-
Original Article00-00-2024
Prevalence and factors associated with anxiety, depression and burnout in gynecology and obstetrics residents during the COVID-19 pandemic
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo17
Abstract
Original ArticlePrevalence and factors associated with anxiety, depression and burnout in gynecology and obstetrics residents during the COVID-19 pandemic
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo17
Views462Abstract
Objective:
To determine the prevalence of anxiety, depression and burnout in residents of Gynecology and Obstetrics during COVID-19 pandemic in Brazil and its associated factors.
Methods:
Cross-sectional study involving all regions of Brazil, through the application of a sociodemographic questionnaire, the Hospital Anxiety and Depression Scale (HAD) and the Maslach Burnout Inventory (MBI-HSS) instrument. Multivariate analysis was performed after adjusting the Poisson model.
Results:
Among the 719 participating medical residents, screening was positive for anxiety in 75.7% and for depression in 49.8% of cases. Burnout syndrome was evidenced in 41.3% of the physicians studied. Those with depression are more likely to have anxiety (OR 0.797; 95%CI 0.687 - 0.925) and burnout syndrome (OR 0.847 95%CI 0.74 - 0.97). Residents with anxiety (OR 0.805; 95%CI 0.699 - 0.928) and burnout (OR 0.841; 95%CI 0.734 - 0.963) are more likely to have depression.
Conclusion:
High prevalence of anxiety, depression and burnout were found in residents of Gynecology and Obstetrics in Brazil, in addition to important correlations between anxiety-depression and depression-burnout.
Key-words AnxietyBrazilBurnout, psychologicalCOVID-19DepressionGynecologyinternship and residencymedical residencyMental healthObstetricspandemicsSee more -
Review Article01-11-2023
Incidence and Outcomes Associated with Menopausal Status in COVID-19 Patients: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):796-807
Abstract
Review ArticleIncidence and Outcomes Associated with Menopausal Status in COVID-19 Patients: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):796-807
Views196See moreAbstract
Objective
Menopause causes several changes in the body that may affect the response to COVID-19. We aimed to investigate the possible association between menopausal status and incidence and outcomes in COVID-19 patients.
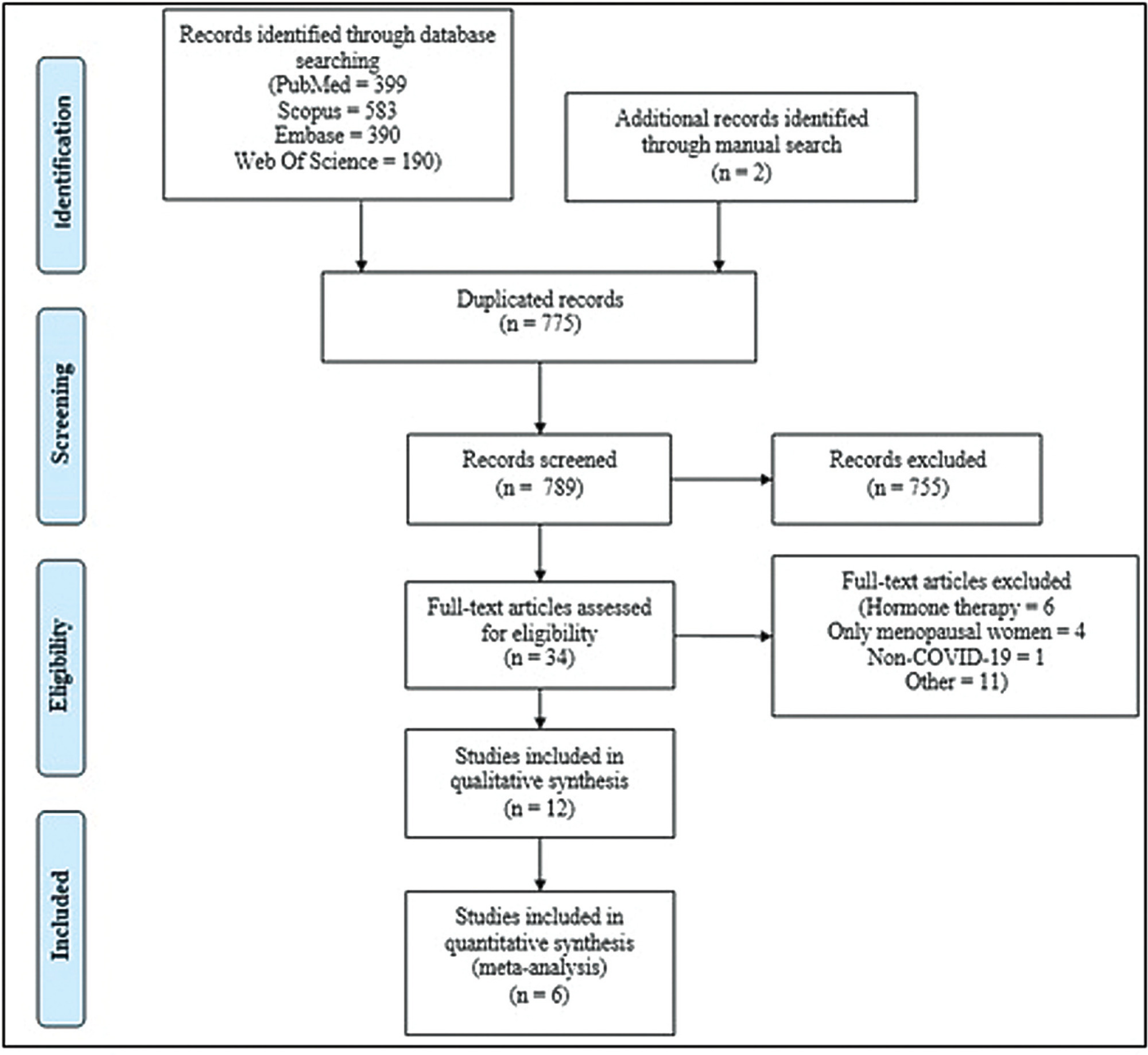
Methods
Combinations of keywordsCOVID-19, menopause, and estrogen were used to search the PubMed, Embase, Web-of-Science, and Scopus databases for articles reporting the incidence and outcomes of COVID-19 (discharge, length-of-admission, intensive care, or mortality) in premenopausal women, available through December 29, 2022. Data from studies comparing the incidence of COVID-19 infection with the age-matched male population were pooled and meta-analyzed using a random-effects model.
Results
Overall, 1,564 studies were retrieved, of which 12 were finally included in the systematic review to compare disease outcomes, and 6 were meta-analyzed for the incidence of COVID-19 in premenopausal and postmenopausal women. All studies reported better COVID-19-associated outcomes in premenopausal women compared with postmenopausal women. After adjusting for confounding factors, three studies found better outcomes in postmenopausal women, and two found no association between menopausal status and COVID-19 outcomes. Our meta-analysis found a higher incidence of COVID-19 infection among premenopausal women than postmenopausal women, when compared with age-matched men (odds ratio = 1.270; 95% confidence interval: 1.086–1.486; p = 0.003).
Conclusion
The incidence of COVID-19 was significantly higher in premenopausal women than in postmenopausal women when compared with age-matched men. Although premenopausal women may have more favorable COVID-19-associated outcomes, the presumed preventive effect of estrogens on the incidence and related outcomes of COVID-19 in premenopausal women cannot be proven at present. Further longitudinal studies comparing pre- and post-menopausal women are required to provide further insight into this matter.
-
Original Article10-09-2023
The Effect of SARS-CoV-2 İnfection on Perinatal Outcomes in Hypertensive Disorders of Pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):439-446
Abstract
Original ArticleThe Effect of SARS-CoV-2 İnfection on Perinatal Outcomes in Hypertensive Disorders of Pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):439-446
Views134See moreAbstract
Objective
To evaluate the fetal and maternal effects of the severe acute respiratory syndrome virus 2 (SARS-CoV-2) infection in women with hypertensive disorders of pregnancy.
Methods
Patients with hypertensive disorders of pregnancy and SARS-CoV-2 polymerase chain reaction (PCR) positivity (n = 55) were compared with cases with similar characteristics and PCR negativity (n = 53). The study group was further divided into two groups as severe (n = 11) and nonsevere (n = 44) coronavirus disease 2019 (COVID-19). The groups were compared in terms of clinical characteristics and perinatal outcomes.
Results
The study and control groups were similar in terms of maternal age, parity, gestational age at diagnosis, type of hypertensive disorders, magnesium sulfate administration rate, gestational age at birth, birth weight, Apgar scores, and maternal complications. However, all cases of fetal loss (n = 6) were observed in the SARS-CoV-2 positive group (p = 0.027). From the 6 cases, there were 5 in the nonsevere group and 1 patient in the severe SARS-CoV-2 positive group. Moreover, higher rates of maternal complications, lower oxygen saturation values, and intensive care unit admissions were observed in the severe COVID-19 group.
Conclusion
Physicians should be cautious about the management of hypertensive disorders of pregnancy cases with SARS-CoV-2 positivity. Fetal loss seems to be more common in cases with SARS-CoV-2 positivity and severe COVID-19 seems to be associated with higher rates of maternal complications. Close follow-up for fetal wellbeing and active management of severe cases in terms of maternal complications seem to be favorable.
-
Original Article09-08-2023
A Study of the Current Scenario of the Obstetrics and Gynecology Residency during the COVID-19 Pandemic
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(7):377-383
Abstract
Original ArticleA Study of the Current Scenario of the Obstetrics and Gynecology Residency during the COVID-19 Pandemic
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(7):377-383
Views178See moreAbstract
Objective
To analyze the impact of the COVID-19 pandemic on the residency of gynecology and obstetrics in São Paulo.
Methods
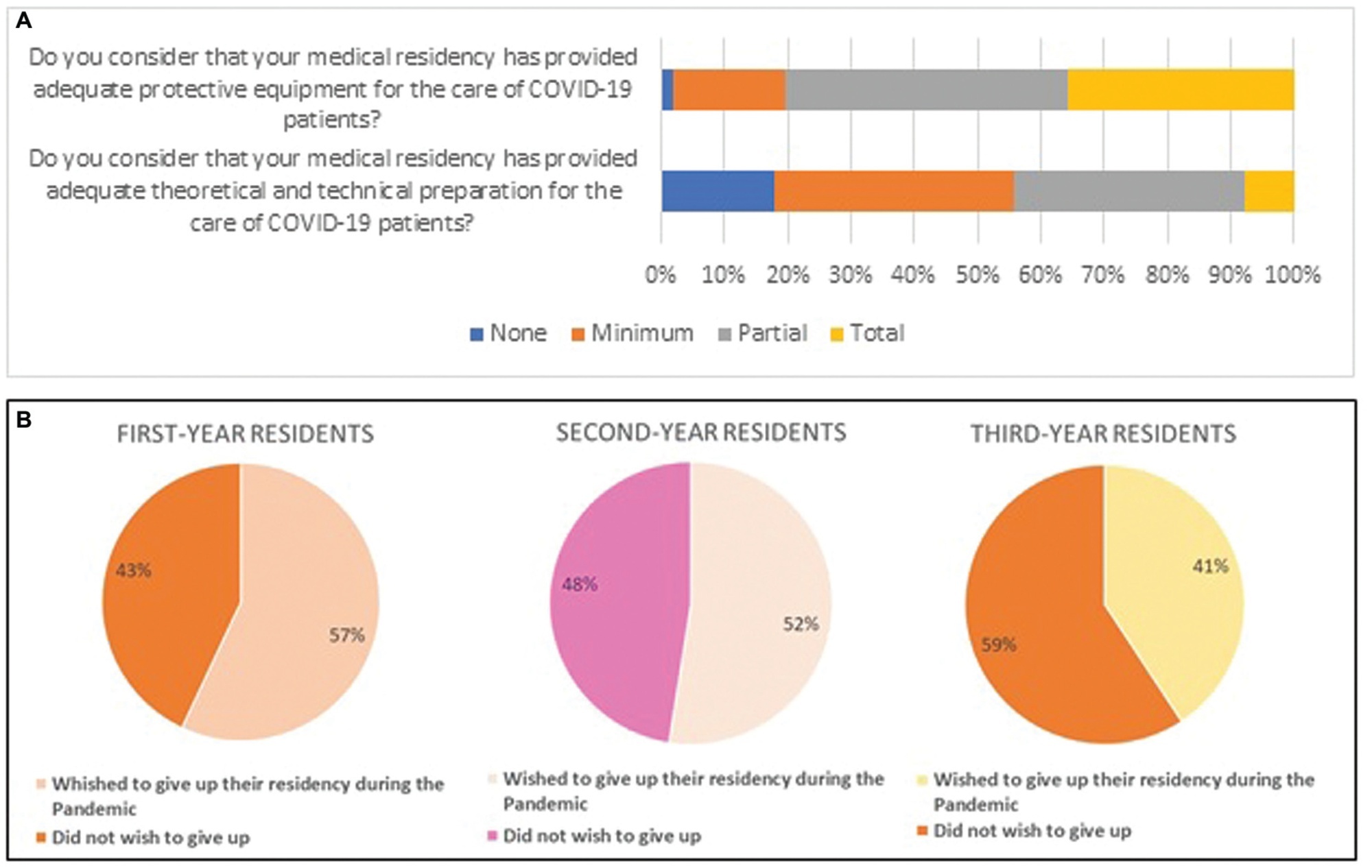
Cross-sectional study developed by representatives of residents of the Association of Gynecology and Obstetrics of the State of São Paulo (SOGESP, in the Portuguese acronym). Data were collected from questionnaires applied to gynecology and obstetrics residents registered on the SOGESP website in February 2022. The interviewees answered about the repercussions of the pandemic on medical residency and whether they had technical and psychological support during the period.
Results
A total of 247 questionnaires were collected from residents of gynecology and obstetrics. The residents had an age of 28.3 ± 3 years old, and most of them were female (88.4%). The displacement to COVID care was reported by 62.34% of the students, but only 35.6% reported completely adequate personal protective equipment and only 7.7% reported complete theoretical and technical instruction to support these patients. Almost all of the interviewees stated that the gynecology sector was the most affected. The majority of the interviewees considered that the second-year residents had the greatest loss, and more than half of the residents in the 1st and 2nd year said they wished to give up their residency during the pandemic. More than 80% of the residents reported online theoretical classes and/or presentation of articles, reinforcing the fact that virtual activities gained a greater space within the medical residency.
Conclusion
The pandemic impacted the residency in greater proportion in outpatient clinics and gynecological surgeries, also interfering with the physician's desire to continue with the program.
-
Original Article09-08-2023
Increased Cesarean Section Rates during the COVID-19 Pandemic: Looking for Reasons through the Robson Ten Group Classification System
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(7):371-376
Abstract
Original ArticleIncreased Cesarean Section Rates during the COVID-19 Pandemic: Looking for Reasons through the Robson Ten Group Classification System
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(7):371-376
Views147See moreAbstract
Objective
To compare cesarean section (CS) rates according to the Robson Ten Group Classification System (RTGCS) and its indications in pregnant women admitted for childbirth during the first wave of the coronavirus disease 2019 (COVID-19) pandemic with those of the previous year.
Materials and Methods
We conducted a cross-sectional study to compare women admitted for childbirth from April to October 2019 (before the pandemic) and from March to September 2020 (during the pandemic). The CSs and their indications were classified on admission according to the RTGCS, and we also collected data on the route of delivery (vaginal or CS). Both periods were compared using the Chi-squared (χ2) test or the Fisher exact test.
Results
In total, 2,493 women were included, 1,291 in the prepandemic and 1,202 in the pandemic period. There was a a significant increase in the CS rate (from 39.66% to 44.01%; p = 0.028), mostly due to maternal request (from 9.58% to 25.38%; p < 0.01). Overall, groups 5 and 2 contributed the most to the CS rates. The rates decreased among group 1 and increased among group 2 during the pandemic, with no changes in group 10.
Conclusion
There was an apparent change in the RTGSC comparing both periods, with a significant increase in CS rates, mainly by maternal request, most likely because of changes during the pandemic and uncertainties and fear concerning COVID-19.
-
Original Article08-07-2023
Existence of SARS-Cov-2 in the Peritoneal Fluid
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):261-265
Abstract
Original ArticleExistence of SARS-Cov-2 in the Peritoneal Fluid
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):261-265
Views208See moreAbstract
Objective
To determine the existence of SARS-CoV-2 in the peritoneal fluid to assess the risk of exposure through surgical smoke and aerosolization threatening healthcare workers during abdominal surgery.
Background
SARS-CoV-2 is a respiratory virus and possible ways of viral transmission are respiratory droplets, close contact, and fecal-oral route. Surgeries pose risk for healthcare workers due to the close contact with patients. Aerosolized particles may be inhaled via the leaked CO2 during laparoscopic procedures and surgical smoke produced by electrocautery.
Methods
All the data of 8 patients, who were tested positive for COVID–19, were collected between August 31, 2020 and April 30, 2021. Recorded clinicopathologic data included age, symptoms, radiological and laboratory findings, antiviral treatment before surgery, type of surgery and existence of the virus in the peritoneal fluid. Nasopharyngeal swab RT-PCR was used for the diagnosis. COVID–19 existence in the peritoneal fluid was determined by RT-PCR test as well.
Results
All 8 COVID–19 positive patients were pregnant, and surgeries were cesarean sections. 1 of the 8 patients was febrile during surgery. Also only 1 patient had pulmonary radiological findings specifically indicating COVID-19 infection. Laboratory findings were as follows: 4 of 8 had lymphopenia and all had elevated D-dimer levels. Peritoneal and amniotic fluid samples of all patients were negative for SARS-CoV-2.
Conclusion
SARS-CoV-2 exposure due to aerosolization or surgical fumes does not seem to be likely, provided the necessary precautions are taken.
-
Original Article08-07-2023
Brazilian Black Women are at Higher Risk for COVID-19 Complications: An Analysis of REBRACO, a National Cohort
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):253-260
Abstract
Original ArticleBrazilian Black Women are at Higher Risk for COVID-19 Complications: An Analysis of REBRACO, a National Cohort
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):253-260
Views150See moreAbstract
Objective
To evaluate the impact of the race (Black versus non-Black) on maternal and perinatal outcomes of pregnant women with COVID-19 in Brazil. Methods This is a subanalysis of REBRACO, a Brazilian multicenter cohort study designed to evaluate the impact of COVID-19 on pregnant women. From February2020 until February 2021, 15 maternity hospitals in Brazil collected data on women with respiratory symptoms. We selected all women with a positive test for COVID-19; then, we divided them into two groups: Black and non-Black women. Finally, we compared, between groups, sociodemographic, maternal, and perinatal outcomes. We obtained the frequency of events in each group and compared them using X2 test; p-values < 0.05 were considered significant. We also estimated the odds ratio (OR) and confidence intervals (CI).
Results
729 symptomatic women were included in the study; of those, 285 were positive for COVID-19, 120 (42.1%) were Black, and 165 (57.9%) were non-Black. Black women had worse education (p = 0.037). The timing of access to the health system was similar between both groups, with 26.3% being included with seven or more days of symptoms. Severe acute respiratory syndrome (OR 2.22 CI 1.17–4.21), intensive care unit admission (OR 2.00 CI 1.07–3.74), and desaturation at admission (OR 3.72 CI 1.41–9.84) were more likely to occur among Black women. Maternal death was higher among Black women (7.8% vs. 2.6%, p = 0.048). Perinatal outcomes were similar between both groups.
Conclusion
Brazilian Black women were more likely to die due to the consequences of COVID-19.
-
Review Article08-04-2023
COVID-19 and Preeclampsia: A Systematic Review of Pathophysiological Interactions
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(6):347-355
Abstract
Review ArticleCOVID-19 and Preeclampsia: A Systematic Review of Pathophysiological Interactions
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(6):347-355
Views249See moreAbstract
Objective:
To review the literature and synthesize evidence on pathophysiological interactions attributed to the simultaneous occurrence of COVID-19 and preeclampsia.
Methods:
A systematic review was conducted from November (2021) to January (2022) to retrieve observational studies published on the PubMed, LILACS, SciELO Brazil and Google Scholar databases. The search was based on the descriptors [(eclampsia OR preeclampsia) AND (COVID-19)]. Quantitative studies that pointed to pathophysiological interactions were included. Literature reviews, studies with HIV participants, or with clinical approach only were excluded. The selection of studies was standardized and the evaluation was performed by pairs of researchers.
Results:
In this review, 155 publications were retrieved; 16 met the inclusion criteria. In summary, the physiological expression of angiotensin-converting enzyme-2 (ACE-2) receptors is physiologically increased in pregnant women, especially at the placental site. Studies suggest that the coronavirus binds to ACE-2 to enter the human cell, causing deregulation of the renin-angiotensin-aldosterone system and in the ratio between angiotensin-II and angiotensin-1-7, inducing manifestations suggestive of preeclampsia. Furthermore, the cytokine storm leads to endothelial dysfunction, vasculopathy and thrombus formation, also present in preeclampsia.
Conclusion:
The studies retrieved in this review suggest that there is a possible overlap of pathophysiological interactions between COVID-19 and preeclampsia, which mainly involve ACE-2 and endothelial dysfunction. Given that preeclampsia courses with progressive clinical and laboratory alterations, a highly quality prenatal care may be able to detect specific clinical and laboratory parameters to differentiate a true preeclampsia superimposed by covid-19, as well as cases with hypertensive manifestations resulting from viral infection.


