Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo23
To assess the rate of missed postpartum appointments at a referral center for high-risk pregnancy and compare puerperal women who did and did not attend these appointments to identify related factors.
This was a retrospective cross-sectional study with all women scheduled for postpartum consultations at a high-risk obstetrics service in 2018. The variables selected to compare women were personal, obstetric, and perinatal. The variables of interest were obtained from the hospital's electronic medical records. Statistical analyses were performed using the Chi-square, Fisher's exact, or Mann–Whitney tests. For the variable of the interbirth interval, a receiver operating characteristic curve (ROC) was used to best discriminate whether or not patients attended the postpartum consultation. The significance level for the statistical tests was 5%.
A total of 1,629 women scheduled for postpartum consultations in 2018 were included. The rate of missing the postpartum consultation was 34.8%. A shorter interbirth interval (p = 0.039), previous use of psychoactive substances (p = 0.027), current or former smoking (p = 0.003), and multiparity (p < 0.001) were associated with non-attendance.
This study showed a high rate of postpartum appointment non-attendance. This is particularly relevant because it was demonstrated in a high-risk obstetric service linked to clinical severity or social vulnerability cases. This highlights the need for new approaches to puerperal women before hospital discharge and new tools to increase adherence to postpartum consultations, especially for multiparous women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):186-191
Psychiatric symptoms are common mental issues in pregnancy and the postpartum period. There is limited information regarding the psychiatric symptoms of women with high-risk pregnancy in the postpartum period. This study aimed to compare the severity of psychiatric symptoms and psychological distress in women with high-risk and low-risk pregnancies in the postpartum period.
This case-control study examined 250 women in the postpartum period in two groups with low-risk (n = 112) and high-risk (n = 138) pregnancies. Women completed the Brief Symptom Inventory-53 (BSI-53) and the Risk Postnatal Psychosocial Depression Risk Questionnaire (PPDRQ).
The mean severity of psychiatric symptoms in women with high-risk pregnancies was significantly higher than that in women with low-risk pregnancies (39.34 ± 17.51 vs. 30.26 ± 17.08). Additionally, the frequency of psychological distress in women with high-risk pregnancies was approximately twice higher than that in women with low-risk pregnancies (30.3% vs. 15.2%). Furthermore, the risk factors for depression in women with high-risk pregnancies were almost 1.5 times (59.8% vs. 39.8%) higher than the factors in women with low-risk pregnancies. The results of the logistic analysis indicated that high-risk pregnancies could be twice the odds ratio of developing postpartum psychological distress (ß = 2.14, 95% CI 1.4-6.3, p= 0.036).
Psychiatric symptoms and the psychological distress index are higher in postpartum women with high-risk pregnancies than in postpartum women with low-risk pregnancies. The study suggests that obstetricians and pregnant women's health care providers should strongly consider screening of psychiatric symptoms in women with high-risk pregnancies both during pregnancy and after delivery as the women's routine care priorities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):11-20
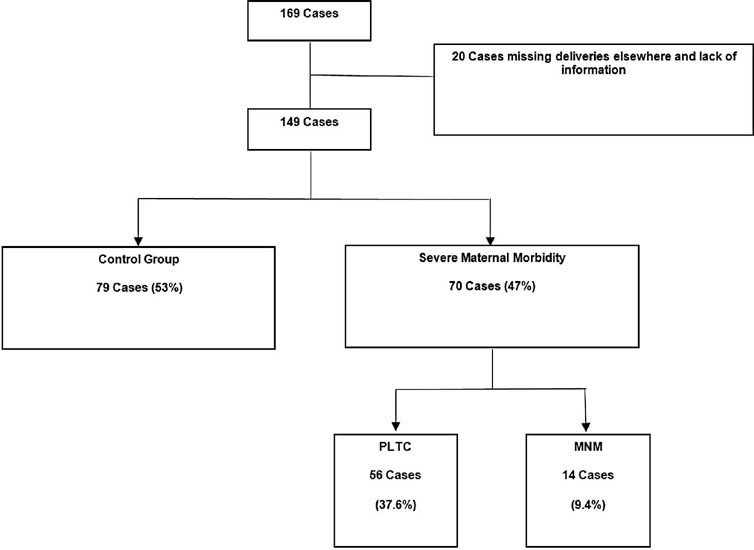
Systemic lupus erythematosus (SLE) may cause irreversible organ damage. Pregnancy with SLE may have severe life-threatening risks. The present study aimed to determine the prevalence of severe maternal morbidity (SMM) in patients with SLE and analyze the parameters that contributed to cases of greater severity.
This is a cross-sectional retrospective study from analysis of data retrieved from medical records of pregnant women with SLE treated at a University Hospital in Brazil. The pregnant women were divided in a control group without complications, a group with potentially life-threatening conditions (PLTC), and a group with maternal near miss (MNM).
The maternal near miss rate was 112.9 per 1,000 live births. The majority of PLTC (83.9%) and MNM (92.9%) cases had preterm deliveries with statistically significant increased risk compared with the control group (p = 0.0042; odds ratio [OR]: 12.05; 95% confidence interval [CI]: 1.5–96.6 for the MNM group and p = 0.0001; OR: 4.84; 95%CI: 2.2–10.8 for the PLTC group). Severe maternal morbidity increases the risk of longer hospitalization (p < 0.0001; OR: 18.8; 95%CI: 7.0–50.6 and p < 0.0001; OR: 158.17; 95%CI: 17.6–1424,2 for the PLTC and MNM groups, respectively), newborns with low birthweight (p = 0.0006; OR: 3.67; 95%CI: 1.7–7.9 and p = 0.0009; OR: 17.68; 95%CI: 2–153.6) for the PLTC and MNM groups, respectively] as well as renal diseases (PLTC [8.9%; 33/56; p = 0.0069] and MNM [78.6%; 11/14; p = 0.0026]). Maternal near miss cases presented increased risk for neonatal death (p = 0.0128; OR: 38.4; 95%CI: 3.3–440.3]), and stillbirth and miscarriage (p = 0.0011; OR: 7.68; 95%CI: 2.2–26.3]).
Systemic lupus erythematosus was significantly associated with severe maternal morbidity, longer hospitalizations, and increased risk of poor obstetric and neonatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1094-1101
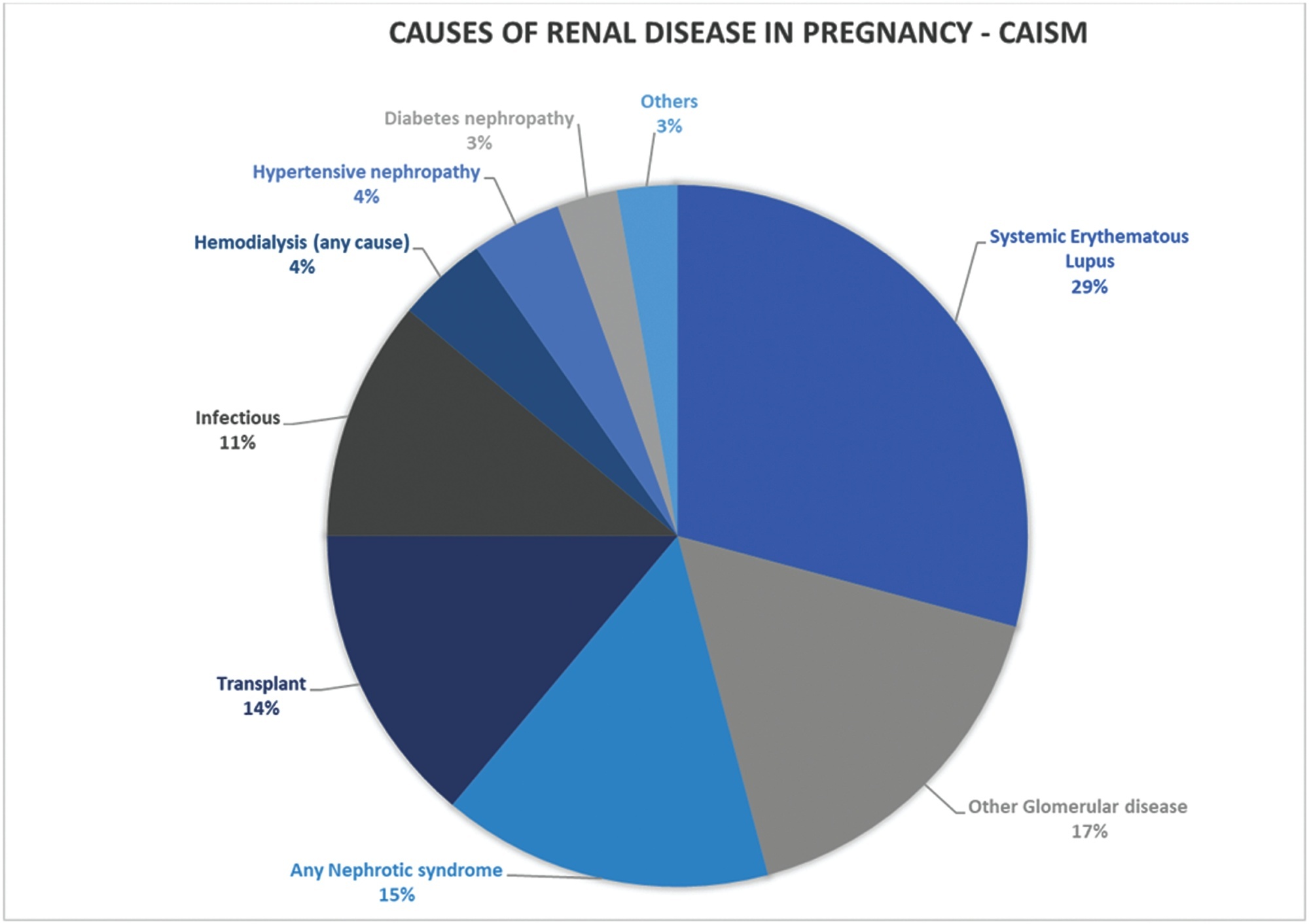
To assess maternal and neonatal outcomes in women with chronic kidney disease (CKD) at a referral center for high-risk pregnancy.
A retrospective cohort of pregnant women with CKD was followed at the Women's Hospital of Universidade Estadual de Campinas, Brazil, between 2012 and 2020. Variables related to disease etiology, treatment duration, sociodemographic variables, lifestyle, other associated diseases, obstetric history, and perinatal outcomes were assessed. The causes of CKD were grouped into 10 subgroups. Subsequently, we divided the sample according to gestational age at childbirth, as preterm and term births, comparing maternal and neonatal outcomes, and baseline characteristics as well as outcomes among such groups.
A total of 84 pregnancies were included, in 67 women with CKD. Among them, six pregnancies evolved to fetal death, five to miscarriage, and one was a twin pregnancy. We further analyzed 72 single pregnancies with live births; the mean gestational age at birth was 35 weeks and 3 days, with a mean birth weight of 2,444 g. Around half of the sample (51.39%) presented previous hypertension, and 27.7% developed preeclampsia. Among the preterm births, we observed a higher frequency of hypertensive syndromes, longer maternal intensive care unit (ICU) stay in the postpartum period, higher incidence of admission to the neonatal ICU, higher neonatal death, lower 5-minute Apgar score, and lower birth weight.
This study demonstrates increased adverse outcomes among pregnancies complicated by CKD and expands the knowledge on obstetric care among such women in an attempt to reduce maternal risks and identify factors related to prematurity in this population.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(5):384-394
Coronavirus disease 2019 (COVID-19) is a disease caused by a newly discovered coronavirus, severe acute respiratory syndrome coronavirus 2 (SARSCoV-2), which usually leads to non-specific respiratory symptoms. Although pregnant women are considered at risk for respiratory infections by other viruses, such as SARS and Middle East respiratory syndrome (MERS), little is known about their vulnerability to SARS-CoV-2. Therefore, this study aims to identify and present the main studies on the topic, including the postpartum period.
In this narrative review, articles were searched in various databases, organizations, and health entities using keywords compatible with medical subject headings (MeSH), such as: COVID-19, pregnancy, vertical transmission, coronavirus 2019, and SARS-CoV-2.
The review of the scientific literature on the subject revealed that pregnant women with COVID-19 did not present clinical manifestations significantly different from those of non-pregnant women; however, there are contraindicated therapies. Regarding fetuses, studies were identified that reported that infection by SARS-CoV-2 in pregnant women can cause fetal distress, breathing difficulties and premature birth, but there is no substantial evidence of vertical transmission.
Due to the lack of adequate information and the limitations of the analyzed studies, it is necessary to provide detailed clinical data on pregnant women infected with SARS-CoV-2 and on the maternal-fetal repercussions caused by this infection. Thus, this review may contribute to expand the knowledge of professionals working in the area as well as to guide more advanced studies on the risk related to pregnant women and their newborns. Meanwhile, monitoring of confirmed or suspected pregnant women with COVID-19 is essential, including in the postpartum period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):323-328
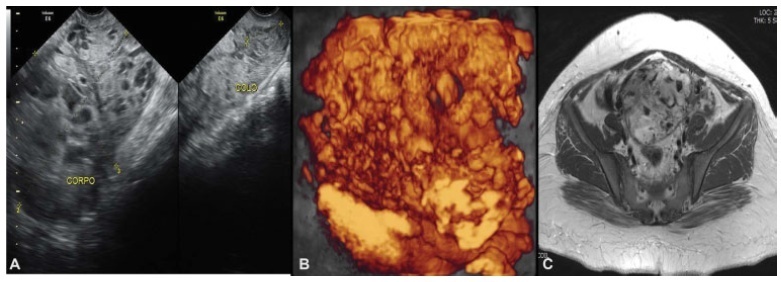
Complete hydatidiform mole (CHM) is a rare type of pregnancy, in which 15 to 20% of the cases may develop into gestational trophoblastic neoplasia (GTN). The diagnostic of GTN must be done as early as possible through weekly surveillance of serum hCG after uterine evacuation.We report the case of 23-year-old primigravida, with CHM but without surveillance of hCG after uterine evacuation. Two months later, the patient presented to the emergency with vaginal bleeding and was referred to the Centro de Doenças Trofoblásticas do Hospital São Paulo. She was diagnosed with high risk GTN stage/score III:7 as per The International Federation of Gynecology and Obstetrics/World Health Organization (FIGO/WHO). The sonographic examination revealed enlarged uterus with a heterogeneous mass constituted of multiple large vessels invading and causing disarrangement of the myometrium. The patient evolved with progressive worsening of vaginal bleeding after chemotherapy with etoposide, methotrexate, actinomycin D, cyclophosphamide and vincristine (EMA-CO) regimen. She underwent blood transfusion and embolization of uterine arteries due to severe vaginal hemorrhage episodes, with complete control of bleeding. The hCG reached a negative value after the third cycle, and there was a complete regression of the anomalous vascularization of the uterus as well as full recovery of the uterine anatomy. The treatment in a reference center was essential for the appropriate management, especially regarding the uterine arteries embolization trough percutaneous femoral
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):84-90
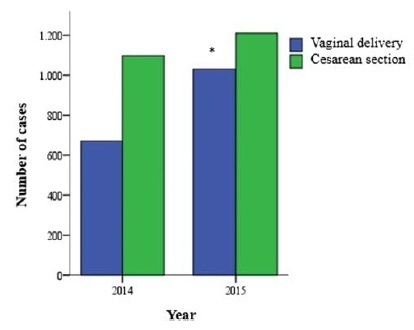
To analyze and compare the frequency of cesarean sections and vaginal deliveries through the Robson Classification in pregnant women attended at a tertiary hospital in two different periods.
Cross-sectional, retrospective study of birth records, comprising 4,010 women, conducted from January 2014 to December 2015 in the only public regional referral hospital for the care of high- risk pregnancies, located in Southern Brazil.
The overall cesarean section rate reached 57.5% and the main indication was the existence of a previous uterine cesarean scar. Based on the Robson Classification, groups 5 (26.3%) and 10 (17.4%) were the most frequent ones. In 2015, there was a significant increase in the frequency of groups 1 and 3 (p < 0.001), when compared with the previous year, resulting in an increase in the number of vaginal deliveries (p < 0.0001) and a reduction in cesarean section rates.
The Robson Classification proved to be a useful tool to identify the profile of parturients and the groups with the highest risk of cesarean sections in different periods in the same service. Thus, it allowsmonitoring in a dynamic way the indications and delivery routes and developing actions to reduce cesarean rates according to the characteristics of the pregnant women attended.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):74-80
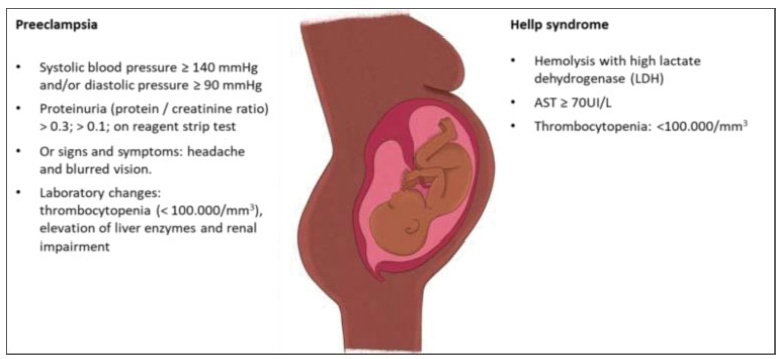
To evaluate the impact of the presence of criteria for severe maternal morbidity and maternal near miss associated with hypertensive disorders on maternal and perinatal outcomes in a maternity school.
The present is a sub-analysis of a larger study involving 27 centers in Brazil that estimated the prevalence of serious maternal morbidity and near miss. It is an analytical and cross-sectional study with a quantitative approach, involving 928 women who were cared for at Maternidade Escola Assis Chateaubriand (MEAC, in Portuguese), Universidade Federal do Ceará (UFC, in Portuguese), from July 2009 to June 2010. The women were diagnosed with near miss according to the World Health Organization (WHO) criteria. The sample was divided into 2 groups: patients with (n = 827) and without hypertension (n = 101). The results were considered statistically significant when p < 0.05. The Pearson chi-squared and Fisher Exact tests were used for the categorical variables, and the Mann–Whitney U test was used for the continuous variables.
In total, 51 participants with maternal near miss criteria were identified, and 36 of them had hypertensive disorders. Of these, 5 died and were obviously excluded from the near miss final group. In contrast, we observed 867 cases with non-near miss maternal morbidity criteria. During this period, there were 4,617 live births (LBs) in the institution that was studied.
In the severe morbidity/maternal near miss population, the presence of hypertensive complications was prevalent, constituting a risk factor for both the mother and the fetus.