Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(1):10-17
DOI 10.1590/S0100-72032006000100003
PURPOSE: to describe to emotional process experienced with termination of pregnancy after the diagnosis of lethal fetal malformation. METHODS: thirty-five pregnant women who underwent termination of pregnancy for lethal fetal anomaly after judicial permission were interviewed. The most frequent fetal malformation was anencephaly (71.5%). The patients were submitted to an open interview as soon as the diagnosis of fetal malformation was confirmed, allowing them to express their feelings and stimulating them to think about asking for termination of pregnancy. The mean time spent until the judicial agreement was 16.6 days. The women who requested and were submitted to the procedure of abortion were invited to return for psychological evaluation after 30-60 days. At this moment, a semi-structured interview was performed to find the emotional aspects and feelings that existed. RESULTS: thirty-five patients were interviewed. The decision-making feelings about termination of pregnancy were negative for 60%, 51.4% declared that they had no doubts about the assumed decision and 65.7% declared that their own opinion was more important for decision than anyone else's. Most of the women (89%) affirmed to remember the facts about the procedure that they experienced, 91% affirmed that they would have the same attitude in the case of another similar situation in the future and 60% declared that they would advise someone to opt for termination of pregnancy if asked about the same situation. CONCLUSIONS: the anguish experienced showed that the process of thinking is very important for the decision-making process and posterior satisfaction with the assumed posture. The psychological follow-up allows to review the moral and cultural values in order to help the decision-making process with the aim of minimizing the suffering.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(3):155-160
DOI 10.1590/S0100-72032005000300010
PURPOSE: to evaluate the outcome of fetuses with risk of chromosomal anomalies over 1:300, based on the nuchal translucency measurement, according to the Fetal Medicine Program. METHODS: in the pregnancies with risk of chromosomal anomalies over 1:300, variables like fetal karyotype, spontaneous or induced abortion, prematurity, stillbirth, neonatal death, malformations, and healthy newborn were considered. We used Fisher's exact test to compare differences in proportions between groups. RESULTS: we selected 193 (3.6%) single pregnancies with risk of chromosomal anomalies over 1:300. Only 165 cases fulfilled the inclusion criteria. Of these only 32.1% underwent fetal karyotyping and of which 8.5% had chromosomal anomalies (85.7% had trisomy 21). Regarding pregnancy outcomes, 4.2% were spontaneous miscarriages, 4.2% induced abortions, 4.8% were premature, 1.8% had neonatal death, 1.8% were stillborn, and 4.2% had structural malformation (85.7% congenital heart diseases). Almost 85.0% were healthy newborns. Patients with abnormal karyotyping had more induced abortions (p<0.001) and more structural malformations (p<0.001) than patients with normal karyotyping. None of the genetic diseases or miscarriages was associated with invasive procedures. Sixty-six percent of the pregnancies with prenatal diagnosis of abnormal karyotype were interrupted. CONCLUSION: nuchal translucency is an important screening tool for chromosomal diseases especially for low-risk pregnancies. However, counseling pregnancies with high risk of chromosomal anomalies should consider that, although these fetuses have a worse prognosis, most of the outcomes are favorable.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(3):149-154
DOI 10.1590/S0100-72032005000300009
PURPOSE: to analyze the efficacy, safety and real advantage of vesicoamniotic shunt catheter in the intrauterine treatment of obstructive uropathy. METHODS: a retrospective and descriptive study, in which the evolution of 35 fetuses with obstructive uropathy, submitted to vesicoamniotic shunt from 1990 to 2004 in a Fetal Medical Center was evaluated. All these fetuses fitted the selection criteria defined by a protocol of this service, and had the parents' consent for the procedure. The Pediatric Nephrology Sector of the Hospital das Clínicas of UFMG assessed all of them after delivery to confirm the prenatal diagnosis and outcome. The dead neonates were studied by the Pathological Anatomy Sector of UFMG. Descriptive analysis of the following parameters was performed: prenatal diagnosis of the uropathy, gestational age at shunt insertion, time of catheter utilization, post-surgery complications, perinatal mortality and neonatal survival. RESULTS: posterior urethral valve was the most common uropathy (62.8%). The mean gestational age at the vesicoamniotic shunt placement was 26.1weeks and the mean time of its presence was 46 days (1-119 days). There were four intrauterine fetal deaths and 17 in the neonatal period (60% perinatal mortality). The main cause of death was pulmonary hypoplasia. Olygohidramnios was present in 33/35 fetuses (94.3%) and it was reversed in 23 of them (70%); fourteen fetuses survived the neonatal period. At present, there are 4 children followed up by the Pediatric Sector of Nephrology of Hospital das Clínicas. Two of them have been treated with peritoneal dialysis, awaiting renal transplantation. The other two have normal renal function. Their age varies from 2 months to 4 years. CONCLUSION: the vesicoamniotic shunt may be a viable intrauterine treatment for severe obstructive uropathy, with 40% of survival rate of fetuses that might have progressed to death. However, the procedure's success was directly related to the adequate selection, and to the early intervention in the uterus, performed before 32 weeks of gestation in fetuses with bilateral obstruction, without any associated malformation and with still preserved renal function. Olygohidramnios reversion did not guarantee a good prognosis. It remains controversial if the vesicoamniotic shunt can really ensure long-term renal function.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(6):353-356
DOI 10.1590/S0100-72032005000600010
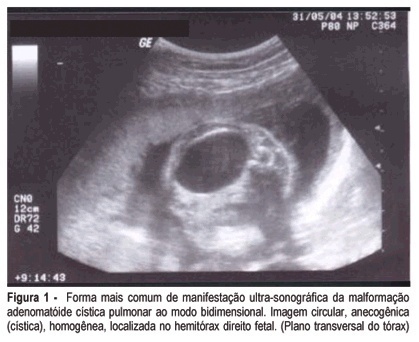
Fetal cystic adenomatoid malformation is a pulmonary developmental anomaly arising from an overgrowth of the terminal respiratory bronchioles. This is such a rare malformation, that is not always thought of as a diagnostic possibility. We present a case of pulmonary cystic adenomatoid malformation and emphasize the importance of early diagnosis and therapeutic possibilities. We also present its evolution after prenatal placement of a catheter for continuous drainage.