Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(8):790-796
This systematic review aims at describing the prevalence of urinary and sexual symptoms among women who underwent a hysterectomy for cervical cancer.
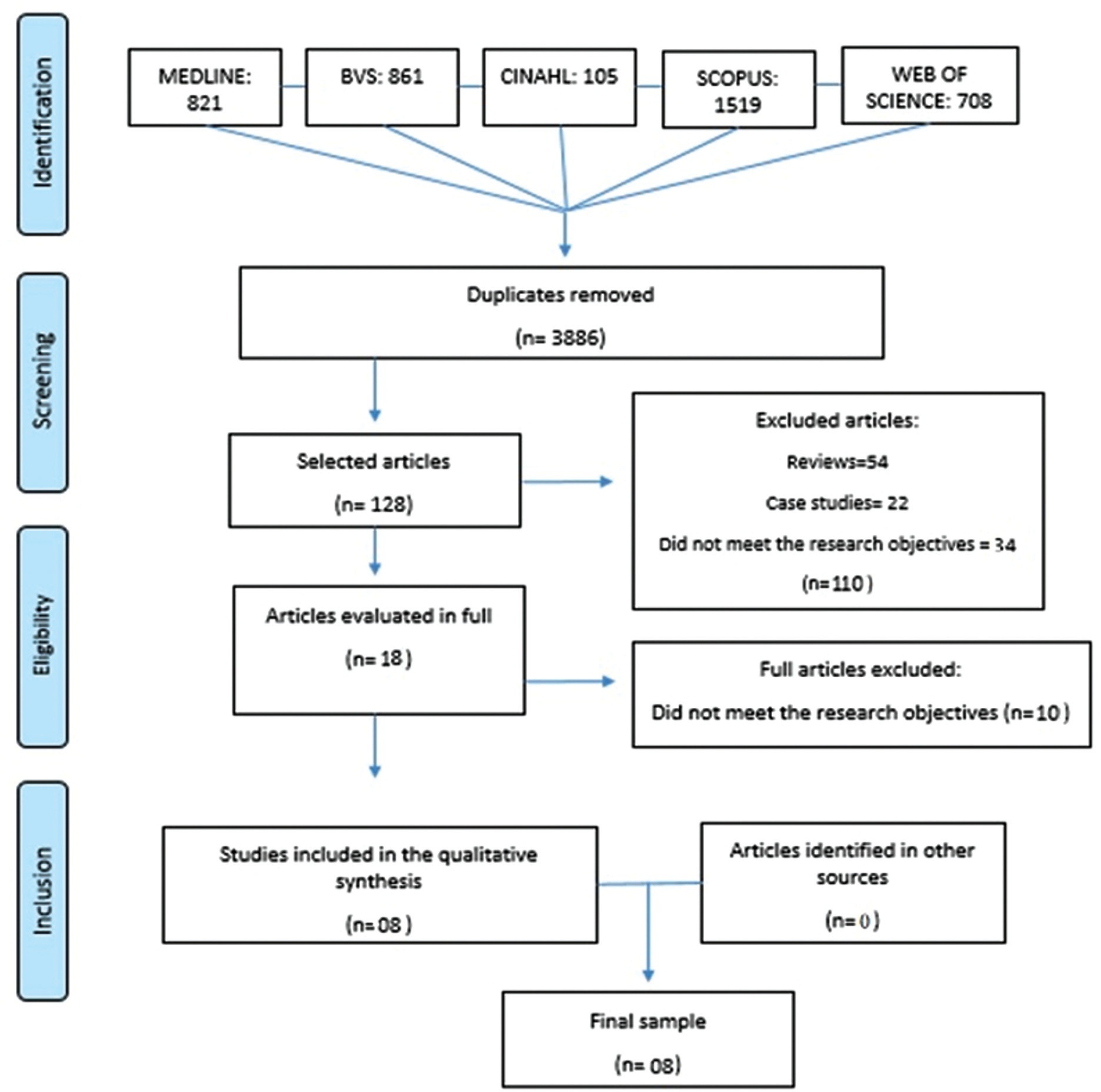
A systematic search in six electronic databases was performed, in September 2019, by two researchers. The text search was limited to the investigation of prevalence or occurrence of lower urinary tract symptoms (LUTS) and sexual dysfunctions in women who underwent a hysterectomy for cervical cancer. For search strategies, specific combinations of terms were used.
A total of 8 studies, published between 2010 and 2018, were included in the sample. The average age of the participants ranged from 40 to 56 years, and the dysfunctions predominantly investigated in the articles were urinary symptoms (n= 8). The rates of urinary incontinence due to radical abdominal hysterectomy ranged from 7 to 31%. The same dysfunction related to laparoscopic radical hysterectomy varied from 25 to 35% and to laparoscopic nerve sparing radical hysterectomy varied from 25 to 47%. Nocturia ranged from 13%, before treatment, to 30%, after radical hysterectomy. The prevalence rates of dyspareunia related to laparoscopic radical hysterectomy and laparoscopic nerve sparing radical hysterectomy ranged from 5 to 16% and 7 to 19% respectively. The difficulty in having orgasm was related to laparoscopic radical hysterectomy (10 to 14%) and laparoscopic nerve sparing radical hysterectomy (9 to 19%).
Urinary and sexual dysfunctions after radical hysterectomy to treat cervical cancer are frequent events. The main reported disorders were urinary incontinence and dyspareunia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):311-316
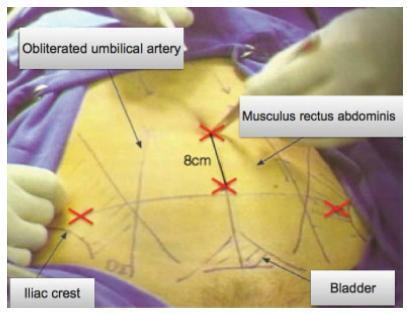
A cesarean scar pregnancy (CSP) is a scary and life-threatening complication of cesarean section (CS). Nevertheless, the incidence of CS is constantly growing. The CSP incidence is 0,15% of pregnancies after CS which represents 6,1% of all ectopic pregnancies in women with condition after CS. Therefore, it should be more present in the clinical daily routine. From mild nonspecific symptoms to hypovolemic shock, diagnosis and therapy must be performed quickly. With the progressive growth of the scar pregnancy, a uterine rupture involves the risk of severe bleeding, and an emergency hysterectomy could be necessary. Prolongation of pregnancy has been successful only in a few cases.We report 11 cases from our hospital in the past 10 years. In the discussion, treatment options of this complication with an increasing incidence, which is associated with serious morbidity and mortality, are presented based on the current literature. Treatment options include drug therapy, but also surgical or combined procedures with radiological intervention.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(5):266-271
To observe if the histopathological result of a conization performed after cervical adenocarcinoma in situ diagnosis is compatible with the histopathological analysis of a subsequent hysterectomy.
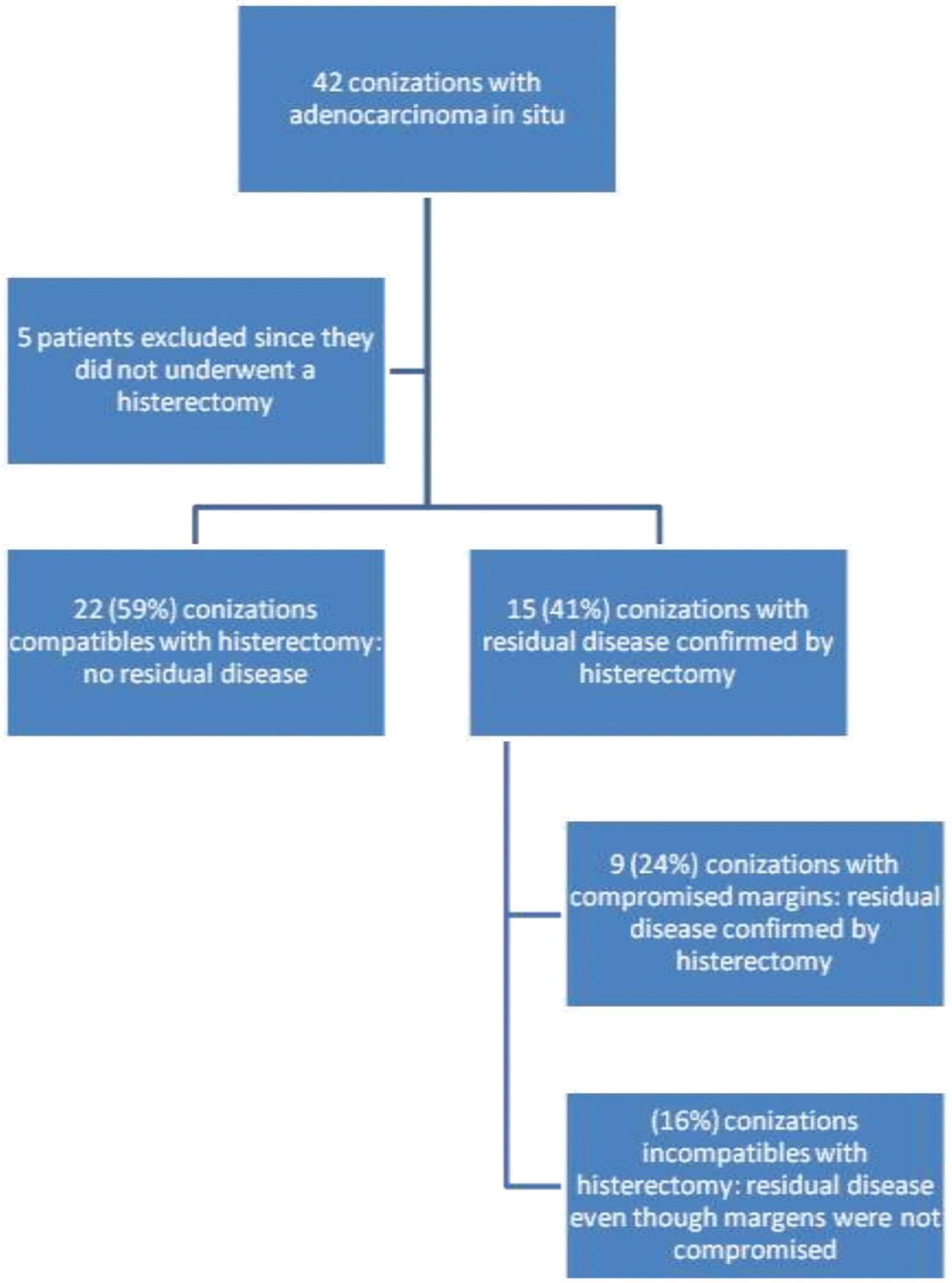
The present descriptive and observational research consisted of the analysis of the medical records of 42 patients who were diagnosed with in situ adenocarcinoma postconization. The analysis consisted of whether there was compatibility between the histopathological reports of conization and hysterectomy and if there was an association between adenocarcinoma in situ and another neoplasia (squamous disease). Interpretation of any immunohistochemistry reports obtained was also performed. In addition, clinical and epidemiological data were also analyzed.
A total of 42 conizations were performed, 33 (79%) were cold knife conizations and 9 (21%) were loop electrosurgical excision procedures (LEEPs). Of the patients analyzed, 5 (10%) chose not to undergo subsequent hysterectomy to preserve fertility or were < 25 years old. Out of the 37 patients with adenocarcinoma in situ who underwent subsequent hysterectomy, 6 (16%) presented with residual disease. This findingprovedincompatiblewiththe finding of the conizations, which had ruled out invasive cancer.
The prevalence of adenocarcinoma in situ increased in the past years. There is still a large part of the medical literature that advocates the use of conservative treatment for this disease, even though it is common knowledge that it is a multifocal disease. However, the majority of studies advocate that hysterectomy should remain the preferred treatment for women who have already completed their reproductive purpose.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):718-725
To evaluate the impact of systematic laparoscopic skills and suture training (SLSST) on the total laparoscopic hysterectomy intra- and postoperative outcomes in a Brazilian teaching hospital.
A cross-sectional observational study in which 244 charts of total laparoscopic hysterectomy (TLH) patients operated from 2008 to 2014 were reviewed. Patient-specific (age, parity, previous cesarean sections, abdominal surgeries and endometriosis) and surgery-related variables (hospital stay, operative time, uterine volume and operative complications) were analyzed in three different time-frame groups: 2008-09 (I-1) - TLHs performed by senior attending physicians; 2010-11 (I-2) - TLHs performed by residents before the implementation of the SLSST program; and 2012-14 (I-3) - TLHs performed by residents after the implementation of the SLSST program.
A total of 244 TLH patients (mean age: 45.93 years) were included: 24 (I-1), 55 (I-2), and 165 (I-3). The main indication for TLH was uterine myoma (66.4%). Group I-3 presented a decrease in surgical time compared to group I-2 (p=0.010). Hospital stay longer than 2 days decreased in group I-3 compared to group I-2 (p=0.010). Although we observed decreased uterine volume (154.2 cm3) in group I-2 compared to group I-1 (217.8 cm3) (p=0.030), logistic regression did not find any association between uterine volume and surgical time (p=0.103).
The total operative time for laparoscopic hysterectomy was significantly shorter in the group of patients (I-3) operated after the systematic laparoscopic skills and suture training was introduced in our hospital.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):306-311
To compare laparoscopy with laparotomy for surgical staging of endometrial cancer.
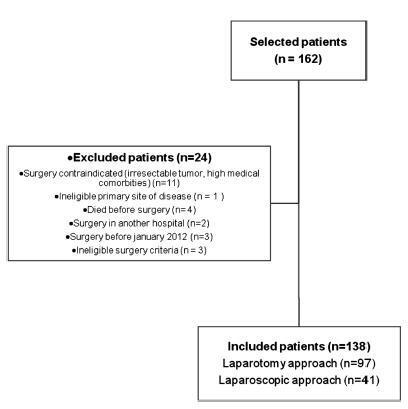
A cohort of women with preoperative diagnosis of endometrial cancer who underwent surgical staging was retrospectively evaluated. The main study end points were: morbidity and mortality, hospital length of stay, perioperative adverse events and recurrence rate. Data analysis was performed with the software SPSS v25 (IBM Corp., Armonk, NY, USA), categorical variables using a Chi-square and Fisher test, and continuous variables using the Student t-test.
Atotal of 162 patientswere analyzed. 138 patientsmet the inclusion criteria, 41of whom underwent staging by laparoscopy and 97 by laparotomy. Conversions from laparoscopy to laparotomy happened in 2 patients (4.9%) and were secondary to technical difficulties and poor exposure. Laparoscopy had fewer postoperative adverse events when compared with laparotomy (7.3% vs 23.7%, respectively; p = 0.005), but similar rates of intraoperative complications, despite having a significantly longer operative time (median, 175 vs 130 minutes, respectively; p < 0.001). Hospital stay was significantly lower in laparoscopy versus laparotomy patients (median, 3 vs 7 days, respectively; p < 0.001). No difference in recurrence or mortality rates were observed.
Laparoscopic surgical staging for endometrial cancer is feasible and safe. Patients have lower postoperative complication rates and shorter hospital stays when compared with the approach by laparotomy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(1):35-39
Robotic surgeries for cervical cancer have several advantages compared with lapa-rotomic or laparoscopic surgeries. Robotic single-site surgery has many advantages compared with the multiport approach, but its safety and feasibility are not established in radical oncologic surgeries. We report a case of a Federation of Gynecology and Obstetrics (FIGO) stage IB1 cervical carcinoma whose radical hysterectomy, sentinel lymph node mapping, and lymph node dissection were entirely performed by robotic single-site approach. The patient recovered very well, and was discharged from the hospital within 24 hours.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):530-535
DOI 10.1590/S0100-72032010001100003
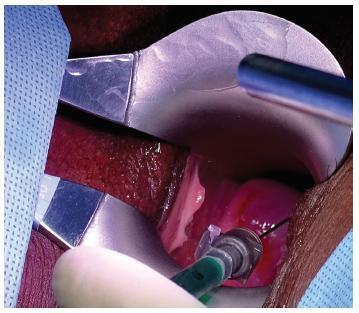
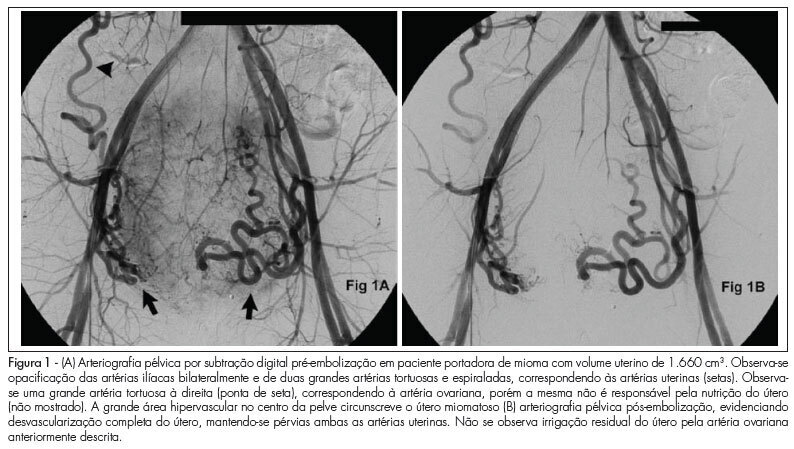
PURPOSE: to evaluate the effectiveness of uterine fibroid embolization (UFE) in patients with giant fibroids, with regard to both clinical outcomes and size reduction. METHODS: twenty-six patients with a mean age of 36.5 years, carrying symptomatic fibroids with a volume over 1,000 cm³, were referred for UFE. All patients had indication for percutaneous treatment. The procedures were performed under epidural anesthesia and sedation, using an institutional protocol. By unilateral femoral access, selective catheterization of uterine arteries and infusion of calibrated microspheres through microcatheter were carried out. Clinical evaluation was performed by means of regular outpatient gynecology consultation. All patients underwent magnetic resonance imaging (MRI) before the procedure and 15 patients underwent control MRI after 6 months. RESULTS: technical success was 100%. There was no complication related to the procedures. Mean uterine volume of the 15 patients studied was 1,401 cm³ before embolization (min 1,045 cm³, max 2,137 cm³) and 799 cm³ after 6 months (525 cm³ min, max. 1,604 cm³), resulting in a total reduction of 42.9%. Clinical improvement was observed in 25 of 26 patients. One woman with uterine volume of 1,098 cm³ who developed necrosis and partial fibroid expulsion underwent myomectomy. Another patient was submitted to myomectomy six months after the procedure because she wanted to become pregnant, despite partial fibroid size reduction. One patient with a uterine volume of 2,201 cm³ required a second intervention to achieve an adequate angiographic result. No patient underwent hysterectomy. On average, 9.2 microsphere syringes were used per patient. CONCLUSION: embolization of giant uterine fibroids is a feasible procedure with acceptable clinical and radiological outcomes. It can be considered an option for patients who desire to preserve the uterus, and it may serve as adjuvant therapy for high-risk myomectomy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(10):503-507
DOI 10.1590/S0100-72032009001000006
PURPOSE: to evaluate the impact of hysterectomy on the sexuality of women with uterine leiomyoma. METHODS: prospective study including 33 sexually active women, with ages from 35 to 50 years old, with orgasmic experience and with a fit stable partner. All the women were submitted to two instruments for the evaluation or their sexuality: Sexual Quotient - Female Version (SQF) and Sexual Satisfaction Inventory - Female Version (SSIF). Both instruments were applied by the same examiner, before and six months after the hysterectomy. RESULTS: the SQF has shown that 39.4% of the patients presented deterioration in the sexual intercourse, even though there has not been found an association between the SQF results before and after hysterectomy (χ2= 0.6; degree of freedom=12; p=0.05). The mean scores obtained after the application of the SSIF have shown significant deterioration in the following parameters: sexual satisfaction (p=0.03); expression of feminine sensuality (p=0.01); vaginismus/dyspareunia (p=0.02) and anorgasmia (p=0.04). CONCLUSIONS: it seems that hysterectomy has a negative impact on women's sexual life, with reports of decreased libido, arousal and orgasmic capacity.