Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo71
09-04-2024
To conduct a systematic review of external validation studies on the use of different Artificial Intelligence algorithms in breast cancer screening with mammography.
Our systematic review was conducted and reported following the PRISMA statement, using the PubMed, EMBASE, and Cochrane databases with the search terms “Artificial Intelligence,” “Mammography,” and their respective MeSH terms. We filtered publications from the past ten years (2014 – 2024) and in English.
A total of 1,878 articles were found in the databases used in the research. After removing duplicates (373) and excluding those that did not address our PICO question (1,475), 30 studies were included in this work.
The data from the studies were collected independently by five authors, and it was subsequently synthesized based on sample data, location, year, and their main results in terms of AUC, sensitivity, and specificity.
It was demonstrated that the Area Under the ROC Curve (AUC) and sensitivity were similar to those of radiologists when using independent Artificial Intelligence. When used in conjunction with radiologists, statistically higher accuracy in mammogram evaluation was reported compared to the assessment by radiologists alone.
AI algorithms have emerged as a means to complement and enhance the performance and accuracy of radiologists. They also assist less experienced professionals in detecting possible lesions. Furthermore, this tool can be used to complement and improve the analyses conducted by medical professionals.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):480-488
10-09-2023
To present the update of the recommendations of the Brazilian College of Radiology and Diagnostic Imaging, the Brazilian Society of Mastology and the Brazilian Federation of Associations of Gynecology and Obstetrics for breast cancer screening in Brazil.
Scientific evidence published in Medline, EMBASE, Cochrane Library, EBSCO, CINAHL and Lilacs databases between January 2012 and July 2022 was searched. Recommendations were based on this evidence by consensus of the expert committee of the three entities.
Annual mammography screening is recommended for women at usual risk aged 40–74 years. Above 75 years, it should be reserved for those with a life expectancy greater than seven years. Women at higher than usual risk, including those with dense breasts, with a personal history of atypical lobular hyperplasia, classic lobular carcinoma in situ, atypical ductal hyperplasia, treatment for breast cancer or chest irradiation before age 30, or even, carriers of a genetic mutation or with a strong family history, benefit from complementary screening, and should be considered individually. Tomosynthesis is a form of mammography and should be considered in screening whenever accessible and available.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):871-877
06-06-2022
This study aimed to evaluate the diagnostic profile of breast cancer cases during the coronavirus disease 2019 (COVID-19) pandemic compared with the previous year.
It is a retrospective study of cases diagnosed by a reference service in the public health system of Campinas, SP, Brazil. Two periods were analyzed: March to October 2019 (preCOVID period) and March to October 2020 (COVID-period). All women diagnosed during the periods were included. The Chi-Squared or Fisher exact and Mann-Whitney tests were used.
In the preCOVID and COVID periods, breast cancers were diagnosed, respectively, in 115 vs 59 women, and the mean ages at diagnosis were 55 and 57 years (p = 0.339). In the COVID period, the family history of breast cancer was more observed (9.6% vs 29.8%, p < 0.001), cases were more frequently symptomatic (50.4% vs 79.7%, p < 0.001) and had more frequently palpable masses (56.5% vs 79.7%, p = 0.003). In symptomatic women, the mean number of days from symptom to mammography were 233.6 (458.3) in 2019 and 152.1 (151.5) in 2020 (p = 0.871). Among invasive tumors, the proportion of breast cancers in stages I and II was slightly higher in the COVID period, although not significantly (76.7% vs 82.4%, p = 0.428). Also in the COVID period, the frequency of luminal A-like tumors was lower (29.2% vs 11.8%, p = 0.018), of triple-negative tumors was twice as high (10.1% vs 21.6%, p = 0.062), and of estrogen receptor-positive tumors was lower (82.2% vs 66.0%, p = 0.030).
During the COVID-19 pandemic, breast cancer diagnoses were reduced. Cases detected were suggestive of a worse prognosis: symptomatic women with palpable masses and more aggressive subtypes. Indolent tumors were those more sensitive to the interruption in screening.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):491-493
08-01-2018
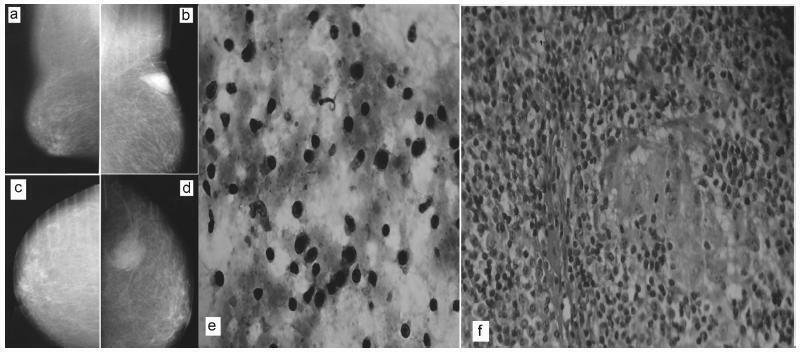
There are rare benign diseases that can mimic malignant breast neoplasms in the clinical exam and in mammography. We evaluated the contribution of an accessible procedure to most clinicians, the fine-needle aspiration cytology, to identify a rare mimicker of malignant breast neoplasms. A type 2 diabetic 85-year-old female presented with a 6-month history of a left breast lump. The physical exam and mammography were compatible with breast cancer. Nevertheless, after fine-needle aspiration cytology, the diagnosis was plasma cellmastitis. Once this rare diagnosis was established, the tumor was extirpated, and the final histologic diagnosis corroborated chronic plasma cellmastitis. The patient’s postoperative evolution was uneventful, and no other treatment was needed. Fine-needle aspiration cytology could be a valuable tool to identify rare mimickers of malignant breast neoplasms.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):239-245
05-01-2016
to evaluate the agreement between the clinical and pathological stagings of breast cancer based on clinical and molecular features.
this was a cross-sectional study, in which clinical, epidemiological and pathological data were collected from 226 patients who underwent surgery at the Prof. Dr. José Aristodemo Pinotti Women's Hospital (CAISM/Unicamp) from January 2008 to September 2010. Patients were staged clinically and pathologically, and were classified as: understaged, when the clinical staging was lower than the pathological staging; correctly staged, when the clinical staging was the same as the pathological one; and overstaged, when the clinical staging was greater than the pathological staging.
understaged patients were younger (52.2 years; p < 0.01) and more symptomatic at diagnosis (p = 0.04) when compared with correctly or overstaged patients. Clinicopathological surrogate subtype, menopausal status, parity, hormone replace therapy and histology were not associated with differences in staging. Women under 57 years of age were clinically understaged mainly due to underestimation of T ( tumor staging) (p < 0.001), as were the premenopausal women (p < 0.01). Patients whose diagnosis was made due to clinical complaints, and not by screening, were clinically understaged due to underestimation of N (lymph nodes staging) (p < 0.001).
the study shows that the clinicopathological surrogate subtype is not associated with differences in staging, while younger women diagnosed because of clinical complaints tend to have their breast tumors understaged during clinical evaluation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):112-116
02-01-2016
Lobular carcinoma in situ (LCIS) is associated with an increased risk of breast cancer and accounts for 1 to 2% of all breast cancers. LCIS diagnosis currently remains one of the major identifiable risk factors for subsequent breast cancer development. Imaging methods are becoming increasingly sensitive, and the consequent detection of small lesions and subtle abnormalities increases the chance of detection of in situ and invasive carcinomas, leading to a reduction in mortality. This report describes a case of a palpable complaint with abnormal imaging findings, including a solid LCIS mass.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(7):315-319
07-29-2014
DOI 10.159/S0100-720320140004977
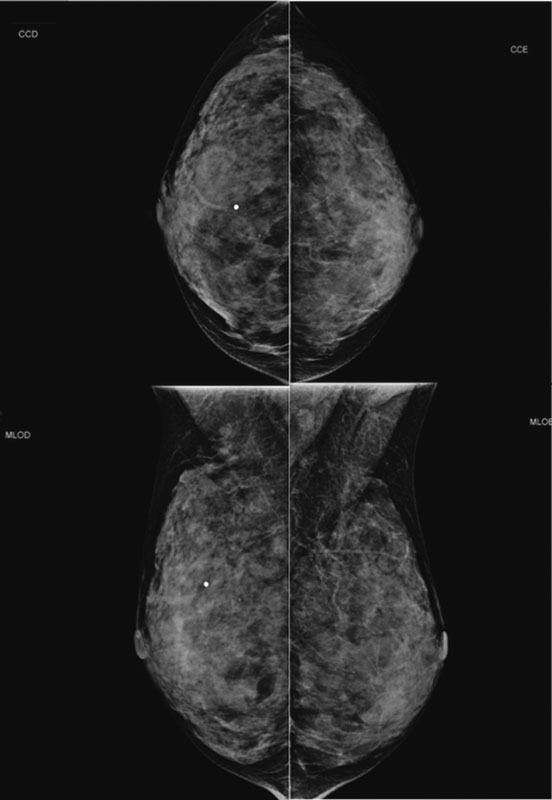
To analyze associations between mammographic arterial mammary calcifications in menopausal women and risk factors for cardiovascular disease.
This was a cross-sectional retrospective study, in which we analyzed the mammograms and medical records of 197 patients treated between 2004 and 2005. Study variables were: breast arterial calcifications, stroke, acute coronary syndrome, age, obesity, diabetes mellitus, smoking, and hypertension. For statistical analysis, we used the Mann-Whitney, χ2 and Cochran-Armitage tests, and also evaluated the prevalence ratios between these variables and mammary artery calcifications. Data were analyzed with the SAS version 9.1 software.
In the group of 197 women, there was a prevalence of 36.6% of arterial calcifications on mammograms. Among the risk factors analyzed, the most frequent were hypertension (56.4%), obesity (31.9%), smoking (15.2%), and diabetes (14.7%). Acute coronary syndrome and stroke presented 5.6 and 2.0% of prevalence, respectively. Among the mammograms of women with diabetes, the odds ratio of mammary artery calcifications was 2.1 (95%CI 1.0-4.1), with p-value of 0.02. On the other hand, the mammograms of smokers showed the low occurrence of breast arterial calcification, with an odds ratio of 0.3 (95%CI 0.1-0.8). Hypertension, obesity, diabetes mellitus, stroke and acute coronary syndrome were not significantly associated with breast arterial calcification.
The occurrence of breast arterial calcification was associated with diabetes mellitus and was negatively associated with smoking. The presence of calcification was independent of the other risk factors for cardiovascular disease analyzed.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(4):191-197
07-02-2010
DOI 10.1590/S0100-72032010000400007
PURPOSE: to assess compliance with the recommendations for opportunistic breast cancer screening by mammography. METHODS: 460 women from the town of Taubaté, São Paulo, Brazil, were followed-up prospectively after the index mammography, 327 of them attended by the public health system and 133 by the private system. We evaluated the prevalence of mammography repetition, the adherence rates and predictive factors associated with the current recommendations of mammographic screening. The association of the outcomes with the independent variables was studied by obtaining the risk rates (RR) and the respective 95% confidence intervals (95%CI). The adjusted prevalence rates were calculated by the COX regression model. RESULTS: although more than 90% of the studied women repeated the mammography at least once, the rate of correct compliance with the recommendations of mammographic screening, with repetition of the procedure every 24 months, was low (about 30% of the study sample). The preditive factors associated with compliance with mammographic screening were related to the unequal access to public or private healthcare services (RR=1.77; 95%CI=1.26-2.48) and to previous screening (RR=3.07; 95%CI=1.86-5.08). CONCLUSION: we concluded that compliance with the recommendations of opportunistic mammographic screening for breast cancer was low in both studied population segments.