-
Review Article06-03-2024
How can we reduce maternal mortality due to preeclampsia? The 4P rule
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo43
Abstract
Review ArticleHow can we reduce maternal mortality due to preeclampsia? The 4P rule
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo43
Views385See moreAbstract
In low and middle-income countries such as Brazil, most maternal deaths are related to hypertensive complications. Preeclampsia is the leading cause of maternal mortality and morbidity. Significant proportion is associated with the following factors: lack of identification of high-risk women, lack of adequate prevention, difficulty in maintaining a high-risk prenatal follow-up, delayed diagnosis, insecurity and low use of magnesium sulphate, delayed pregnancy interruption and lack of postpartum follow-up of these high-risk cases. Four major actions are proposed to minimize this alarming clinical picture and reduce the mortality rates due to preeclampsia, called the "4 P Rule" (Adequate Prevention – Vigilant Prenatal Care – Timely Delivery (Parturition) – Safe Postpartum). From this simple "rule" we can open a range of important processes and reminders that may help in the guidance of preeclampsia management.
-
Review Article06-20-2022
Renin-Angiotensin-Aldosterone System in Women Using Combined Oral Contraceptive: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(7):710-718
Abstract
Review ArticleRenin-Angiotensin-Aldosterone System in Women Using Combined Oral Contraceptive: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(7):710-718
Views344See moreAbstract
Objective
To describe the effects of combined oral contraceptives (COC) on the renin-angiotensin-aldosterone system (RAAS).
Conclusion
The findings of this study suggest that the COC promotes greater activation of the RAAS. Supporting the idea that its use is related to an increased risk of cardiovascular events, including systemic arterial hypertension.
-
Review Article04-25-2022
Diagnosis and Management of Preeclampsia: Suggested Guidance on the Use of Biomarkers
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):878-883
Abstract
Review ArticleDiagnosis and Management of Preeclampsia: Suggested Guidance on the Use of Biomarkers
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):878-883
Views287Abstract
Objective
It is a challenge to consider preeclampsia (PE) diagnosis and management in low and middle-income settings, where it represents a major public health concern. The placenta is the underlying cause of disease, and the plasma concentrations of proangiogenic and antiangiogenic factors released by the placenta can reflect the risks of disease progression. Antiangiogenic proteins, such as soluble fms-like tyrosine kinase 1 (sFlt-1), and proangiogenic, like placental growth factors (PlGF), are directly and inversely correlated with the disease onset, respectively.
Methods
Narrative review on the use of biomarkers (sFlt-1 to PlGF ratio) with a suggested guidance protocol.
Results
Key considerations on the use of biomarkers: the sFlt-1/PlGF ratio is mainly relevant to rule out PE between 20 and 36 6/7 weeks in cases of suspected PE; however, it should not replace the routine exams for the diagnosis of PE. The sFlt-1/PlGF ratio should not be performed after confirmed PE diagnosis (only in research settings). In women with suspected PE, sFlt-1/PlGF ratio < 38 can rule out the diagnosis of PE for 1 week (VPN = 99.3) and up to 4 weeks (VPN= 94.3); sFlt-1/PlGF ratio > 38 does not confirm the diagnosis of PE; however, it can assist clinical management. In cases of severe hypertension and/or symptoms (imminent eclampsia), hospitalization is imperative, regardless of the result of the sFlt-1/PlGF ratio.
Conclusion
The use of biomarkers can help support clinical decisions on the management of suspected PE cases, especially to rule out PE diagnosis, thus avoiding unnecessary interventions, especially hospitalizations and elective prematurity
Key-words Hypertensionplacental growth factorPreeclampsiapreterm preeclampsiasoluble fms-like tyrosine kinase 1See more -
Original Article01-24-2021
Preeclampsia and Gestational Hypertension: Biochemical and Antioxidant Features in Vitro Might Help Understand Different Outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):894-903
Abstract
Original ArticlePreeclampsia and Gestational Hypertension: Biochemical and Antioxidant Features in Vitro Might Help Understand Different Outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):894-903
Views169See moreAbstract
Objective
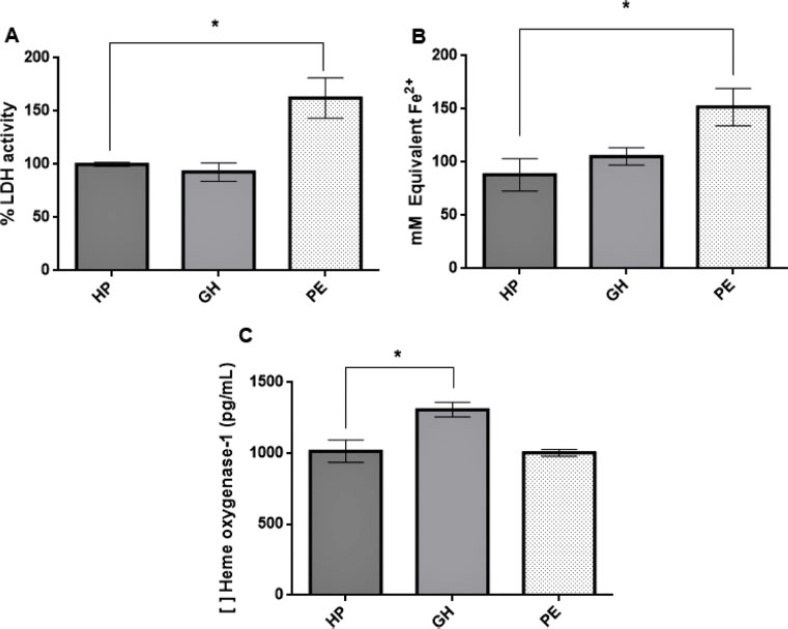
Gestational hypertension (GH) is characterized by increased blood pressure after the 20th gestational week; the presence of proteinuria and/or signs of end-organ damage indicate preeclampsia (PE). Heme oxygenase-1 (HO-1) is an antioxidant enzyme with an important role in maintaining endothelial function, and induction of HO-1 by certain molecules shows potential in attenuating the condition’s effects over endothelial tissue. HO-1 production can also be stimulated by potassium iodide (KI). Therefore, we evaluated the effects of KI over HO-1 expression in human umbilical vein endothelial cells (HUVECs) incubated with plasma from women diagnosed with GH or PE.
Methods
Human umbilical vein endothelial cells were incubated with a pool of plasma of healthy pregnant women (n = 12), pregnant women diagnosed with GH (n = 10) or preeclamptic women (n = 11)with or without the addition of KI for 24 hours to evaluate its effect on this enzyme expression. Analysis of variance was performed followed by Dunnet’s test for multiple comparisons between groups only or between groups with addition of KI (p ≤ 0.05).
Results
KI solution (1,000 µM) reduced HO-1 in the gestational hypertension group (p = 0.0018) and cytotoxicity in the preeclamptic group (p = 0.0143); treatment with KI reduced plasma cytotoxicity but did not affect the preeclamptic group’s HO-1 expression.
Conclusion
Our findings suggest that KI alleviates oxidative stress leading to decreased HO-1 expression; plasma from preeclamptic women did not induce the enzyme’s expression in HUVECs, and we hypothesize that this is possibly due to inhibitory post-transcriptional mechanisms in response to overexpression of this enzyme during early pregnancy.
-
Original Article04-22-2020
The Role of Ischemia-modified Albumin as a Biomarker in Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):133-139
Abstract
Original ArticleThe Role of Ischemia-modified Albumin as a Biomarker in Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):133-139
Views243See moreAbstract
Objective
Ischemia-modified albumin (IMA)is a modified type of albumin protein that is formed under oxidative stress. This study aims to compare the levels of serum IMA between normotensive and preeclamptic pregnancies and to evaluate the relationship between the severity of the disease.
Methods
A total of 90 pregnant women aged between 18 and 45 years participated in this cross-sectional study. The levels of serum IMA were measured by enzyme-linked immunosorbent assay in 30 preeclamptic pregnant women with the severe signs of the disease, 30 preeclamptic pregnant women, and 30 normotensive pregnant women.. The study was designed as a cross-sectional clinical study.
Results
When the demographic characteristics were examined, statistically significant differences were found between the groups in terms of age, gestational week at birth and blood pressure. Age was higher in the preeclampsia with signs of severity group than in the normotensive group (p = 0.033). Pregnancy week was significantly the lowest in the preeclampsia with the severity signs group (p = 0.004). In normotensive patients, IMA levels were lower than in the preeclampsia groups (p = 0.001) but there was no significant difference in terms of severity of disease (p = 0.191). According to laboratory data; only the creatinine level was significantly different between the groups.
Conclusion
The levels of serum IMA were higher in patients with preeclampsia than in healthy pregnancies. However, there was no significant correlation in terms of preeclampsia severity; more extensive, prospective and long-term studies are needed.
-
Original Article08-15-2019
Pregnancy Among Women with Kidney Transplantation: A 20-Years Single-Center Registry
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(7):419-424
Abstract
Original ArticlePregnancy Among Women with Kidney Transplantation: A 20-Years Single-Center Registry
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(7):419-424
Views160See moreAbstract
Objective
To assess maternal and perinatal outcomes in pregnancies after kidney transplantation in a tertiary center in Brazil.
Methods
Retrospective cohort of pregnancies in women with kidney transplantation at the Universidade Estadual de Campinas, from January 1995 until December 2017. Medical charts were reviewed, andmaternal and perinatal outcomes were described as means and frequencies. Renal function and blood pressure were evaluated during pregnancy and postpartum.
Results
A total of 22 women had at least 1 pregnancy during the considered timeinterval, and 3 of them had > 1 pregnancy, totalizing 25 pregnancies. The mean age at transplantation was of 24.6 ± 4.2 years old, and the mean time interval until pregnancy was of 67.8 ± 46.3months. Themost frequent complication during pregnancywas hypertension, which affected 11 (64.7%)women. The gestational age at delivery was 34.7 ± 4weeks, and 47% of these pregnancies were preterm (< 37 weeks). A total of 88.2% of the women delivered by cesarean section. Renal function, measured by serum creatinine, remained stable during pregnancy, and the systolic blood pressure increased significantly, while the diastolic blood pressure did not differ during pregnancy.
Conclusion
Pregnancy after kidney transplantation is a rare event. Pre-eclampsia and prematurity were frequent complications, and cesarean section rates were very high. A specialized antenatal and postpartum care with a multiprofessional approach and continuous monitoring of graft function are essential for the early diagnosis of complications and improved outcomes.
-
Original Article06-19-2019
Maternal Weight Variation in Different Intrauterine Environments: An Important Role of Hypertension
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):220-229
Abstract
Original ArticleMaternal Weight Variation in Different Intrauterine Environments: An Important Role of Hypertension
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):220-229
Views226See moreAbstract
Objective
Different intrauterine environments may influence the maternal prepregnancy body weight (BW) variation up to 6 months postpartum. The objective of the present study was to verify the association of sociodemographic, obstetric, nutritional, and behavioral factors with weight variation in women divided into four groups: hypertensive (HM), diabetic (DM), smokers (SM), and control mothers (CM).
Methods
It was a convenience sample of 124 postpartum women recruited from 3 public hospitals in the city of Porto Alegre, state of Rio Grande do Sul, Brazil, between 2011 and 2016.Multiple linear regressions and generalized estimating equations (GEE) were conducted to identify the factors associated with maternal weight variation. For all GEE, the maternal weight measurements were adjusted for maternal height, parity, educational level, and the type of delivery, and 3 weight measurements (prepregnancy, preceding delivery, and 15 days postpartum) were fixed.
Results
A hierarchical model closely associated the maternal diagnosis of hypertension and a prepregnancy body mass index (BMI) classified as overweight with maternal weight gain measured up to the 6th month postpartum (the difference between the maternal weight at 6months postpartum and the prepregnancy weight). These results showed that the BW of the HM group and of overweight women increased ~ 5.2 kg 6 months postpartum, compared with the other groups. Additionally, women classified as overweight had a greater BW variation of 3.150 kg.
Conclusion
This evidence supports the need for specific nutritional guidelines for gestational hypertensive disorders, as well as great public attention for overweight women in the fertile age.
-
Original Article04-01-2015
Podocyturia in pregnant women with chronic hypertension may predict kidney injury?
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):172-177
Abstract
Original ArticlePodocyturia in pregnant women with chronic hypertension may predict kidney injury?
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):172-177
DOI 10.1590/SO100-720320150005238
Views195See morePURPOSE:
To evaluate the presence of podocyturia in chronic hypertensive pregnant women in the third trimester of pregnancy and its possible association with renal disease.
METHODS:
This was an observational study of a convenience sample of 38 chronic hypertensive pregnant women. The podocytes were labeled by the indirect immunofluorescence technique with anti-podocin and diamidino-phenylindole (DAPI). The count was made on 30 random fields analyzed and corrected according to urinary creatinine (podocytes/mg creatinine). The patients were assigned to two groups: NG (normal glomerular function), up to 100 podocytes, and GP (probable glomerulopathy), more than 100 podocytes. Urinary creatinine was measured by the alkaline picrate method. The variables analyzed were body mass index, gestational age, and systolic and diastolic blood pressure at the time of sample collection. Data were analyzed using the SPSS - version 16.0 (IBM - USA). Statistical analysis was performed by the χ2 test, and significant differences were considered when p<0.05.
RESULTS:
The median podocyte count was 20.3 (0.0-98.1) for group GN, and 176.9 (109.1-490.6) for GP. The mean body mass index was 30.2 kg/m2 (SD=5.6), mean gestational age was 35.1 weeks (SD=2.5), median systolic blood pressure was 130.0 mmHg (100.0-160.0) and median diastolic blood pressure was 80.0 mmHg (60.0-110.0). There was no significant correlation between podocyturia and body mass index (p=0.305), gestational age (p=0.392), systolic blood pressure (p=0.540) or diastolic blood pressure (p=0.540).
CONCLUSIONS:
In this study, there was no podocyturia pattern consistent with the presence of active renal disease, although some of the women studied (15.8%) exhibited a significant loss. We believe that it is premature to recommend the inclusion of the determination of podocyturia in routine prenatal clinical practice in chronically hypertensive pregnant women.


