-
Original Article12-21-2020
The Influence of Preeclampsia, Advanced Maternal Age and Maternal Obesity in Neonatal Outcomes Among Women with Gestational Diabetes
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(10):607-613
Abstract
Original ArticleThe Influence of Preeclampsia, Advanced Maternal Age and Maternal Obesity in Neonatal Outcomes Among Women with Gestational Diabetes
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(10):607-613
Views342See moreAbstract
Objective
The present study aims to analyze adverse fetal or neonatal outcomes in women with gestational diabetes, including fetal death, preterm deliveries, birthweight, neonatal morbidity and mortality, as well as the synergic effect of concomitant pregnancy risk factors and poor obstetric outcomes, as advanced maternal age, maternal obesity and pre-eclampsia in their worsening.
Methods
The present cohort retrospective study included all pregnant women with gestational diabetes, with surveillance and childbirth at the Hospital da Senhora da Oliveira during the years of 2017 and 2018. The data were collected from the medical electronic records registered in health informatic programs Sclinico and Obscare, and statistical simple and multivariate analysis was done using IBM SPSS Statistics.
Results
The study participants included 301 pregnant women that contributed to 7.36% of the total institution childbirths of the same years, in a total of 300 live births. It was analyzed the influence of pre-eclampsia coexistence in neonatal morbidity (p = 0.004), in the occurrence of newborns of low and very low birthweight (p < 0.01) and in preterm deliveries (p < 0.01). The influence of maternal obesity (p = 0.270; p = 0.992; p = 0.684) and of advanced maternal age in these 3 outcomes was also analyzed (p = 0,806; p = 0.879; p = 0.985).Using a multivariate analysis, the only models with statistic significance to predict the three neonatal outcomes included only pre-eclampsia (p = 0.04; p < 0.01; p < 0.01).
Conclusion
Only coexistence of pre-eclampsia showed an association with adverse neonatal outcomes (neonatal morbidity, newborns of low and very low birthweight and preterm deliveries) and can be used as a predictor of them in women with gestational diabetes.
-
Original Article03-27-2020
Gestational Diabetes in the Population Served by Brazilian Public Health Care. Prevalence and Risk Factors
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):12-18
Abstract
Original ArticleGestational Diabetes in the Population Served by Brazilian Public Health Care. Prevalence and Risk Factors
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):12-18
Views370See moreAbstract
Objective
To assess the prevalence of gestational diabetes mellitus and the main associated risk factors in the population served by the Brazilian Unified Health System in the city of Caxias do Sul, state of Rio Grande do Sul.
Materials and Methods
A descriptive, cross-sectional and retrospective study was conducted. Maternal variables were collected from the medical records of all pregnant women treated at the basic health units in 2016. Hyperglycemia during pregnancy (pregestational diabetes, overt diabetes and gestational diabetes mellitus) was identified by analyzing the results of a 75-g oral glucose tolerance test, as recommended by the Brazilian Ministry of Health. Based on the data, the women were allocated into two groups: the gestational diabetes group and the no gestational diabetes group.
Results
The estimated prevalence of gestational diabetes among 2,313 pregnant women was of 5.4% (95% confidence interval [95%CI]: 4.56-6.45). Pregnant women with 3 or more pregnancies had twice the odds of having gestational diabetes compared with primiparous women (odds ratio [OR]=2.19; 95%CI: 1.42-3.37; p<0.001). Pregnant women aged 35 years or older had three times the odds of having gestational diabetes when compared with younger women (OR=3.01; 95%CI: 1.97-4.61; p<0.001). Overweight pregnant women were 84% more likely to develop gestational diabetes than those with a body mass index lower than 25 kg/m2 (OR =1.84; 95%CI: 1.25-2.71; p=0.002). A multivariable regression analysis showed that being overweight and being 35 years old or older were independent variables.
Conclusion
In this population, the prevalence of gestational diabetes mellitus was of 5.4%. Age and being overweight were predictive factors for gestational diabetes.
-
Original Article02-03-2019
Factors Associated with the Need for Insulin as a Complementary Treatment to Metformin in Gestational Diabetes Mellitus
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):697-702
Abstract
Original ArticleFactors Associated with the Need for Insulin as a Complementary Treatment to Metformin in Gestational Diabetes Mellitus
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):697-702
Views289See moreAbstract
Objective
To evaluate the factors associated with the need for insulin as a complementary treatment to metformin in pregnant women with gestational diabetes mellitus (GDM).
Methods
A case-control study was performed from April 2011 to February 2016 with pregnant women with GDM who needed complementary treatments besides diet and physical exercise. Those treated with metformin were compared with those who, in addition to metformin, also needed the combination with insulin. Maternal characteristics and glycemic control were evaluated. Multinomial logistic regression models were developed to evaluate the influence of different therapies on neonatal outcomes.
Results
A total of 475 pregnant women who needed pharmacological therapy were evaluated. Of these, 366 (77.05%) were submitted to single therapy with metformin, and 109 (22.94%) needed insulin as a complementary treatment. In the analysis of the odds ratio (OR), fasting glucose (FG)<90 mg/dL reduced the odds of needing the combination (OR: 0.438 [0.235-0.815]; p=0.009], as well as primiparity (OR: 0.280 [0.111-0.704]; p=0.007]. In obese pregnant women, an increased chance of needing the combination was observed (OR: 2,072 [1,063-4,039]; p=0,032).
Conclusion
Obesity resulted in an increased chance of the mother needing insulin as a complementary treatment to metformin, while FG<90 mg/dL and primiparity were protective factors.
-
Original Article12-20-2019
Comparison of Maternal and Fetal Outcomes in Parturients With and Without a Diagnosis of Gestational Diabetes
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(11):647-653
Abstract
Original ArticleComparison of Maternal and Fetal Outcomes in Parturients With and Without a Diagnosis of Gestational Diabetes
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(11):647-653
Views203See moreAbstract
Objective
The present study aims to compare the maternal and fetal outcomes of parturients with and without a gestational diabetes diagnosis.
Methods
A case-control study including parturients with (cases) and without (control) a gestational diabetes diagnosis, who delivered at a teaching hospital in Southern Brazil, between May and August 2018. Primary and secondary data were used. Bivariate analysis and a backward conditionalmultivariate logistic regression were used to make comparisons between cases and controls, which were expressed by odds ratio (OR), with a 95% confidence interval (95%CI) and a statistical significance level of 5%.
Results
The cases (n=47) weremore likely to be 35 years old or older compared with the controls (n=93) (p<0.001). The cases had 2.56 times greater chance of being overweight (p=0.014), and a 2.57 times greater chance of having a positive family history of diabetes mellitus (p=0.01). There was no significant difference regarding weight gain, presence of a previous history of gestational diabetes, height, or delivery route. The mean weight at birth was significantly higher in the infants of mothers diagnosed with diabetes (p=0.01). There was a 4.7 times greater chance of macrosomia (p<0.001) and a 5.4 times greater chance of neonatal hypoglycemia (p=0.01) in the infants of mothers with gestational diabetes.
Conclusion
Therefore, maternal age, family history of type 2 diabetes, obesity and pregestational overweightness are important associated factors for a higher chance of developing gestational diabetes.
-
Review Article02-01-2019
Effectiveness of Insulin Analogs Compared with Human Insulins in Pregnant Women with Diabetes Mellitus: Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(2):104-115
Abstract
Review ArticleEffectiveness of Insulin Analogs Compared with Human Insulins in Pregnant Women with Diabetes Mellitus: Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(2):104-115
Views180See moreAbstract
Diabetes during pregnancy has been linked to unfavorable maternal-fetal outcomes. Human insulins are the first drug of choice because of the proven safety in their use. However, there are still questions about the use of insulin analogs during pregnancy. The objective of the present study was to determine the effectiveness of insulin analogs compared withhuman insulin in the treatment of pregnant women with diabetes througha systematic review withmeta-analysis. The search comprised the period since the inception of each database until July 2017, and the following databases were used:MEDLINE, CINAHL, EMBASE, ISIWeb of Science, LILACS, Scopus, SIGLE andGoogle Scholar.We have selected 29 original articles: 11 were randomized clinical trials and 18 were observational studies.We have explored data from 6,382 participants. All of the articles were classified as having an intermediate to high risk of bias. The variable that showed favorable results for the use of insulin analogs was gestational age, with a mean difference of - 0.26 (95 % confidence interval [CI]: 0.03-0.49; p = 0.02), but with significant heterogeneity (Higgins test [I2] = 38%; chi-squared test [χ2] = 16.24; degree of freedom [DF] = 10; p = 0.09). This result, in the clinical practice, does not compromise the fetal well-being, since all babies were born at term. There was publication bias in the gestational age and neonatal weight variables. To date, the evidence analyzed has a moderate-to-high risk of bias and does not allow the conclusion that insulin analogs are more effective when compared with human insulin to treat diabetic pregnant women.
-
Original Article02-01-2017
Predictors of cesarean delivery in pregnant women with gestational diabetes mellitus
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):60-65
Abstract
Original ArticlePredictors of cesarean delivery in pregnant women with gestational diabetes mellitus
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):60-65
Views278See moreAbstract
Purpose
The aim of this study was to evaluate which risk factors may lead patients with gestational diabetes mellitus to cesarean delivery.
Methods
This was a retrospective, descriptive study. The subjects of the study were pregnant women with gestational diabetes mellitus attending a public maternity hospital in the south of Brazil. The primary outcomes assessed were based on maternal and fetal characteristics. The data were correlated using an odds ratio (OR) with a 95% confidence interval (95%CI), calculated using multinomial logistic regression.
Results
A total of 392 patients with gestational diabetes mellitus were analyzed, and 57.4% of them had cesarean deliveries. Among the maternal characteristics, the mean age of the patients and the pregestational body mass index were greater when a cesarean delivery was performed (p = 0.029 and p < 0.01 respectively). Gestational age at birth, newborn weight, weight class according to gestational age, and Apgar score were not significant. The analysis of the OR showed that the chance of cesarean delivery was 2.25 times (95%CI = 1.49-2.39) greater if the pregnant woman was obese, 4.6 times (95%CI = 3.017-7.150) greater if she was a primigravida, and 5.2 times (95% CI = 2.702-10.003) greater if she had a previous cesarean delivery. The other parameters analyzed showed no differences.
Conclusion
The factors that led to an increase in the occurrence of cesarean deliveries included history of a prior cesarean section, first pregnancy, and obesity.
-
Original Article01-01-2017
Prevalence of Hypertrophic Cardiomyopathy in Fetuses of Mothers with Gestational Diabetes before Initiating Treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(1):9-13
Abstract
Original ArticlePrevalence of Hypertrophic Cardiomyopathy in Fetuses of Mothers with Gestational Diabetes before Initiating Treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(1):9-13
Views215See moreABSTRACT
Objective:
To evaluate the prevalence of hypertrophic cardiomyopathy (HCM) in fetuses of pregnant women with gestational diabetes mellitus (GDM) in the beginning of the treatment.
Methods:
A cross-sectional study was performed between July 1, 2013, and Decem-ber 20, 2013, in a public maternity clinic in southern Brazil. The subjects were 63 fetuses of mothers with gestational diabetes, with a single pregnancy and no other associated pathologies. We diagnosed HCM through a fetal echocardiography before treatment and evaluated the maternal and fetal characteristics.
Results:
The average age of the pregnant women was 32.32 (±6.2) years, and the average gestational age at the time of the evaluation was 30.59 (±2.27) weeks. The interventricular septum thickness showed a standard deviation of more than two in 50.8% of the fetuses (95% confidence interval [95%CI]: 38.1-63.5%). The left ventricular wall thickness showed a standard deviation of more than 2 in 13 (20.6%) fetuses (95%CI: 11.1-30.2%). The HCM was confirmed in 54% of the fetuses (95%CI: 41.3-65.1%). The fetal abdominal circumference was normal in 46 (73%) fetuses, and 50% of these fetuses had HCM.
Conclusion:
The prevalence of hypertrophic cardiomyopathy in fetuses of pregnant women with GDM before treatment was of 54% (95%CI: 41.3-65.1%).
-
Original Article08-01-2016
Postpartum Reclassification of Glycemic Status in Women with Gestational Diabetes Mellitus and Associated Risk Factors
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):381-390
Abstract
Original ArticlePostpartum Reclassification of Glycemic Status in Women with Gestational Diabetes Mellitus and Associated Risk Factors
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):381-390
Views235See moreAbstract
Objective
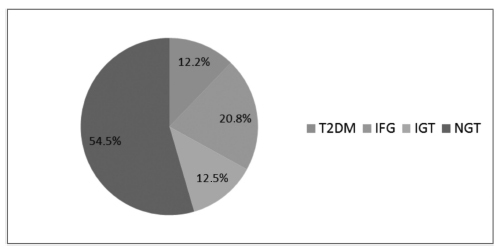
The aims of the study were to evaluate, after pregnancy, the glycemic status of women with history of gestational diabetes mellitus (GDM) and to identify clinical variables associated with the development of type 2 diabetes mellitus (T2DM), impaired fasting glucose (IFG), and impaired glucose tolerance (IGT).
Methods
Retrospective cohort of 279 women with GDM who were reevaluated with an oral glucose tolerance test (OGTT) after pregnancy. Characteristics of the index pregnancy were analyzed as risk factors for the future development of prediabetes (IFG or IGT), and T2DM.
Results:
T2DM was diagnosed in 34 (12.2%) patients, IFG in 58 (20.8%), and IGT in 35 (12.5%). Women with postpartum T2DM showed more frequently a family history of T2DM, higher pre-pregnancy body mass index (BMI), lower gestational age, higher fasting and 2-hour plasma glucose levels on the OGTT at the diagnosis of GDM, higher levels of hemoglobin A1c, and a more frequent insulin requirement during pregnancy. Paternal history of T2DM (odds ratio [OR] =5.67; 95% confidence interval [95%CI] =1.64-19.59; p =0.006), first trimester fasting glucose value (OR =1.07; 95%CI =1.03-1.11; p =0.001), and insulin treatment during pregnancy (OR =15.92; 95%CI =5.54-45.71; p < 0.001) were significant independent risk factors for the development of T2DM.
Conclusion
A high rate of abnormal glucose tolerance was found in women with previous GDM. Family history of T2DM, higher pre-pregnancy BMI, early onset of GDM, higher glucose levels, and insulin requirement during pregnancy were important risk factors for the early identification of women at high risk of developing T2DM. These findings may be useful for developing preventive strategies.