-
Original Article08-01-2017
Trends in the Prevalence of Live Macrosomic Newborns According to Gestational Age Strata, in Brazil, 2001-2010, and 2012-2014
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):376-383
Abstract
Original ArticleTrends in the Prevalence of Live Macrosomic Newborns According to Gestational Age Strata, in Brazil, 2001-2010, and 2012-2014
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):376-383
Views155See moreAbstract
Purpose
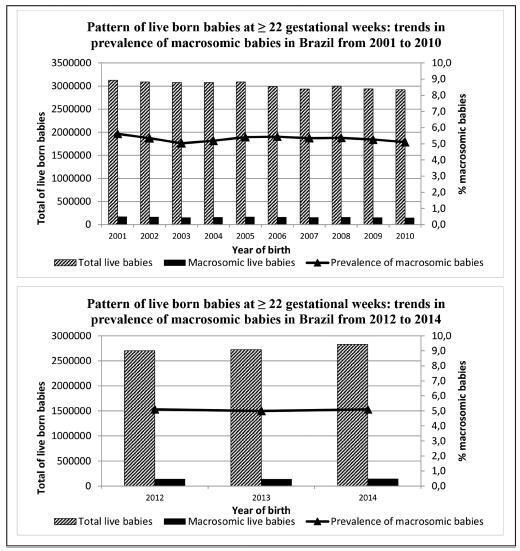
To describe the trends in the prevalence of macrosomia (birth weight ± 4,000 g) according to gestational age in Brazil in the periods of 2001-2010 and 2012-2014.
Methods
Ecological study with data from the Brazilian Live Birth Information System (SINASC, in the Portuguese acronym) regarding singleton live newborns born from 22 gestational weeks. The trends in Brazil as a whole and in each of its five regions were analyzed according to preterm (22-36 gestational weeks) and term (37-42 gestational weeks) strata. Annual Percent Changes (APCs) based on the Prais-Winsten method and their respective 95% confidence intervals (CIs) were used to verify statistically significant changes in 2001-2010.
Results
In Brazil, the prevalence of macrosomic births was of 5.3% (2001-2010) and 5.1% (2012-2014). The rates were systematically higher in the North and Northeast Regions both in the preterm and in term strata. In the preterm stratum, the North Region presented the highest variation in the prevalence of macrosomia (+137.5%) when comparing 2001 (0.8%) to 2010 (1.9%). In the term stratum, downward trends were observed in Brazil as a whole and in every region. The trends for 2012-2014 were more heterogeneous, with the prevalence systematically higher than that observed for 2001-2010. The APC in the preterm stratum (2001-2010) showed a statistically significant trend change in the North (APC: 15.4%; 95%CI: 0.6-32.3) and South (APC: 13.5%; 95%CI: 4.8-22.9) regions. In the term stratum, the change occurred only in the North region (APC:-1.5%; 95%CI: -2.5--0.5).
Conclusion
The prevalence of macrosomic births in Brazil was higher than 5.0%. Macrosomia has potentially negative health implications for both children and adults, and deserves close attention in the public health agenda in Brazil, as well as further support for investigation and intervention.
-
Original Article07-01-2017
Prevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian Amazon
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):350-357
Abstract
Original ArticlePrevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian Amazon
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):350-357
Views278Abstract
Purpose
The aim of this study was to evaluate the overall and type-specific prevalence of human papillomavirus (HPV) infection among females living in riverside communities in the state of Pará, in the Eastern Brazilian Amazon. These communities are inhabited by low-income people, and are accessible only by small boats. Cervical cytology and risk factors for HPV infection were also assessed.
Methods
Cervical samples from 353 women of selected communities were collected both for Papanicolau (Pap) test and HPV detection. Conventional polymerase chain reaction (PCR) and real-time PCR were used to assess the overall and type-specific prevalence of HPV-16 and HPV-18, the main oncogenic types worldwide. Epidemiological questionnaires were used for the assessment of the risk factors for HPV infection.
Results
The mean age of the participants was 37 years (standard deviation [SD] ± 13.7). Most were married or with a fixed sexual partner (79%), and had a low educational level (80%) and family monthly income (< U$ 250; 53%). Overall, HPV prevalence was 16.4% (n = 58), with 8 cases of HPV-16 (2.3%) and 5 of HPV-18 (1.4%). Almost 70% of the women surveyed had never undergone the Pap test. Abnormal cytology results were found in 27.5% (n = 97) of the samples, with higher rates of HPV infection according to the severity of the lesions (p = 0.026).
Conclusions
The infections by HPV-16 and HPV-18 were not predominant in our study, despite the high prevalence of overall HPV infection. Nevertheless, the oncogenic potential of these types and the low coverage of the Pap test among women from riverside communities demonstrate a potential risk for the development of cervical lesions and their progression to cervical cancer, since the access to these communities is difficult and, in most cases, these women do not have access to primary care and public health services.
Key-words cervical cancer screeningEpidemiologyhuman papillomavirus 16human papillomavirus 18Sexually transmitted diseasesSee more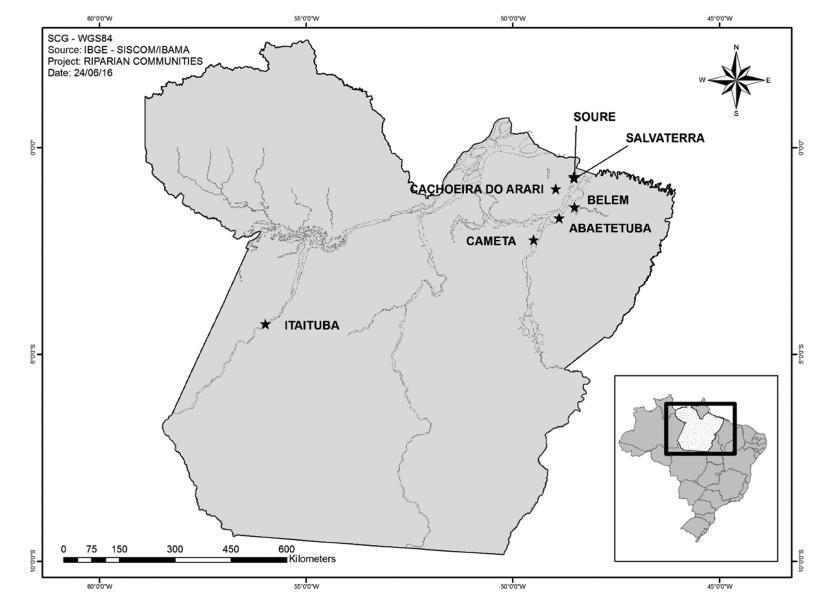
-
Original Article08-01-2016
HIV Prevalence among Pregnant Women in Brazil: A National Survey
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):391-398
Abstract
Original ArticleHIV Prevalence among Pregnant Women in Brazil: A National Survey
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):391-398
Views219See moreAbstract
Background
This study was conducted to determine the seroprevalence of HIV among pregnant women in Brazil and to describe HIV testing coverage and the uptake of antenatal care (ANC).
Methods
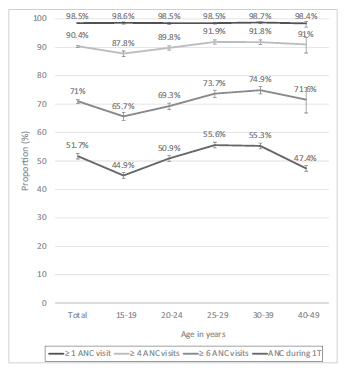
Between October 2010 and January 2012, a probability sample survey of parturient women aged 15-49 years who visited public hospital delivery services in Brazil was conducted. Data were collected from prenatal reports and hospital records. Dried blood spot (DNS) samples were collected and tested for HIV.We describe the agespecific prevalence of HIV infection and ANC uptake with respect to sociodemographic factors.
Results
Of the 36,713 included women, 35,444 (96.6%) were tested for HIV during delivery admission. The overall HIV prevalence was of 0.38% (95% confidence interval [CI]: 0.31-0.48), and it was highest in: the 30 to 39 year-old age group (0.60% [0.40- 0.88]), in the Southern region of Brazil (0.79% [0.59-1.04]), among women who had not completed primary (0.63% [0.30-1.31]) or secondary (0.67% [0.49-0.97]) school education, and among women who self-reported as Asian (0.94% [0.28-3.10]). The HIV testing coverage during prenatal care was of 86.6% for one test and of 38.2% for two tests. Overall, 98.5% of women attended at least 1 ANC visit, 90.4% attended at least 4 visits, 71% attended at least 6 visits, and 51.7% received ANC during the 1st trimester. HIV testing coverage and ANC uptake indicators increased with increasing age and education level of education, and were highest in the Southern region.
Conclusions
Brazil presents an HIV prevalence of less than 1% and almost universal coverage of ANC. However, gaps in HIV testing and ANC during the first trimester challenge the prevention of the vertical transmission of HIV. More efforts are needed to address regional and social disparities.
-
Original Article08-28-2012
Alcohol use pattern in pregnant women cared for in a public university hospital and associated risk factors
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):296-303
Abstract
Original ArticleAlcohol use pattern in pregnant women cared for in a public university hospital and associated risk factors
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):296-303
DOI 10.1590/S0100-72032012000700002
Views105See morePURPOSE: To determine the pattern of alcohol use before and during pregnancy and associated risk factors in puerperal women hospitalized in a public university hospital in Southeastern Brazil. METHODS: Between June and September 2009, 493 puerperae were consecutively evaluated. Those with cognitive impairment were excluded from the study. The AUDIT and CAGE questionnaires were used to diagnose alcohol use/abuse before pregnancy, in addition to the T-ACE during pregnancy. Another questionnaire was applied to collect sociodemographic data, such as age, educational level, marital status, and household income. The χ² test was used in the statistical analysis and the Odds Ratio (OR) and 95% confidence interval (95%CI) were calculated. A p-value <0.05 was considered to be significant. RESULTS: Before pregnancy, the CAGE was positive in 50/405 (12.3%) women and the AUDIT identified alcohol use in 331 (67.1%), which was of low risk in 233 (47.3%), risky in 73 (14.8%), and harmful or indicating possible alcohol dependence in 25 (5%). During pregnancy, the CAGE was positive in 53/405 (13.1%) women and the T-ACE in 84 (17%); the AUDIT identified alcohol use in 114 women, which was of low risk in 73 (14.8%), risky in 27 (5.5%), and harmful or indicating possible alcohol dependence in 14 (2.8%). During pregnancy, alcohol use was more frequent (OR=2.8; 95%CI 1.2 - 6.2) among women with a lower educational level (8.8 versus 3.3%) and more frequent (OR=3.8; 95%CI 1.3 - 11.1) among those who did not cohabit with a partner (6 versus 1.7%). Among pregnant women who drank alcohol, 49/114 (43%) were advised to stop drinking. CONCLUSIONS: Alarming alcohol use was observed during pregnancy, especially among pregnant women with a lower educational level and those who did not cohabit with a partner. There was a low frequency of counseling aimed at abstinence and the AUDIT was the instrument that most frequently diagnosed alcohol consumption.
-
Original Article04-04-2007
Risk factors for the indication of caesarean section in Campinas (SP)
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(1):34-40
Abstract
Original ArticleRisk factors for the indication of caesarean section in Campinas (SP)
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(1):34-40
DOI 10.1590/S0100-72032007000100006
Views99PURPOSE: to determine the cesarean section (CS) rate in Campinas (SP) and to identify its risk factors. METHODS: a cross-sectional study that analyzed data obtained from Live Birth Certificates in 2001. The dependent variable was the type of delivery and the independent variables were: mothers’ characteristics and those related to their pregnancies, deliveries and to newborns. The assessment of the association among variables was performed through the chi2 test, and crude and adjusted odds ratio (OR) values were calculated. RESULTS: the CS rate was 54.9%. The chances of having CS increased 1.9 times for women from 20-34 years old (adjOR-1.9; 95% CI:1.7-2.1); 3.7 times for those over 35 years old (adjOR-3.8; 95% CI:3.2-4.5); 1.5 times for those who studied from 8-11 years (adjOR-1.5; 95% CI:1.4-1.6); 2.5 times for those who studied more than 11 years (adjOR-2.6; 95% CI:2.2-2.9); 1.3 times for those who were married (adjOR-1.3; 95 % CI:1.2-1.4); 1.6 times for those who had jobs (adjOR-1.6; 95% CI:1.5-1.8); 1.2 times for who had good living conditions (adjOR-1.2; 95% CI:1.0-1.3); 2.2 times for primiparous (adjOR-2.2; 95% CI:1.9-2.5), 1.6 times for multiparous (adjOR-1.6; 95% CI:1.4-1.9) and 2.7 times in twin gestations (adjOR-2.7; 95% CI:1.9-3.9). The women who had inadequate prenatal care were protected for CS (adjOR-0.6; 95% CI:0.5-0.7). CONCLUSION: the chance of having CS was greater among women with better socio-economic conditions, with adequate prenatal care, for primiparous, for multiparous and in twin gestations, suggesting that the basis for indication of cesarean sections were not restricted to clinical factors but influenced by non-medical reasons.
Key-words Cesarean sectionEpidemiologyRisk factorsSexual and reproductive healthSocioeconomic factorsSee more -
Original Article08-07-1999
The relationship between borderline and invasive epithelial ovarian tumors: epidemiology, histology and prognosis
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(5):273-277
Abstract
Original ArticleThe relationship between borderline and invasive epithelial ovarian tumors: epidemiology, histology and prognosis
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(5):273-277
DOI 10.1590/S0100-72031999000500005
Views156See morePurpose: to determine some epidemiological, diagnostic and prognostic aspects in women with borderline and invasive epithelial ovarian tumors. Methods: the charts of 198 women treated at CAISM/UNICAMP from 1986 to 1996 were revised. For statistical assessment, chi², Fisher's exact and t Student's tests were used when appropriate, followed by survival curves by the Kaplan-Meyer method, compared by the log-rank test. The mean follow-up was 50 months (11 to 168). Results: the overall rate of borderline tumors was 12% (24 cases), and for invasive carcinoma, 88% (174 cases). The mean age of the patients with borderline tumors was significantly lower than that of those with invasive carcinoma (43 ± 14.8 years vs. 52 ± 12.6 years, p<0.002). The most frequent histologic types were the serous (81 cases: 41%) and the mucinous (46 cases: 23%) tumor. The women with borderline tumors had their diseases diagnosed in earlier stages when compared with the invasive carcinoma patients (p<0.0001). The frozen biopsy, performed on 77 patients, showed a high agreement with the paraffin fixed tissue in the invasive carcinoma cases. However, in borderline tumors, the rate of failure was higher (13%) and the major rate of failure was in mucinous tumors. Regarding prognosis, the survival rate was significantly higher in borderline tumors (p<0.001). Conclusions: women with epithelial ovarian tumors were younger, presented the disease at earlier stages, and had a better prognosis when compared with those with invasive carcinoma.


