Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo9
03-18-2025
To evaluate the continuation rate, satisfaction, and reasons for discontinuation of depot medroxyprogesterone acetate (DMPA) in adolescents treated in a mental health service.
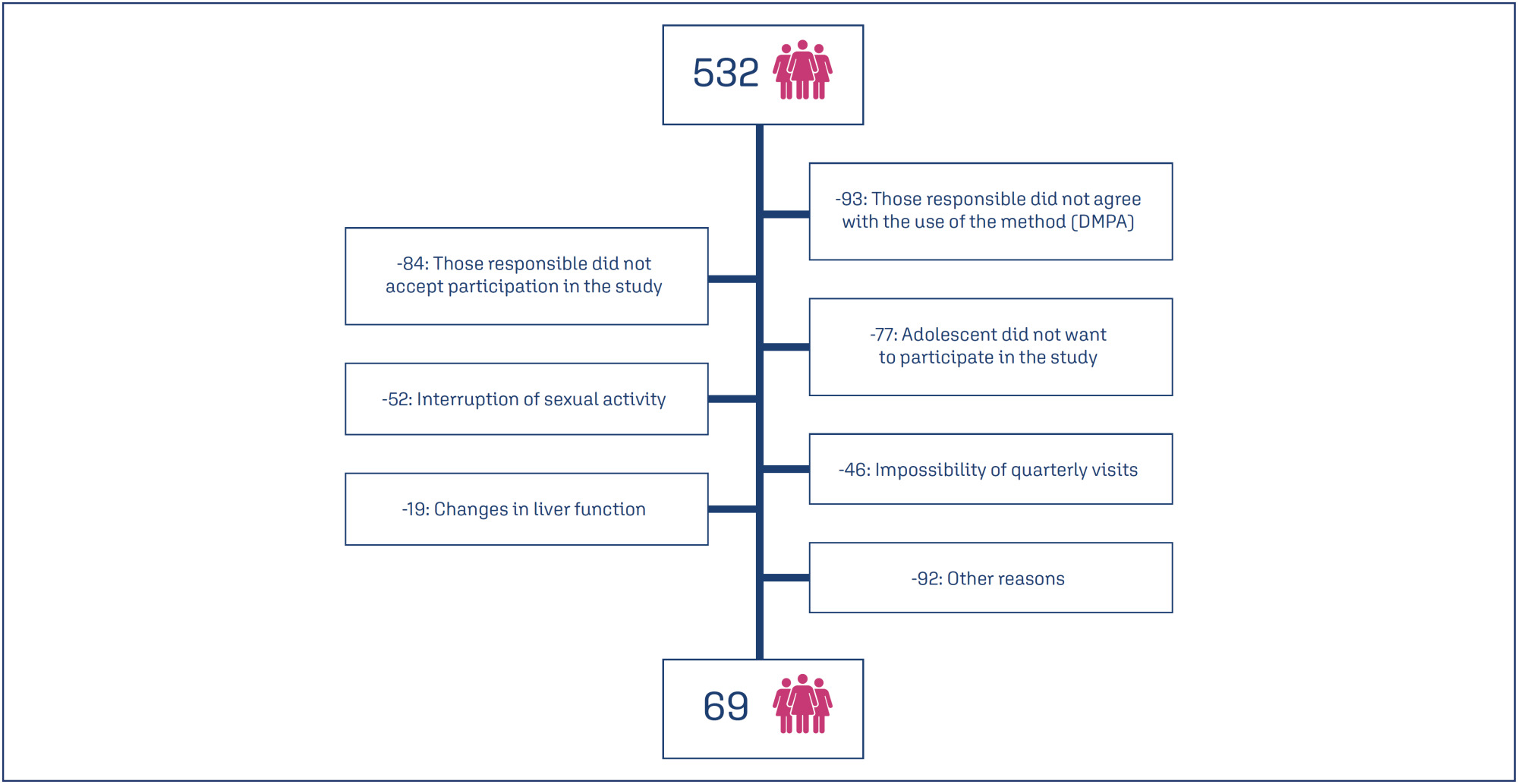
Prospective cohort study conducted in a reference unit for the care of adolescents with mental disorders (MDs) and intellectual disabilities (IDs). All patients received a gynecological consultation and an educational group on contraceptive methods. Sociodemographic data on age, education and gynecological data (menarche, coitarche, regularity of menstrual cycles and presence of symptoms) were collected. Follow-up was quarterly for 12 months, during which symptoms, desire to continue, and satisfaction with the use of the quarterly injectable were assessed.
Eight hundred and sixty-two sexually active adolescents were supported, 532 adolescents chose to use the quarterly injectable, and 69 of these agreed to participate in the study. The mean age of users was 15.5 years (SD=0.91). After 12 months of follow-up, 34 (49.3%) of the 69 adolescents continued to use the method and 36 (52.3%) were satisfied. Among the 33 (47.8%) who discontinued use, the most common reasons were irregular bleeding and weight gain.
Adolescents with intellectual disabilities and/or other mental disorders showed a significant rate of continuation and satisfaction with the use of the depot medroxyprogesterone acetate at 12 months, and the most common reasons for discontinuation were irregular uterine bleeding and weight gain.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):654-660
12-05-2023
To evaluate the continuation rates of the 52-mg levonorgestrel-releasing intrauterine system (LNG-IUS) during the first 5 years of use, reasons for its discontinuation, bleeding patterns, and new contraceptive choice after the 5th year, in adolescents and young women.
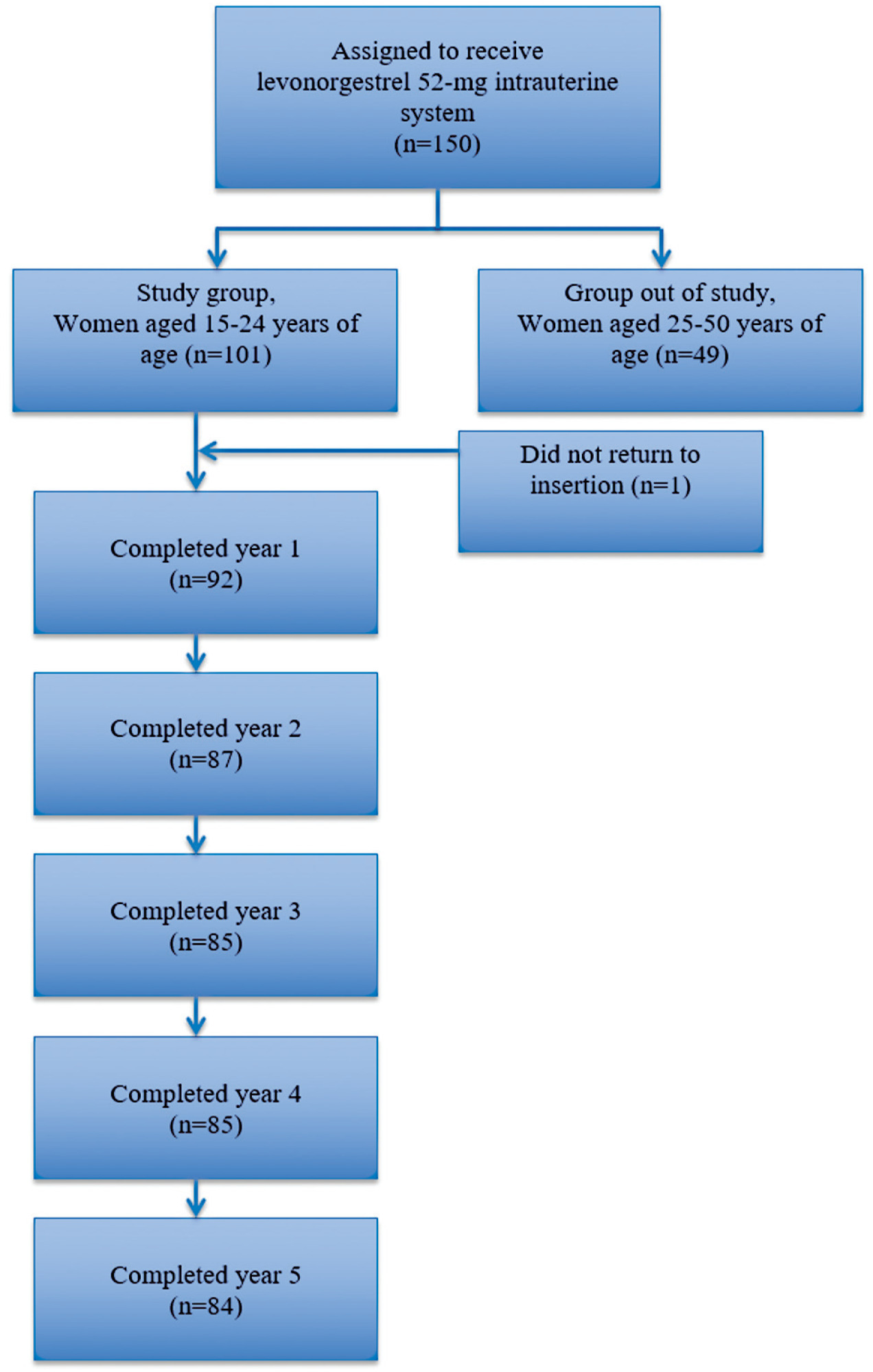
The present study was a 5-year prospective cohort conducted in a Family Planning Service of a tertiary hospital in Brazil. We selected 100 healthy women between 15 and 24 years old who used 52-mg LNG-IUS for contraception. The clinical follow-up of these women took place from June 2017 to December 2022. The study evaluated the continuation rates of the method, reasons for its discontinuation, bleeding patterns, and new contraceptive choice after the 5th year. Continuous data were reported as mean ± standard deviation (SD) and range (minimum-maximum). Categorical variables were described as percentages.
The continuation rates of LNG-IUS were 89.1% (82/92), 82.9% (72/87), 75.3% (64/85), 70.5% (60/85), and 64.2% (54/84) in the 1st, 2nd, 3rd, 4th, and 5th years of use, respectively. The main reason for discontinuation was acne (11/30). Amenorrhea rates were 50, 54.1, 39, 35.7, and 51.8% at 12, 24, 36, 48, and 60 months, respectively. All patients who completed the study and needed contraception after the 5th year opted for long-acting contraceptive methods (LARC).
The LNG-IUS showed high continuation rates in adolescents and young women in the first 5 years of use. Most patients who completed the study chose a LARC method after the 5th year.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):884-890
07-06-2022
Although almost 0.7% of the Brazilian population identifies as transgender, there is currently no training for healthcare professionals to provide comprehensive care to these patients, including the discussion of reproductive planning. The use of testosterone promotes amenorrhea in the first months of use; however, this effect does not guarantee contraceptive efficacy, and, consequently, increases the risks of unplanned pregnancy. The present article is an integrative review with the objective of evaluating and organizing the approach of contraceptive counseling for the transgender population who were assigned female at birth. We used the PubMed and Embase databases for our search, as well as international guidelines on care for the transgender population. Of 88 articles, 7 were used to develop the contraceptive counseling model. The model follows the following steps: 1. Addressing the information related to the need for contraception; 2. Evaluation of contraindications to the use of contraceptive methods (hormonal and nonhormonal); and 3. Side effects and possible discomfort associated with the use of contraception. The contraceptive counseling model is composed of 18 questions that address the indications and contraindications to the use of these methods, and a flowchart to assist patients in choosing a method that suits their needs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(2):194-200
04-08-2022
To analyze the existing scientific literature to find out if the coronavirus disease 2019 (COVID-19) pandemic has an effect on gynecological health.
We performed an integrative review of articles published between April 2020 and April 2021 on the PubMed, SciELO, and LILACS databases, using COVID-19 and the following relevant terms: Menstrual change; Ovarian function; Violence against women; Contraception; HPV; Mental health; and Urogynecology.
Among the eligible studies found, editorials and primary research articles, which describe the dynamics between severe acute respiratory syndrome coronavirus (SARS-CoV-2) infection (the cause of the COVID-19 pandemic) and gynecological health, were included.
Through qualitative synthesis, data were extracted from the included publications and from guidelines of national and international societies of gynecology.
The 34 publications included in the present study showed that some factors of the SARS-CoV-2 infection, and, consequently, the COVID-19 pandemic, might be associated with menstrual abnormalities, effects on contraception, alterations in steroid hormones, changes in urogynecological care, effects on women’s mental health, and negative impact on violence against women.
The COVID-19 pandemic has significantly impacted the health of women. The scientific community encourages the development of recommendations for specialized care for women and strategies to prevent and respond to violence during and after the COVID-19 pandemic.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(2):154-160
04-08-2022
To analyze the profiles of women who accepted and who refused the insertion of the copper intrauterine device (IUD) postpartum and to learn the motivations related to the refusal of the method.
Cross-sectional study with 299 pregnant women. The women were informed about the possibility of inserting a copper IUD postpartum and were questioned about their interest in adopting or not this contraceptive. All participants answered a questionnaire with information relevant to the proposals of the present study. The sample size was limited to the number of devices available for the present study.
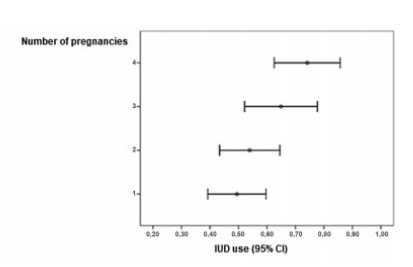
A total of 560 women were invited to join the present study and 299 accepted. Out of the 299 women included in the present study, 175 accepted the copper IUD and 124 refused. As the number of pregnancies increased, the IUD acceptance rate raised (p=0.002), especially between the groups with 1 and with ≥ 4 pregnancies (p=0.013). Regarding the desire to havemore children, the women who planned to have more children were more likely to refuse the method than the ones who did not (p<0,001).
Women with multiple pregnancies and desire to not have more children were more likely to accept the copper IUD. The profile of those who refused was first pregnancy and desire to have more children. Among the three most frequent reasons reported for copper IUD rejection, two responses stood out: no specific justification and desire to have more children.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):940-948
01-24-2021
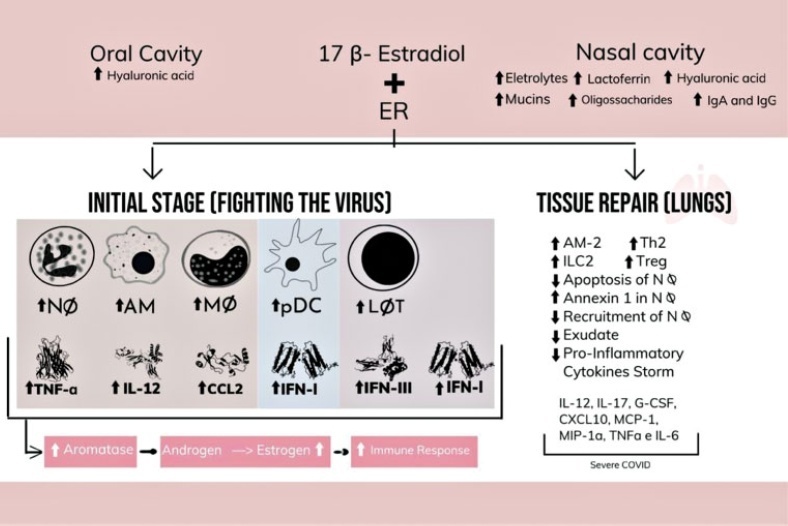
Women have metabolic, immunological, and genetic variables that ensure more protection from coronavirus infection. However, the indication of treatment for several pathologies and contraception is determined by hormones that have adverse effects and raise doubts about their use during the COVID-19 pandemic. Therefore, the present study searches women specificities and the relation between female sexual hormones and COVID-19, and reports the main recommendations in this background. To this end, a review of the literature was conducted in the main databases, auxiliary data sources, and official websites. Therefore, considering the hypercoagulability status of COVID-19, the debate about the use of contraceptives due to the relative risk of thromboembolic effects that they impose arises. However, the current available evidence, as well as the recommendations of main health organs around the world, demonstrate that the use of hormonal contraceptives must be maintained during the pandemic.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):172-177
05-24-2021
To evaluate the acceptability of postplacental placement of intrauterine devices (PPIUD), reasons for refusal and suggested policies to increase its use.
Cross-sectional study conducted at the Women Hospital of the Universidade de Campinas, Campinas, SP, Brazil. Postplacental placement of intrauterine devices was offered to women admitted in labor who did not present infections, uterinemalformation, twin pregnancy, preterm birth, and were at least 18 years old. In case of refusal, the parturient was asked to give their reasons and the answers were classified as misinformation about contraception or other reasons. The following were considered misinformation: fear of pain, bleeding, contraception failure and future infertility. Bivariate analysis was performed.
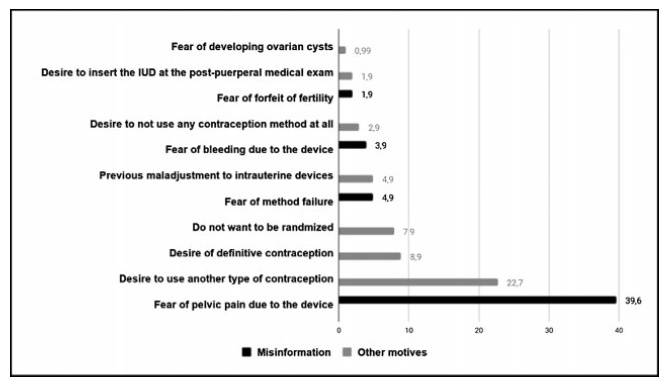
Amongst 241 invited women, the refusal rate was of 41.9%. Misinformation corresponded to 50.5% of all refusals, and the reasons were: fear of pain (39.9%); fear of contraception failure (4.9%); fear of bleeding (3.9%); fear of future infertility (1.9%); other reasons for refusal were 49.5%. Parturients aged between 18 and 27 years old refused the PPIUD more frequently due to misinformation (67.4%), and older parturients (between 28 and 43 years old) refused frequently due to other reasons (63.6%) (p=0.002). Themean age of those who declined the PPIUD due to misinformation was 27.3 ± 6.4 years old, while those who declined for other reasons had a mean age of 29.9 ± 5.9 years old (p=0.017).
The refusal of the PPIUD was high, especially amongst young women and due to misinformation. It is necessary to develop educative measures during antenatal care to counsel women about contraception, reproductive health and consequences of unintended pregnancy.