Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo25
04-09-2024
Fertility preservation is a priority in oncology for female cancer patients. However, there is a lack of communication between infertility specialists and oncologists. This study aimed to evaluate infertility specialists’ perceptions and experiences regarding fertility preservation.
Conduct an online survey to profile infertility specialists. Participants were infertility affiliated with the Brazilian Federation of Gynecology and Obstetrics Associations (FEBRASGO). The specialists received an online survey, which response rate were 30.9%, most of whom were in southern and southeastern. The survey consisted on 14 questions about the infertility specialists’ location, techniques in clinical practice, treatment successful rate, patients idea, etc.
The average experience in human reproduction were 15.5 ± 10.2 years (mean ± standard deviation, range 1-40). Among reproductive-aged female cancer patients recommended for fertility preservation, 60.3 ± 28.8% (range 10-100%) underwent preservation procedures. Main barriers were cost (41%), oncologists’ knowledge or acceptance (35%) and accessibility (9%). Most infertility specialists (58%) considered 40 years the limit for fertility preservation. Leukemia, lymphoma, breast and ovarian cancers were prioritized for fertility preservation, while lung, thyroid, gastric, and brain cancers were less relevant.
This is the first Brazilian study about infertility specialists’ perceptions on oncology patients access to fertility preservation. These patients primarily receive treatment in the public health system, while infertility specialists mainly work in the private healthcare. This healthcare mode is currently fragmented, but integrating these experts is enhancing patient access to fertility preservation. Studies on this topic are still warranted.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo33
04-09-2024
Evaluate histological changes in testicular parameters after hormone treatment in transgender women.
Cross-section study with patients who underwent gonadectomy at Hospital de Clínicas de Porto Alegre from 2011 to 2019. Hormone treatment type, route of administration, age at initiation and duration were recorded. Atrophy parameters were observed: testicular volume, tubular diameter, basal membrane length, presence of spermatogonia and spermatids (diploid and haploid spermatozoid precursors).
Eighty-six patients were included. Duration of hormone treatment is associated with testicular atrophy and spermatogenesis arrest. Other characteristics of hormone treatment such as age of initiation, route of administration and type of treatment were not associated with testicular histological changes. Testicular volume may predict spermatogenesis arrest. Basal membrane length and tubular diameter ratio is an interesting predictor of germ cell presence.
Cross-sex hormone treatment affects testicular germ cell presence. Basal membrane length and tubular diameter ratio reduces inter variability of measurements and better exemplify how atrophic seminiferous tubules are. Fertility preservation should be addressed by healthcare providers in order to recognize gender affirming treatment impact on transgender health.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):249-255
06-19-2019
The present study aimed to examine which development indicators are correlated with cervical cancer (CC) mortality rates in Brazil.
This was an ecological study that correlatedmortality rates and indicators, such as human development index (HDI), gross domestic product (GDP) per capita, illiteracy rate, fertility rate, screening coverage, proportion of private health insurance use, density of physicians, and density of radiotherapy centers. Themortality rateswere obtained fromthe Brazilian national registry, while the indicators were based on official reports from the Ministry of Health. Univariate and multivariate linear regression was used.
Among the states of Brazil, the average age-specific CC mortality rate from 2008 to 2012 varied from 4.6 to 22.9 per 100,000 women/year. In the univariate analysis, HDI, proportion of private health insurance use, density of physicians, and density of radiotherapy centers were inversely correlated with the mortality rates. Fertility rate was positively correlated with the mortality rates. In the multivariate analysis, only fertility rate was significantly associated with the CC mortality rate (coefficient of correlation: 9.38; 95% confidence interval [CI]: 5.16-13.59).
A decrease in the fertility rate, as expected when the level of development of the regions increases, is related to a decrease in the mortality rate of CC. The results of the present study can help to better monitor the quality assessment of CC programs both among and within countries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):217-223
05-01-2017
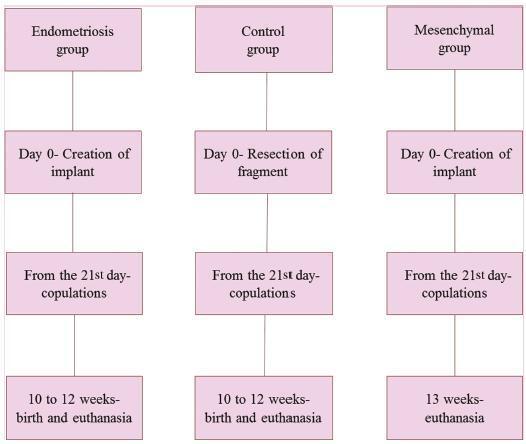
To evaluate the effect of mesenchymal stem cells (MSCs) on fertility in experimental retrocervical endometriosis.
A total of 27 New Zealand rabbits were divided into three groups: endometriosis, in which endometrial implants were created; mesenchymal, in which MSCs were applied in addition to the creation of endometrial implants; and control, the group without endometriosis. Fisher’s exact test was performed to compare the dichotomous qualitative variables among the groups. The quantitative variables were compared by the nonparametric Mann-Whitney and Kruskal-Wallis tests. The MannWhitney test was used for post-hoc multiple comparison with Boniferroni correction.
Regarding the beginning of the fertile period, the three groups had medians of 14±12.7, 40±5, and 33±8.9 days respectively (p = 0.005). With regard to fertility (number of pregnancies), the endometriosis and control groups showed a rate of 77.78%, whereas the mesenchymal group showed a rate of 11.20% (p = 0.015). No differences in Keenan’s histological classification were observed among the groups (p = 0.730). With regard to the macroscopic appearance of the lesions, the mesenchymal group showed the most pelvic adhesions.
The use of MSCs in endometriosis negatively contributed to fertility, suggesting the role of these cells in the development of this disease.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):333-339
07-01-2016
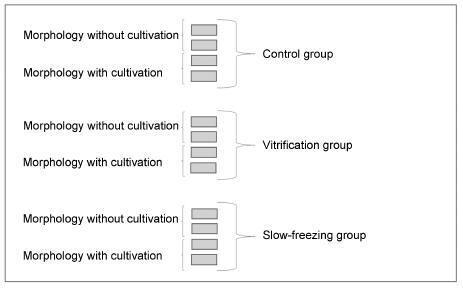
To assess the viability of bovine ovarian tissue after cryopreservation through either slow freezing or vitrification, and to compare it to that of control tissue by performing morphological analyses.
The study included 20 bovine ovarian cortex fragments that were divided into control, vitrification, and slow freezing groups. Each group consisted of four fragments of the same ovary, two fixed without cultivation, and two fixed with cultivation. Tissues were evaluated based on follicular morphology immediately after heating and after 7 days of culture, and compared with the control group.
A total of 240 fragments were analyzed, generating a sample of 1,344 follicles without cultivation and 552 with cultivation. When the non-cultivated samples were classified as non-atretic follicles, 572 were found in the control group, 289 in the vitrification group, and 373 in the slow freezing group, showing no significant differences. When classified as atretic, 46 follicles were found in the control group, 23 in the vitrification group, and 41 in the slow freezing group, also showing no statistical difference. In the post-culture sample, an evolution of the follicular stages could be observed. This finding was important to support that the follicles considered non-atretic in the non-cultivated group were actually viable in the morphological evaluation.
With no differences between the protocols, vitrification was shown to be an advanced and alternative method for patients who will undergo treatments that
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(5):246-251
08-15-2011
DOI 10.1590/S0100-72032011000500007
PURPOSE: to evaluate the prevalence of cytogenetic alterations and chromosomic polymorphism in couples with a subfertility phenotype in a Brazilian population. METHODS: karyotype analysis through G and C banding of 1,236 individuals who presented the subfertility phenotype, from two different centers (public and private) were included in the study. These patients were classified in two sub-groups: one with two or more gestational consecutive losses or not and the o with, at least, one gestacional loss or absence of conception. Karyotype results were evaluated in different groups and frequencies were calculated. Statistical analyses were carried out through Fisher's exact test and Odds Ratio analysis. RESULTS: approximately 25% of the cases presented abnormal karyotype results, including numerical and structural alterations and also polymorphic variants. In both centers, the prevalence of polymorphic variants was 8.9 and 3.8%, respectively. CONCLUSIONS: there was no significant difference between the prevalence of polymorphic variants and other abnormalities in individuals with or without previous history of reproductive loss. The results of the present study reinforce the need of adequate disclosure of complete cytogenetic information in the karyotype results, with specific attention in relation to the polymorphic variants.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(12):621-625
01-18-2009
DOI 10.1590/S0100-72032009001200008
The main source of inhibin B in women is the growing follicle granulosa cells, while inhibin A is mainly produced by the corpus luteum and the placenta. In infertile women submitted to therapies of assisted reproduction, inhibin B has shown to be useful to predict a poor ovulatory response, though it has not yet overcome the performance of other markers. In the pre-natal screening of the Down syndrome, inhibin A has been repeatedly confirmed as useful in the second trimester and has also started to be considered in the first trimester test battery. Besides the two applications above, the dosage of total inhibin may contribute to the identification of cases of autoimmune ovarian insufficiency. Total inhibin may also be an auxiliary marker in the diagnosis of ovarian epithelial tumors, while the amount of inhibin B helps in the diagnosis of granulosa cells tumors. The use of inhibin A may be extended to the evaluation of pregnant women with risk of abortion, with a history of repeated abortion, with increased risk of pre-eclampsia, or even in the first days of follow-up of hydatiform mole post-emptying. All those applications are still under study, but with a real possibility of helping to extend the diagnostic spectrum of inhibin dosage in Gynecology and Obstetrics.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(3):149-159
06-05-2008
DOI 10.1590/S0100-72032008000300008
It is advisable to do the non-invasive diagnosis of ectopic pregnancy precociously, before there is the tube rupture, combining for that the transvaginal ultrasonography with the dosage of the b-fraction of the chorionic gonadotrophin. A range of treatment options may be used. Either a surgical intervention or a clinical treatment may be taken into consideration. Laparotomy is indicated in cases of hemodynamic instability. Laparoscopy is the preferential route for the treatment of tube pregnancy. Salpingectomy should be performed in patients having the desired number of children, while salpingostomy should be indicated in patients willing to have more children, when the b-hCG titers are under 5,000 mUI/mL and the surgical conditions are favorable. The use of methotrexate (MTX) is a consecrated clinical procedure and should be indicated as the first option of treatment. The main criteria for MTX indication are hemodynamic stability, b-hCG <5,000 mUI/mL, anexial mass <3,5 cm, and no alive embryo. It is preferable a single intramuscular dose of 50 mg/m², because it is easier, more practical and with less side effects. Protocol with multiple doses should be restricted for the cases with atypical localization (interstitial, cervical, caesarean section scar and ovarian) with values of b-hCG >5,000 mUI/mL and no alive embryo. Indication for local treatment with an injection of MTX (1 mg/kg) guided by transvaginal ultrasonography should occur in cases of alive embryos, but with an atypical localization. An expectant conduct should be indicated in cases of decrease in the b-hCG titers within 48 hous before the treatment, and when the initial titers are under 1,500 mUI/mL. There are controversies between salpingectomy and salpingostomy, concerning the reproductive future. Till we reach an agreement in the literature, the advice to patients who are looking forward to a future gestation, is to choose either surgical or clinical conservative conducts.