the selection of the studies, only nine trials fulfilled the necessary prerequisites. In the present review, 1,146 patients were included. Altogether, the review included trials of three different types of anti-incontinence procedures. We found that performing any anti-incontinence procedure at the same time of prolapse repair reduced the incidence of SUI postoperatively (RR = 0.50; 95% CI: 0.28-0.91). However, when we performed the analysis separately by the type of anti-incontinence procedure, we found different results. In the subgroup analysis with midurethral slings, it is beneficial to perform it to reduce the incidence of SUI (RR = 0.08; 95% CI: 0.02-0.28). On the other hand, in the subgroup analysis with Burch colposuspension, there was no significant difference with the control group (RR = 1.47; 95% CI: 0.28-7.79]).
Performing any prophylactic anti-incontinence procedure at the same time as prolapse repair reduced the incidence of SUI postoperatively. The Burch colposuspension did not show any decrease in the incidence of SUI postoperatively.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(2):116-123
To evaluate if performing anti-incontinence procedures during surgical anterior and/or apical prolapse correction in women with asymptomatic urinary incontinence (UI) may prevent stress urinary incontinence (SUI) postoperatively.
We have performed a systematic review of articles published in the PubMed, Cochrane Library, and Lilacs databases until March 31, 2016. Two reviewers performed the data collection and analysis, independently. All of the selected studiesweremethodologically analyzed. The results are presented as relative risk (RR), with a 95% confidence interval (CI).
After performing the selection of the studies, only nine trials fulfilled the necessary prerequisites. In the present review, 1,146 patients were included. Altogether, the review included trials of three different types of anti-incontinence procedures. We found that performing any anti-incontinence procedure at the same time of prolapse repair reduced the incidence of SUI postoperatively (RR = 0.50; 95% CI: 0.28-0.91). However, when we performed the analysis separately by the type of anti-incontinence procedure, we found different results. In the subgroup analysis with midurethral slings, it is beneficial to perform it to reduce the incidence of SUI (RR = 0.08; 95% CI: 0.02-0.28). On the other hand, in the subgroup analysis with Burch colposuspension, there was no significant difference with the control group (RR = 1.47; 95% CI: 0.28-7.79]).
Performing any prophylactic anti-incontinence procedure at the same time as prolapse repair reduced the incidence of SUI postoperatively. The Burch colposuspension did not show any decrease in the incidence of SUI postoperatively.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):631-641
Previous studies investigating the association between angiotensin-converting enzyme (ACE) gene insertion/deletion (I/D) polymorphism and recurrent pregnancy loss (RPL) risk has provided inconsistent results. The aim of our study was to assess the association between the ACE I/D polymorphism and risk of RPL.
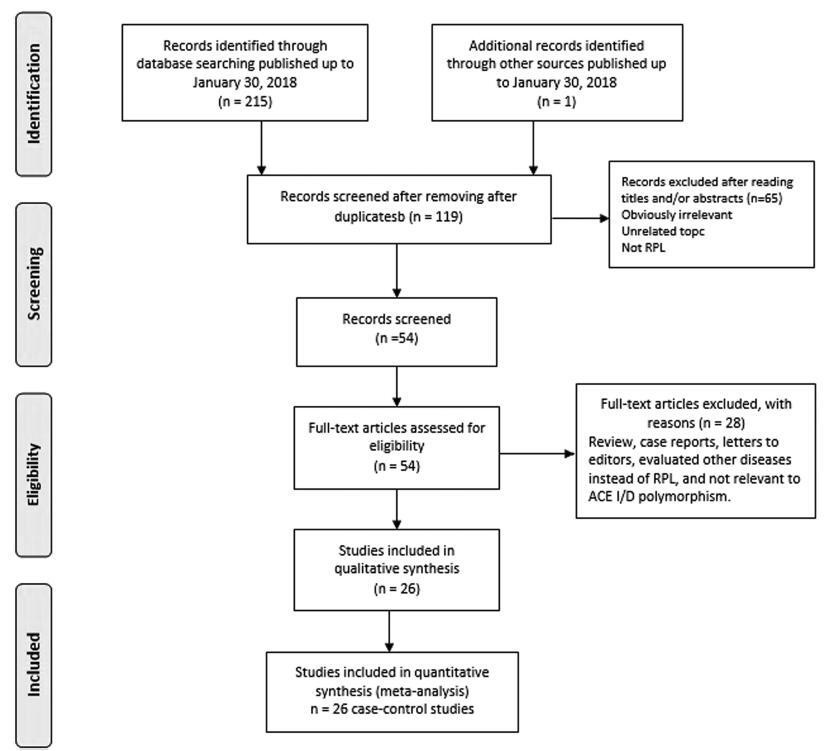
All studies published up to January 30, 2018 on the association of ACE I/D polymorphism with RPL were identified by searching the PubMed, Web of Knowledge, and Google scholar databases.
A total of 26 case-control studies with 3,140 RPL cases and 3,370 controls were included in themeta-analysis. Overall, there was a significant association between ACE I/D polymorphism and RPL risk under the allele model (I versus D: odds ratio [OR] = 0.538, 95% confidence interval [CI] = 0.451-0.643, p 0.001), the homozygote model (II versus DD: OR = 0.766, 95% CI = 0.598-0.981, p = 0.035) and the recessive model (II versus ID + DD: OR = 0.809, 95% CI = 0.658-0.994, p = 0.044). Subgroup analysis by ethnicity showed that there was a significant association between ACE I/D polymorphism and increased risk of RPL in Caucasian and West-Asian populations, but not in East-Asians. When stratified by number of recurrent miscarriages (RMs), a significant association between ACE I/D polymorphism and increased risk of RPL was detected in the group of studies with ≥ 2 RMs, but not in studies with ≥ 3 RMs.
Themeta-analysis suggests that ACE I/D polymorphism is associated with increased risk of RPL. The ACE I/D polymorphism may be a risk factor for RPL in Caucasian and West-Asian populations, but not in East-Asians.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):631-641
Previous studies investigating the association between angiotensin-converting enzyme (ACE) gene insertion/deletion (I/D) polymorphism and recurrent pregnancy loss (RPL) risk has provided inconsistent results. The aim of our study was to assess the association between the ACE I/D polymorphism and risk of RPL.
All studies published up to January 30, 2018 on the association of ACE I/D polymorphism with RPL were identified by searching the PubMed, Web of Knowledge, and Google scholar databases.
A total of 26 case-control studies with 3,140 RPL cases and 3,370 controls were included in themeta-analysis. Overall, there was a significant association between ACE I/D polymorphism and RPL risk under the allele model (I versus D: odds ratio [OR] = 0.538, 95% confidence interval [CI] = 0.451-0.643, p 0.001), the homozygote model (II versus DD: OR = 0.766, 95% CI = 0.598-0.981, p = 0.035) and the recessive model (II versus ID + DD: OR = 0.809, 95% CI = 0.658-0.994, p = 0.044). Subgroup analysis by ethnicity showed that there was a significant association between ACE I/D polymorphism and increased risk of RPL in Caucasian and West-Asian populations, but not in East-Asians. When stratified by number of recurrent miscarriages (RMs), a significant association between ACE I/D polymorphism and increased risk of RPL was detected in the group of studies with ≥ 2 RMs, but not in studies with ≥ 3 RMs.
Themeta-analysis suggests that ACE I/D polymorphism is associated with increased risk of RPL. The ACE I/D polymorphism may be a risk factor for RPL in Caucasian and West-Asian populations, but not in East-Asians.


Search
Search in:
breast breast cancer Breast neoplasms Cesarean section Endometriosis infertility Maternal mortality Menopause Obesity Polycystic ovary syndrome Postpartum period Pregnancy Pregnancy complications Prenatal care prenatal diagnosis Quality of life Risk factors Ultrasonography Uterine cervical neoplasms Women’s health
