Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo48
Evaluate the prevalence of macrosomic newborns (birth weight above 4000 grams) in a high-risk maternity from 2014 to 2019, as well as the maternal characteristics involved, risk factors, mode of delivery and associated outcomes, comparing newborns weighing 4000-4500 grams and those weighing above 4500 grams.
This is an observational study, case-control type, carried out by searching for data in hospital’s own system and clinical records. The criteria for inclusion in the study were all patients monitored at the service who had newborns with birth weight equal than or greater than 4000 grams in the period from January 2014 to December 2019, being subsequently divided into two subgroups (newborns with 4000 to 4500 grams and newborns above 4500 grams). After being collected, the variables were transcribed into a database, arranged in frequency tables. For treatment and statistical analysis of the data, Excel and R software were used. This tool was used to create graphs and tables that helped in the interpretation of the results. The statistical analysis of the variables collected included both simple descriptive analyzes as well as inferential statistics, with univariate, bivariate and multivariate analysis.
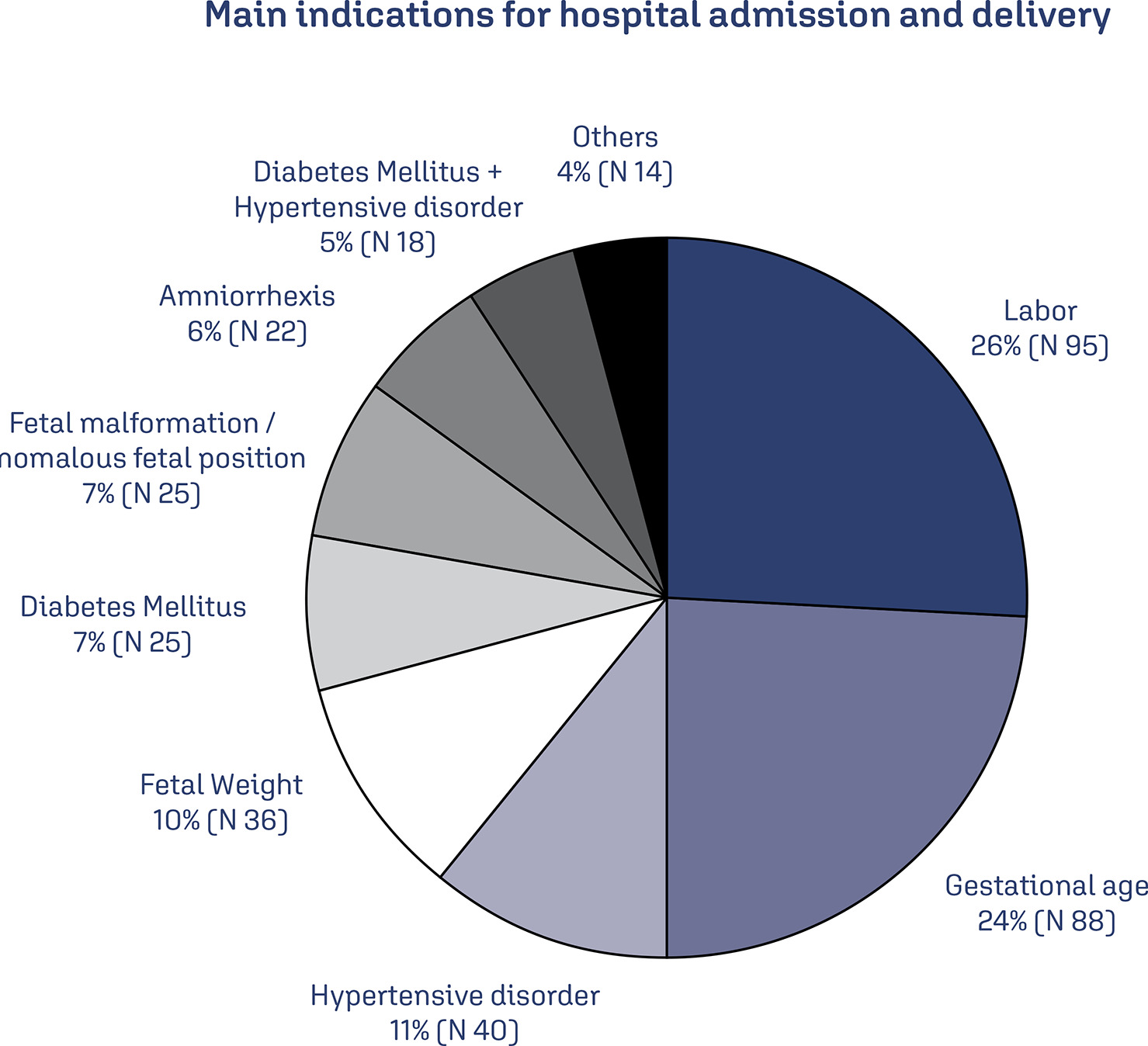
From 2014 to 2019, 3.3% of deliveries were macrosomic newborns. The average gestational age in the birth was 39.4 weeks. The most common mode of delivery (65%) was cesarean section. Diabetes mellitus was present in 30% of the deliveries studied and glycemic control was absent in most patients. Among the vaginal deliveries, only 6% were instrumented and there was shoulder dystocia in 21% of the cases. The majority (62%) of newborns had some complication, with jaundice (35%) being the most common.
Birth weight above 4000 grams had a statistically significant impact on the occurrence of neonatal complications, such as hypoglycemia, respiratory distress and 5th minute APGAR less than 7, especially if birth weight was above 4500 grams. Gestational age was also shown to be statistically significant associated with neonatal complications, the lower, the greater the risk. Thus, macrosomia is strongly linked to complications, especially neonatal complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):682-687
The present study aims to understand to what extent obesity is related to adversematernal, obstetrical, and neonatal outcomes in a Portuguese obstetrical population.
A retrospective case-control study was conducted at the Department of Obstetrics of a differentiated perinatal care facility. The study compared 1,183 obese pregnant womenwith 5,399 normal or underweight pregnantwomen for the occurrence of gestational diabetes, hypertensive pregnancy disorders, and preterm birth. Mode of delivery, birthweight, and neonatal intensive care unit (ICU) admissionswere also evaluated. Mean blood glucose values were evaluated and compared between groups, in the first and second trimesters of pregnancy. Only singleton pregnancies were considered.
The prevalence of obesity was 13.6%. Obese pregnant women were significantly more likely to have cesarean sections (adjusted odds ratio [aOR] 2.0, p< 0.001), gestational diabetes (aOR 2.14, p< 0.001), hypertensive pregnancy disorders (aOR 3.43, p< 0.001), and large-for-gestational age ormacrosomic infants (aOR 2.13, p< 0.001), and less likely to have small-for-gestational age newborns (aOR 0.51, p< 0.009). No significant differences were found in terms of pretermbirths, fetal/neonatal deaths, low birthweight newborns, and neonatal ICU admissions among cases and controls. Maternal obesity was significantly associated with higher mean blood glucose levels, in the first and second trimesters of pregnancy.
Obesity is associated with increased risks of adverse pregnancy and neonatal outcomes. These risks seem to increase progressively with increasing body mass index (BMI) class. Female obesity should be considered a major public health issue and has consequences on maternal-fetal health.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):348-353
DOI 10.1590/S0100-72032011001100005
PURPOSE: To describe the obstetric outcome of women with overweight/obesity treated at the prenatal care clinic of a public maternity hospital in Rio de Janeiro. METHODS: A descriptive cross-sectional study which investigated 433 women (³20 years-old, without any chronic diseases) and their newborns treated at public hospitals in Rio de Janeiro. Information was collected from medical records and through interviews. The characteristics of mothers and newborns evaluated were divided into maternal (social habits, anthropometric measurements and clinical, obstetric, and prenatal care) and newborn groups (birth conditions). Data regarding the categories of nutritional status were analyzed using the odds ratio (OR) and 95% confidence interval (CI). RESULTS: The prevalence of overweight/obesity in this sample was 24.5% (n=106). There was an association between inadequate weight gain and the prevalence of overweight/obesity (OR 2.7, 95%CI 1.5-4.9, p<0.05). Overweight/obese women had an increased risk for preeclampsia (OR 3.3, 95%CI 1.1--9.9, p=0.03). Regarding birth conditions, mean birth weight was 3291.3 g (±455.2), with rates of low birth weight of 4.7% (n=5) and rates of macrosomia of 2.8% (n=3). CONCLUSIONS: There was an alarming prevalence of inadequate nutritional status before and during pregnancy, which may be associated with increased risk of perinatal morbidity and mortality. This suggests the need for nutritional monitoring of these pregnant women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):241-248
DOI 10.1590/S0100-72032009000500007
OBJECTIVE: to determine the frequency of macrosomia in babies born alive at a reference obstetric service, and its association with maternal risk factors. METHODS: a transversal descriptive study, including 551 women at puerperium, hospitalized at Instituto de Saúde Elpídio de Almeida, in Campina Grande (PB), Brazil, from August to October, 2007. Women, whose deliveries had been assisted at the institution, with babies born alive from one single gestation and approached in the first postpartum day, were included in the study. The nutritional and sociodemographic maternal characteristics were analyzed, and the ratio of macrosomia (birth weight >4.000 g) and its association with maternal variables were determined. Macrosomia was classified as symmetric or asymmetric according to Rohrer's index. Statistical analysis has been done through Epi-Info 3.5 software; the prevalence ratio (PR) and the confidence interval at 95% (CI 95%) were calculated. The research protocol was approved by the local Ethics Committee and all the participants signed the informed consent. RESULTS: the mean maternal age was 24.7 years old, and the mean gestational age was 38.6 weeks. Excessive gestational weight gain was observed in 21.3% of the pregnant women, and 2.1% of the participants had a diagnosis of diabetes mellitus (gestational or clinic). A ratio of 5.4% of macrosomic newborns was found, 60 were asymmetric. There was no significant association between macrosomia, mother's age and parity. There was an association between macrosomia and overweight/obesity in the pre-gestational period (PR=2.9; CI 95%=1.0-7.8) and at the last medical appointment (PR=4.9; CI 95%=1.9-12.5), excessive weight gain (PR = 6.9; CI 95%:2.8-16.9), clinical or gestational diabetes (PR = 8.9; CI 95%:4.1-19.4) and hypertension (PR=2.9; CI 95%=1.1-7.9). The factors that persisted significantly associated with macrosomia in the multivariate analysis were the excessive weight gain during the gestation (RR=6.9; CI 95%=2.9-16.9) and the presence of diabetes mellitus (RR=8.9, CI 95%=4.1-19.4). CONCLUSIONS: considering that excessive gestational weight gain and diabetes mellitus were the factors more strongly associated with macrosomia, it is important that precocious detection measurements and adequate follow-up of such conditions be taken, aiming at preventing unfavorable perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(1):5-9
DOI 10.1590/S0100-72032009000100002
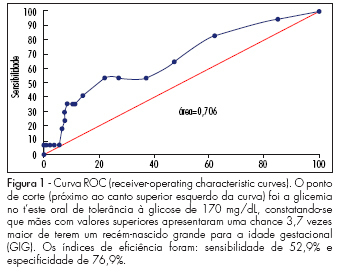
PURPOSE: to evaluate factors related to the presence of neonatal macrosomia in pregnant women with gestational diabetes mellitus. METHODS: 157 pregnant women presenting gestational diabetes mellitus in follow-up were retrospectively selected from January 2004 to July 2006. This group has been divided into two subgroups: one with newborns with weight in accordance with the gestational age (n=136) and another with macrosomic newborns (n=21). Maternal characteristics have been compared between the groups. The t-Student test was used for the analysis of equality hypothesis between the averages of the two groups, and chi-square test, to check the groups' homogeneity concerning ratios. RESULTS: the groups did not show any significant difference concerning the gestational age, body mass index, weight gain along the gestation, number of previous pregnancies, fast glycemia in the oral glucose tolerance test after the ingestion of 75 g (TOTG 75 g), gestational age at delivery, glycemic values during the treatment, and the type of treatment used (p>0.05). In the group with neonatal macrosomia, there was a higher two-hour-glycemia in the TOTG 75 g (p=0.02), higher gestational age at the treatment onset (p=0.02), and a lower number of appointments at the health service (p<0.01). When adjusted to a logistic regression model, the most important factor (p<0.01) found to predict neonatal macrosomia was the two-hour-glycemia in the TOTG 75 g. CONCLUSIONS: the factors more frequently related to neonatal macrosomia were late treatment onset and, consequently, lower number of appointments and chiefly, high two-hour-glycemia in the TOTG 75 g.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(10):486-493
DOI 10.1590/S0100-72032008001000002
PURPOSE: to investigate factors accountable for macrosomia incidence in a study with mothers and progeny attended at a Basic Unity of Health in Rio de Janeiro, Brazil. METHODS: a prospective study, with 195 pairs of mothers and progeny, in which the dependent variable was macrosomia (weight at delivery >4,000 g - independent of the gestational age or of other demographic variables), and socioeconomic, previous pregnancies/gestation course, biochemical, behavioral and anthropometric, the independent variables. Statistical analysis has been done by multiple logistic regression. Relative risk (RR) values have been estimated, based on the simple form: RR=OR/ (1 - I0) + (I0 versus OR), in which I0 is the macrosomia incidence in non-exposed people. RESULTS: Macrosomia incidence was 6.7%, the highest value being found in the progeny of women >30 years old (12.8%), white (10.4%), with two or more children (16.7%), with male newborns (9.6%), with height >1,6 m (12.5%), with overweight or obesity as a nutritional pre-gestational state (13.6%), and with excessive gestational gain of weight (12.7%). The final model has shown that having two or more children (RR=3.7; CI95%=1.1-9.9), and having a male newborn (RR=7.5; CI95%=1.0-37.6) were the variables linked to the macrosomia occurrence. CONCLUSIONS: macrosomia incidence was higher than the one observed in Brazil as a whole, but inferior to the one reported in studies from developed countries. Having two or more children and a newborn male were the factors accountable for the occurrence of macrosomia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(9):513-522
DOI 10.1590/S0100-72032006000900003
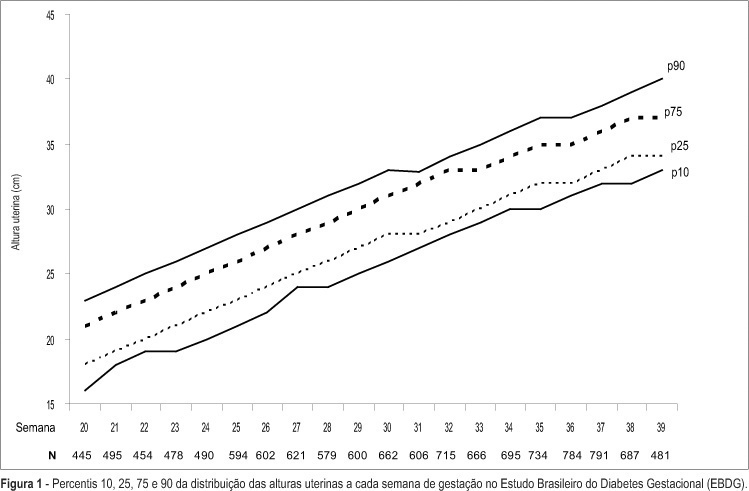
PURPOSE: to describe, in participants of the Brazilian Study of Gestational Diabetes (EBDG), the percentile distribution of uterine height by gestational age and to validate the use of percentiles of the chart derived by the "Centro Latino-Americano de Perinatologia" (CLAP), used as reference in predicting abnormal fetal growth. METHODS: the EBDG is a cohort study of 5564 pregnant women older than 19 years, followed through and after delivery. Interviews and standardized anthropometry were performed at baseline between 20-28 weeks. Medical records covering prenatal and delivery periods were then reviewed following a standardized approach. Analyses pertain to 3539 women with gestational age confirmed by ultrasound. Diagnostic properties of the 10th and the 90th percentiles of both charts (EBDG and CLAP) as predictors of abnormal neonatal weight were determined. RESULTS: uterine height was higher in EBDG than in the CLAP chart at every gestational week, being 1-4 and 2-6 cm greater, at the 10th and 90th percentiles respectively. The CLAP 10th percentile classified as small the uterine heights of only 0.3 to 1.7% of Brazilian women, while the 90th percentile classified as large the uterine heights of 42 to 57% of the sample. The sensitivity of CLAP percentile 10 in the prediction of small for gestational age varied from 0.8 to 6% and the specificity of CLAP percentile 90 in the prediction of large for gestational age, from 46 to 61%. CONCLUSIONS: the CLAP uterine height reference chart does not reflect the current uterine growth pattern of pregnant Brazilians, limiting its clinical applicability in the detection of abnormal fetal growth, especially intrauterine growth restriction.