Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(4):232-237
DOI 10.1590/S0100-72032006000400005
PURPOSE: to identify maternal and perinatal factors related to neonates with birthweight >4,000 g. METHODS: cross-section cohort study with 411 consecutive cases of fetal macrosomia (FM) which occurred from March 1998 to March 2005. Data were compared to 7,349 cases of fetal birthweight >2,500 and <3,999 g which occurred in the same period. Maternal variables (maternal age, parity, diabetes, previous cesarean section, meconium-stained amniotic fluid, cephalopelvic disproportion, main cesarean section indications) and perinatal variables (birth injury, <7 1-min and 5-min Apgar score, fetal and early neonatal mortality range, need of neonatal intensive care unit) were analyzed. For statistical analysis the chi2 test with Yates correction and Student's t test were used with the level of significance set at 5%. RESULTS: FM was significantly associated with older mothers, more parous and <7 1-min Apgar score (p<0.05; OR=1.8; 95% CI: 1,4-2.5) and <7 5-min Apgar score (p<0,05; OR=2.3; 95% CI: 1.3-4,1), diabetes mellitus (p<0.05; OR=4.2; 95% CI: 2.7-6.4), meconium-stained amniotic fluid (p<0.02; OR=1.3; 95% CI: 1.0-1.7), need of neonatal intensive care unit (p<0,05; OR=2.0; 95% CI: 1.5-2.7), early neonatal mortality (p<0,05; OR = 2.7; 95% CI: 1.0-6.7), cesarean section (p < 0.05; OR = 2.03; 95% CI: 1,6-2,5) and cephalopelvic disproportion (p < 0.05;OR = 2.8; 95% CI: 1.6-4,8). There was no statistical difference between birth injury and fetal mortality range. In the FM group the main cesarean section indications were repeat cesarean sections (11.9%) and cephalopelvic disproportion (8.6%); in the normal birthweight group, repeat cesareans (8.3%) and fetal distress during labor (3.9%). CONCLUSIONS: in spite of the characteristic limitations of a retrospective evaluation, the analysis demonstrated which complications were associated with large fetal size, being useful in obstetric handling of patients with a diagnosis of extreme fetal growth. FM remains an obstetric problem of difficult solution, associated with important maternal and perinatal health problems, due to the significant observed rates of maternal and perinatal morbidity and mortality in developed and developing countries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(12):712-718
DOI 10.1590/S0100-72032005001200002
PURPOSE: to verify the fetal heart rate (FHR) patterns of large for gestational age (LGA) fetuses in pregnancies at term complicated by pregestational diabetes. METHODS: fetal surveillance was performed weekly in 64 fetuses of mothers with pregestational diabetes. Inclusion criteria were: diagnosis of pregestational diabetes mellitus, single pregnancy, alive fetus, absence of fetal anomalies, and computerized cardiotocography performed at the 37th week of gestation. Exclusion criteria included: postnatal diagnosis of fetal anomalies and delivery not performed at the local hospital. The FHR patterns were studied with computerized cardiotocography and the parameters were analyzed according to a fetal weight as LGA (birth weight above percentile 90). The cardiotocography parameters included: basal FHR, episodes of high variation, episodes of low variation, and short-term variation. RESULTS: forty-two patients fulfilled the proposed criteria. Ten (23.8%) newborns were LGA. Normal criteria were met in all performed examinations. FHR accelerations (above 15 bpm) were present in 7 (70%) LGA cases and in 29 (90.6%) non-LGA (p=0.135). Accelerations were more frequent in the non-LGA group (1.5±1.3 accelerations/10 min) when compared to LGA group (0.8±0.9 accelerations/10min, p=0.04, Mann-Whitney test). The high variation episodes were detected in all cases. The mean FHR variation in these episodes was different in the LGA group (16.2±2.5 bpm) when compared to the non-LGA group (19.7±4.2 bpm, p=0.02, Mann-Whitney test). CONCLUSION: the FHR patterns of non-LGA (higher frequency of accelerations and higher FHR variation in the high variation episodes) reflect parameters commonly analyzed by traditional cardiotocography of a healthy fetus. This fact appears to confirm the patterns of better oxygen supply to the fetuses less compromised by diabetes in pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):580-587
DOI 10.1590/S0100-72032005001000003
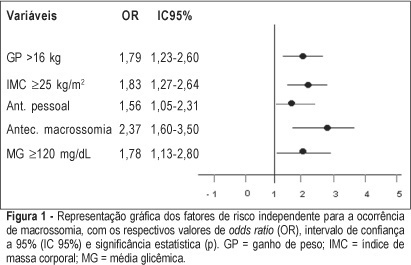
PURPOSE: to identify risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia. METHODS: retrospective study, control-case, including 803 pairs of mothers and newborns belonging to this specific population, divided into two groups - macrosomic (cases, n=242) and non-macrosomic (controls, n=561). Variables regarding age, parity, weight and body mass index (BMI), weight gain (WG), diabetes history, high blood pressure and tabagism, diabetes type and classification, and glycemic control indicators in the third trimester were compared. The means were evaluated by the F test and the categorized variables were submitted to univariate analysis using the chi² test. The significative results were included in the multiple regression model for the identification of macrosomia independent risk considering OR, 95% CI and p value. The statistical significance limit of 5% was established for all analyses. RESULTS: there was a significative association between macrosomia and WG >16 kg, BMI >25 kg/m², personal, obstetric and macrosomic history, classification in the Rudge groups (IB and IIA + IIB), glycemic mean (GM) >120 mg/dL and postprandial glycemic mean >130 mg/dL in the third trimester. In the multiple regression analysis, WG >16 kg (OR=1,79; 95% CI: 1,23-1.60), BMI >25 kg/m² (OR=1.83; 95% CI: 1.27-2.64), personal history of diabetes (OR=1.56; 95% CI: 1.05-2.31) and of macrosomia (OR=2.37; 95% CI: 1.60-3.50) and GM >120 mg/dL in the third trimester (OR=1.78; 95% CI: 1.13-2.80) confirmed to be independent risk factors for macrosomia in these pregnancies. CONCLUSION: WG >16 kg, BMI >25 kg/m², GM >120 mg/dL in the third trimester and personal history of macrosomia and diabetes were identified as risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(8):461-466
DOI 10.1590/S0100-72032005000800005
PURPOSE: to compare the effectiveness of glibenclamide and acarbose with that of insulin for the treatment of gestational diabetes mellitus (GDM), in regard to maternal glucose levels, newborn (NB) weight and neonatal hypoglycemia. METHODS: an open, randomized prospective study was carried out. Fifty-seven patients diagnosed with GDM were included. These patients required dietary control and additional therapy. Pregnant women were randomly alloted to one of three groups with different therapies: a control group making use of insulin therapy, a study group making use of glibenclamide and a study group making use of acarbose. The study took seven months (from October 1st 2003 to May 1st 2004). Assessed outcomes were maternal glucose levels in the prenatal period, the need for replacing therapy to achieve glucose level control, NB weight and neonatal hypoglycemia. Statistical analysis was determined by ANOVA with the level of significance set at 5%. RESULTS: maternal characteristics were similar in all the three groups. Glucose level control was not obtained in three of the patients who used glibenclamide (15%) and in seven (38.8%) of the patients who used acarbose. Regarding fasting and postprandial glucose level rates and average NB weight no difference between the three groups was observed. No statistical difference was found for fasting or postprandial glucose levels and average NB weight in any of the three groups. The rate of large for gestational age fetuses was 5.2, 31.5 and 11.1% for the groups treated with insulin, glibenclamide and acarbose, respectively. Neonatal hypoglycemia was observed in six NB. Four of these were from the glibenclamide group (21.0%). CONCLUSIONS: glibenclamide was more effective for glucose level control than acarbose but neither were more efficient than insulin. NB children whose mothers had been alloted to the glibenclamide group showed a higher rate of macrosomia and neonatal hypoglycemia when compared to those newborns whose mothers were subjected to other therapies.