-
Original Article
Systemic inflammatory indices as a non-invasive grading modality for endometriosis: a comparative study versus exploratory laparoscopy
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo84
12-04-2024
Summary
Original ArticleSystemic inflammatory indices as a non-invasive grading modality for endometriosis: a comparative study versus exploratory laparoscopy
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo84
12-04-2024Views172See moreAbstract
Objective:
Included evaluation of the possibility of using the systemic inflammatory indices for preoperative screening for the presence and severity of endometriosis (EM) in comparison to the findings of the exploratory laparoscopy
Methods:
88 women with clinical manifestations suggestive of EM were evaluated clinically and by US and gave blood samples for estimation of serum cancer antigen-125 (CA125), platelet and total and differential leucocytic counts for calculation of inflammatory indices; the Systemic Immune-Inflammation index, the Systemic Inflammation Response Index (SIRI), the Neutrophil-Lymphocyte ratio (NLR), the Neutrophil-Monocyte ratio, the Neutrophil-Platelet ratio and the Platelet-Lymphocyte ratio. Then, patients were prepared to undergo laparoscopy for diagnosis and staging.
Results:
Laparoscopy detected EM lesions in 63 patients; 27 of stage I-II and 36 of stage III-IV. Positive laparoscopy showed significant relation with US grading, high serum CA125 levels, platelet and inflammatory cell counts and indices. Statistical analyses defined high SIRI and NLR as the significant predictors for positive laparoscopy and high serum CA125 and NLR as the most significant predictors for severe EM (stage III-IV) on laparoscopy
Conclusion:
The intimate relation between EM and inflammation was reflected systematically as high levels of blood cellular components, but indices related to neutrophil especially NLR and SIRI showed highly significant relation to the presence and severity of EM and might be used as routine, cheap and non-invasive screening test before exploratory laparoscopy to guide the decision-making.
-
Original Article
The impact of surgical treatment for deep endometriosis: metabolic profile, quality of life and psychological aspects
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo42
06-27-2024
Summary
Original ArticleThe impact of surgical treatment for deep endometriosis: metabolic profile, quality of life and psychological aspects
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo42
06-27-2024Views196Abstract
Objective
To evaluate the effects of surgical treatment of deep endometriosis on the metabolic profile, quality of life and psychological aspects.
Methods
Prospective observational study, carried out with women of reproductive age diagnosed with deep endometriosis, treated in a specialized outpatient clinic, from October/2020 to September/2022, at a University Hospital in Fortaleza - Brazil. Standardized questionnaires were applied to collect data on quality of life and mental health, in addition to laboratory tests to evaluate dyslipidemia and dysglycemia, at two moments, preoperatively and six months after surgery. The results were presented using tables, averages and percentages.
Results
Thirty women with an average age of 38.5 years were evaluated. Seven quality of life domains showed improved scores: pain, control and impotence, well-being, social support, self-image, work life and sexual relations after surgery (ES ≥ 0.80). There was an improvement in mental health status with a significant reduction in anxiety and depression postoperatively. With the metabolic profile, all average levels were lower after surgery: total cholesterol 8.2% lower, LDL 12.8% lower, triglycerides 10.9% lower, and fasting blood glucose 7.3% lower (p < 0.001).
Conclusion
Surgical treatment of deep endometriosis improved the quality of life and psychological aspects of patients. The lipid profile of patients after laparoscopy was favorable when compared to the preoperative lipid profile.
Key-words AnxietyDepressionEndometriosisInflammationLaparoscopyLipidsMental healthPelvic painQuality of lifesurveys and questionnairesSee more -
Original Article
Assessing Endoscopic Suture Performance of Gynecology and Obstetrics Residents Following Methodic Training
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(10):603-608
12-11-2023
Summary
Original ArticleAssessing Endoscopic Suture Performance of Gynecology and Obstetrics Residents Following Methodic Training
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(10):603-608
12-11-2023Views163See moreAbstract
Objective
To evaluate the performance of residents in gynecology and obstetrics before and after practicing laparoscopic sutures, to establish when the training shows the best results, in addition to comparing whether being in different years of residency influences this progression.
Methods
A prospective cohort study involving 32 medical residents evaluated with a pretest to establish their previous knowledge in laparoscopic suture. This test consisted of knotting two wires, one made of polypropylene and the other of polyglactin, with a blocking sequence of five semi-knots. We set a 30-minute limit to complete the task. Then, the residents held four training meetings, focusing on suture, Gladiator rule, knot, and symmetries, in addition to executing blocking sequences. A second test to establish progress was performed.
Results
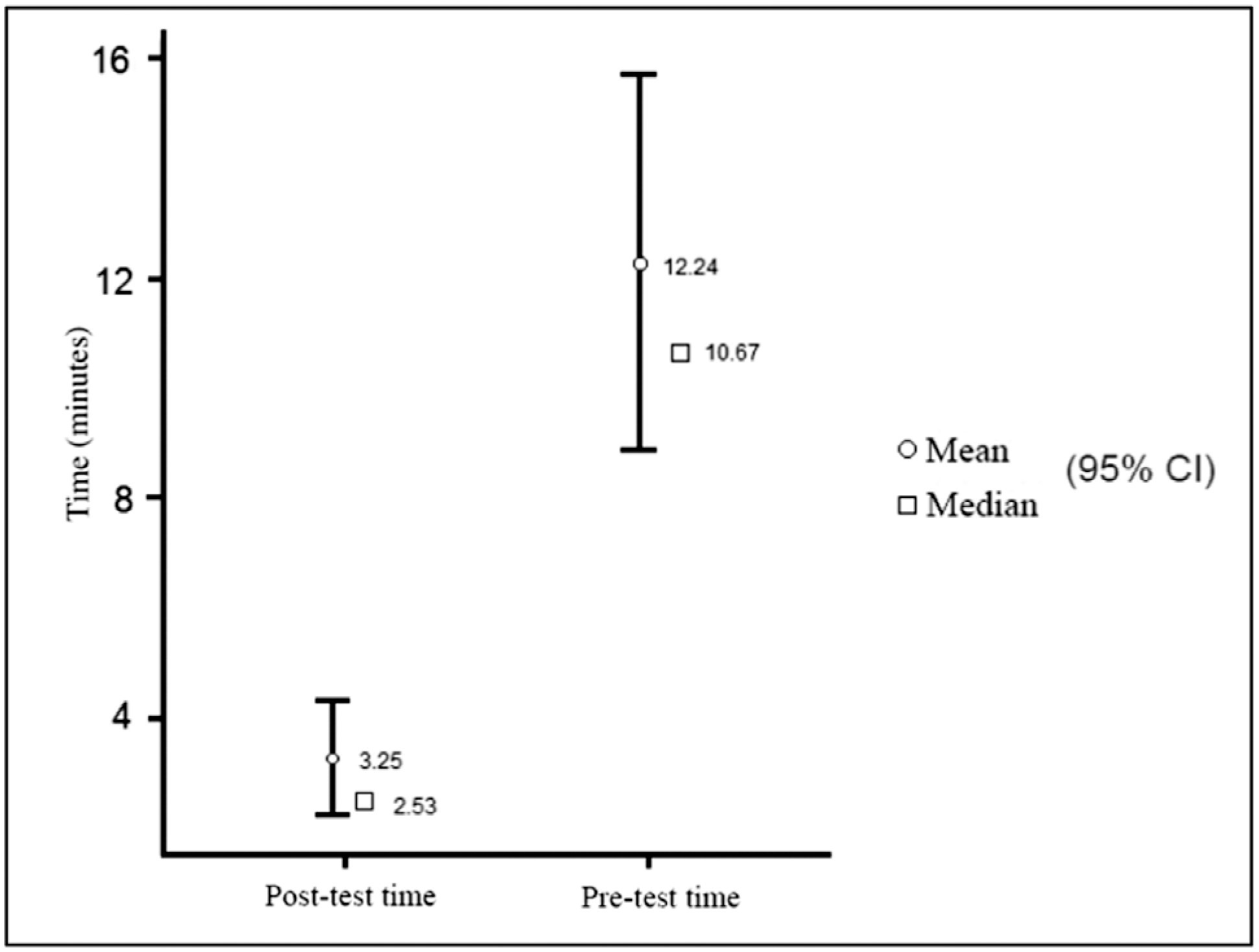
Regarding the time spent to make the stiches using polyglactin wire, a statistically significant time improvement (p< 0.01) was observed, with a 10.67-minute pretraining median (mean 12.24 minutes) and a 2.53-minute posttraining median (mean 3.25 minutes). Regarding the stitches with polypropylene wire, a statistically significant time improvement (p< 0.05) was also observed, with a 9.38-minute pretraining median (mean 15.43 minutes) and a 3.65-minute posttraining median (mean 4.54 minutes). A total of 64.2% of the residents had been able to make the knot with polypropylene previously. One hundred percent were able to complete the task in the posttest.
Conclusion
Model training using the Gladiator rule for laparoscopic suture improves the knotting time with statistically similar performance, regardless of the year of residency, after systematic training.
-
Original Article
Postoperative Complications and Stoma Rates After Laparoscopic Resection of Deep Infiltrating Endometriosis with Bowel Involvement
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1040-1046
01-23-2022
Summary
Original ArticlePostoperative Complications and Stoma Rates After Laparoscopic Resection of Deep Infiltrating Endometriosis with Bowel Involvement
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1040-1046
01-23-2022Views103See moreAbstract
Objective
The purpose was to assess the rates of postoperative complications and the need of temporary stoma of laparoscopic surgical treatment for bowel endometriosis in a referral center.
Methods
The surgical indication, type of operation, operative time, length of hospital stay, need for a temporary stoma, rate of conversion to open surgery, postoperative complications were evaluated.
Results
One-hundred and fifty patients were included. The average duration of surgery was significantly longer for segmental resection (151 minutes) than for disc excision (111.5 minutes, p < 0.001) and shaving (96.8 minutes, p < 0.001). Patients with segmental resection had longer postoperative lengths of hospital stay (1.87 days) compared with patients with disc excision (1.43 days, p < 0.001) and shaving (1.03 days, p < 0.001). A temporary stoma was performed in 2.7% of patients. Grade II and III postoperative complications occurred in 6.7% and 4.7% patients, respectively.
Conclusion
Laparoscopic intestinal resection has an acceptable postoperative complication rate and a low need for a temporary stoma.
-
Review Article
Gynecological Surgery and COVID-19: What is the Impact and How Should I Manage it?
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):415-419
08-26-2020
Summary
Review ArticleGynecological Surgery and COVID-19: What is the Impact and How Should I Manage it?
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):415-419
08-26-2020Views183See moreAbstract
It is estimated that around 28 million surgeries will be postponed or canceled worldwide as a result of this pandemic, causing a delay in the diagnosis and treatment of more than 2 million cancer cases. In Brazil, both the National Health Agency (ANS) and National Health Surveillance Agency (ANVISA) advised the postponement of elective and non-essential surgeries, causing a considerable impact on the number of surgical procedures that decreased by 33.4% in this period. However, some women need treatment for various gynecological diseases that cannot be postponed. The purpose of this article is to present recommendations on surgical treatment during the COVID-19 pandemic.
-
Original Articles
Intraoperative Ultrasound Leads to Conservative Management of Benign Ovarian Tumors: A Retrospective, Single-Center Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(11):673-678
12-20-2019
Summary
Original ArticlesIntraoperative Ultrasound Leads to Conservative Management of Benign Ovarian Tumors: A Retrospective, Single-Center Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(11):673-678
12-20-2019Views121See moreAbstract
Objective
To evaluate whether the use of intraoperative ultrasound leads to more conservative surgeries for benign ovarian tumors.
Methods
Women who underwent surgery between 2007 and 2017 for benign ovarian tumors were retrospectively analyzed. The women were classified into two groups: those who underwent intraoperative ultrasound (group A) and those who did not (group B). In group A, minimally-invasive surgery was performed for most patients (a specific laparoscopic ultrasound probe was used), and four patients were submitted to laparotomy (a linear ultrasound probe was used). The primary endpoint was ovarian sparing surgery (oophoroplasty).
Results
Among the 82 cases identified, only 36 met the inclusion criteria for the present study. Out of these cases, 25 underwent intraoperative ultrasound, and 11 did not. There were no significant differences in arterial hypertension, diabetes, smoking history, and body mass index for the two groups (p=0.450). Tumor diameter was also similar for both groups, ranging from 1 cm to 11 cm in group A and from 1.3 cm to 10 cm in group B (p=0.594). Tumor histology confirmed mature teratomas for all of the cases in group B and for 68.0% of the cases in group A. When the intraoperative ultrasound was performed, a more conservative surgery was performed (p<0.001).
Conclusion
The use of intraoperative ultrasound resulted in more conservative surgeries for the resection of benign ovarian tumors at our center.
-
Original Article
Laparoscopic Approach in Surgical Staging of Endometrial Cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):306-311
06-27-2019
Summary
Original ArticleLaparoscopic Approach in Surgical Staging of Endometrial Cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):306-311
06-27-2019Views147See moreAbstract
Objective
To compare laparoscopy with laparotomy for surgical staging of endometrial cancer.
Methods
A cohort of women with preoperative diagnosis of endometrial cancer who underwent surgical staging was retrospectively evaluated. The main study end points were: morbidity and mortality, hospital length of stay, perioperative adverse events and recurrence rate. Data analysis was performed with the software SPSS v25 (IBM Corp., Armonk, NY, USA), categorical variables using a Chi-square and Fisher test, and continuous variables using the Student t-test.
Results
Atotal of 162 patientswere analyzed. 138 patientsmet the inclusion criteria, 41of whom underwent staging by laparoscopy and 97 by laparotomy. Conversions from laparoscopy to laparotomy happened in 2 patients (4.9%) and were secondary to technical difficulties and poor exposure. Laparoscopy had fewer postoperative adverse events when compared with laparotomy (7.3% vs 23.7%, respectively; p = 0.005), but similar rates of intraoperative complications, despite having a significantly longer operative time (median, 175 vs 130 minutes, respectively; p < 0.001). Hospital stay was significantly lower in laparoscopy versus laparotomy patients (median, 3 vs 7 days, respectively; p < 0.001). No difference in recurrence or mortality rates were observed.
Conclusion
Laparoscopic surgical staging for endometrial cancer is feasible and safe. Patients have lower postoperative complication rates and shorter hospital stays when compared with the approach by laparotomy.


